Predicting, preventing, and managing cardiovascular and chronic kidney disease progression in people with type 2 diabetes: How to improve on traditional strategies
预测、预防与管理2型糖尿病患者的心血管疾病以及慢性肾病的进展:如何改进传统治疗策略
Patients with hypertension and impaired fasting or impaired glucose tolerance are at substantial risk at developing both micro- and macrovascular cardiovascular disease long before the clinical diagnosis of type 2 diabetes (T2D).1 The vascular risk of diabetes is exaggerated if there is any degree of renal impairment or presence of albuminuria.2 There is substantial concern that with the aging of the US population and increasing obesity, the number of people with either impaired fasting glucose or impaired glucose tolerance will contribute to an epidemic of cardiovascular and kidney disease in the near future. Both epidemiological and clinical studies have demonstrated the benefit of multimodal intensive traditional risk factor modification on both micro- and macrovascular events.3 This has raised important questions about optimal targets for blood pressure, HbA1c and low-density lipoprotein cholesterol (LDL-C) levels, because there is a continuous relationship between these levels and the risk for cardiovascular events. However, it is necessary to look beyond epidemiology, and evaluate the effects of risk factor modification on cardiovascular events. Moreover, traditional treatment approaches have focused largely on the reduction of major atherosclerotic cardiovascular events (ie, major adverse cardiac events [MACE])). What is not well described is the effect of intensive risk factor modification and different medications on the risk for development of congestive heart failure. This is now being assessed more carefully in clinical trials.
Numerous studies, including Action to Control Cardiovascular Risk in Diabetes (ACCORD), Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE), and Veterans Administration Diabetes Trial (VADT), have demonstrated the importance of reducing HbA1c to less than 7% in order to reduce micro- and macrovascular complications in patients with T2D.4 Many experts have suggested that lower goals of HbA1c may be considered for individuals without clinically evident cardiovascular disease, or those with a shorter duration of diabetes or a longer life expectancy. However, the benefits for more intensive glycemic control (below 7.0% HbA1c) have been more difficult to demonstrate on macrovascular events without longer-term follow-up of ≥10 years.4, 5 Thus, HbA1c targets need to be carefully individualized to balance the benefit of lower goals with potential side effects such as hypoglycemia.
1 BLOOD PRESSURE
Blood pressure goals are traditionally set at 140/90 mm Hg simply because there was no available data to justify a lower treatment goal. However, the completion of the systolic blood pressure intervention trial (SPRINT) study, provided evidence that blood pressure targets below 130/80 mm Hg may provide important benefits in reducing cardiovascular events.5, 6 Although the SPRINT study excluded people with diabetes, subset analyses of patients with prediabetes demonstrated a similar benefit on cardiovascular outcomes as for those without prediabetes.7 Many have questioned the observations of the SPRINT trial relative to the ACCORD study, which did not demonstrate a benefit of a lower blood pressure goal on cardiovascular outcomes, except for an important reduction in the risk for stroke.7 However, the results of the ACCORD study on intensive blood pressure reduction may have been confounded, in part, by the intensive glucose-lowering efforts (which were also a part of the study). A recent secondary analysis of ACCORD data demonstrated that, in the standard glycemic control group, the lower blood pressure goal did positively reduce the risk for cardiovascular events.8
There are no randomized controlled trials demonstrating the utility of lower blood pressure goals on renal disease progression. However, there are many secondary analyses from clinical trials in people with T2D and chronic kidney disease (CKD) demonstrating the benefit of lower blood pressure goals on the risk of development of doubling of serum creatinine end-stage renal disease or death.9, 10 Moreover, there is abundant literature indicating that patients with proteinuria benefit from renin-angiotensin system (RAS) blockade and lower blood pressure goal.11 As with HbA1c targets, blood pressure targets need to carefully individualized, and lower goals are recommended for people with more cardiovascular risk.
2 LIPID GOALS
The benefits of aggressive LDL-C lowering has been well demonstrated in people with T2D.12 More recent guidelines have suggested that all patients with diabetes should receive lipid-lowering therapy to provide a 40% reduction in LDL-C from prior baseline.13 Similarly, with the completion of the SHARP trial in patients with CKD there is important evidence, especially in people with non-dialysis-dependent CKD, that lipid-lowering therapy can reduce cardiovascular events.14 Thus, it is recommended that all patients with CKD, like those with diabetes, receive lipid-lowering therapy. Thus, there is a movement away from the threshold-based treatment to consider cardiovascular risk factor-based treatment with regard to lipid lowering.
3 NEW OPPORTUNITIES
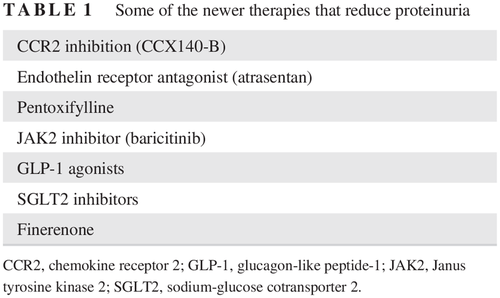
The benefits of RAS inhibition coupled with more intensive targets for blood pressure, cholesterol, and glucose are well demonstrated in the literature for reducing cardiovascular events.3 However, there is much need for improvement. As a consequence, therapeutic strategies are being developed to target atherosclerosis anti-inflammatory therapies. Some of the new anti-inflammatory approaches include chemokine receptor 2 inhibition, endothelin receptor antagonism, Janus tyrosine kinase (JAK) 2 inhibition, pentoxyfyline, and mineralocorticoid receptor antagonists (Table 1).16-19
| CCR2 inhibition (CCX140-B) |
| Endothelin receptor antagonist (atrasentan) |
| Pentoxifylline |
| JAK2 inhibitor (baricitinib) |
| GLP-1 agonists |
| SGLT2 inhibitors |
| Finerenone |
- CCR2, chemokine receptor 2; GLP-1, glucagon-like peptide-1; JAK2, Janus tyrosine kinase 2; SGLT2, sodium-glucose cotransporter 2.
In the past few years, serendipitous observations demonstrating improved cardiovascular and renal outcomes in patients receiving sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide-1 (GLP-1) agonists have been observed in cardiovascular outcome trials that were designed to assess the safety of these drugs.20-22 The potential benefits of these drugs do not appear to be related to glucose lowering, but may be related to a number of different possible factors, including blood pressure reduction, weight reduction, changes in substrate use for energy metabolism and even inhibition of the sodium-hydrogen exchange at a tissue level (Table 2).23 Some have theorized the modest natriuresis associated with SGLT2 inhibitors may alter glomerular hemodynamics in a favorable manner to reduce proteinuria.24 However, these latter observations have been conducted in healthy hyperfiltering diabetics and not in patients with more advanced CKD.
| Blood pressure reduction |
| Glomerular capillary pressure reduction |
| Weight loss |
| Improved metabolic substrate use |
| Reduction in vascular stiffness |
| Proteinuria reduction |
| Inhibition of NHE1 and NHE3 in the heart or vasculature and kidney, respectively |
- NHE, Na+/H+ exchanger.
4 CONCLUSIONS
Efforts to reduce cardiovascular and renal disease progression in people with impaired glycemic control or diagnosed diabetes have come a long way in the past few years. Newer data suggesting more intensive targets for blood pressure, LDL-C, and glycemic control in conjunction with multimodal risk factor modification may have substantial benefits in reducing the risk of cardiovascular events. However, newer opportunities may improve upon traditional methodologies for reducing cardiovascular and renal events. Serendipitous observations with the SGLT2 inhibitors and GLP-1 agonists may assist in unlocking more understanding about the pathophysiology of vascular disease in these patients, and optimize treatment. Moreover, efforts to specifically antagonize vascular inflammation may provide important benefit in future clinical trials.
合并高血压与空腹血糖受损或者糖耐量受损的患者发生微血管与大血管心血管疾病的风险都很大,但这早在他们被临床上诊断为2型糖尿病(T2D)之前已经发生1。如果已经合并任何程度的肾损害或者蛋白尿,那么糖尿病患者的血管风险就会进一步增大2。人们普遍担心,随着美国人口的老龄化以及肥胖患者的增加,合并空腹血糖受损或者糖耐量受损的患者人数很快将会导致心血管疾病与肾脏疾病的流行。流行病学与临床研究已经证实了多种模式的强化治疗矫正传统的危险因素后对微血管以及大血管事件都有益处3。因此出现了一个重要的问题,那就是血压、HbA1c以及低密度脂蛋白胆固醇(LDL-C)的最佳目标是什么,因为这些指标的控制水平与心血管事件风险之间持续相关。然而,我们必须超越流行病学,评估矫正危险因素后对心血管事件有何影响。此外,传统的治疗方法大部分都聚焦于要减少主要动脉粥样硬化性心血管事件(亦即主要不良心脏事件[MACE])。目前尚未明确的是,强化治疗矫正危险因素以及不同的药物对充血性心力衰竭的发生风险有何影响。目前正在临床试验中更仔细地评估这一点。
许多研究,包括控制糖尿病心血管风险行动(Action to Control Cardiovascular Risk in Diabetes,ACCORD)、控制糖尿病与血管疾病行动:百普乐与达美康缓释片对照评估试验(Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation,ADVANCE)以及退伍军人管理局糖尿病试验(Veterans Administration Diabetes Trial,VADT),都已经证实了为了减少T2D患者的微血管与大血管并发症需要将HbA1c降低到小于7%的重要性4。许多专家建议,对于临床上没有明显心血管疾病的患者,或者是糖尿病病程较短或者预期寿命较长的患者,可以考虑将HbA1c降低到更低的目标水平。然而,如果不进行10年以上的长期随访,很难证明进一步的强化血糖控制(HbA1c低于7.0%)对大血管事件有益处4,5。因此,为了平衡更低目标水平的益处与潜在副作用(如低血糖)之间的关系,需要仔细地制定个性化的HbA1c目标。
1 血压
传统上将血压目标简单地设定为140/90 mmHg,因为目前还没有可用的数据来证明更低的治疗目标是合理的。然而,随着收缩压干预试验(systolic blood pressure intervention trial, SPRINT)研究的完成,它所提供的证据表明,血压目标低于130/80 mmHg明显有益于减少心血管事件5,6。虽然SPRINT研究将糖尿病患者排除在外,但是糖尿病前期患者的亚组分析结果表明,与那些非糖尿病前期患者相比,血压目标低于130/80 mmHg对心血管结果的益处也相似7。许多人在质疑SPRINT试验的观察结果, 它与ACCORD研究相似,而后者没有证实更低的血压目标对心血管结果有益处,除了中风的风险有显著下降以外7。然而,ACCORD研究中的强化降压治疗结果有可能在某种程度上受到了强化降糖治疗结果(这也是这项研究的一部分)的影响。最近对ACCORD研究数据进行二次分析后发现,在标准血糖控制组中,更低的血压控制目标确实对减少心血管事件的风险有积极的影响8。
目前还没有随机对照试验证明更低的血压目标对肾脏疾病进展有影响。然而,目前已经有许多来自于T2D与慢性肾脏病患者临床试验的二次分析,结果表明更低的血压目标对血清肌酐倍增、进展为终末期肾病或者死亡风险都有益9,10。此外,大量文献表明蛋白尿患者可以从肾素-血管紧张素系统的阻断以及更低的血压目标中获益11。就像制定HbA1c目标一样,需要仔细地制定个体化的血压目标,推荐具有更高心血管风险的患者采用更低的血压控制目标。
2 血脂目标
积极降低LDL-C水平的益处目前已经在T2D患者中得到了充分证实12。最近的指南都建议所有的糖尿病患者都应该接受降脂治疗,目标是LDL-C水平从既往的基线水平降低40%13。同样,随着在CKD患者中进行的SHARP试验的完成,有重要证据表明,特别是在不依赖透析的CKD患者中,降脂治疗可以减少心血管事件14。因此,建议所有的CKD患者,就像糖尿病患者一样,都要接受降脂治疗。所以,降脂治疗的趋势已经从基于阈值的治疗转变为基于心血管危险因素的治疗。
3 新的治疗方法
众多减少心血管事件的文献都已经充分证实了抑制RAS以及同时达到更严格的血压、胆固醇以及血糖强化治疗目标的益处3。然而,还有许多需要改进的地方。因此,目前正在制定针对动脉粥样硬化抗炎疗法的治疗策略。目前已经有一些新的抗炎方法,包括趋化因子受体2抑制剂、内皮素受体拮抗剂、Janus酪氨酸激酶(JAK)2抑制剂、己酮可可碱以及盐皮质激素受体拮抗剂16-19。过去的几年里,在设计用于评估钠-葡萄糖共转运体2(SGLT2)抑制剂与胰高血糖素样肽-1(GLP-1)激动剂安全性的心血管结果试验中,意外观察到的结果表明,接受这些药物治疗的患者心血管以及肾脏结果都有所改善20-22。这些药物的潜在益处看起来似乎与降糖无关,但是可能与许多不同的可能存在的因素有关,包括血压降低、体重减轻、能量代谢中的底物使用变化,甚至包括在组织水平上抑制钠-氢交换23。一些理论认为,与SGLT2抑制剂相关的中度尿钠增多可能有利于改善肾小球的血流动力学并且减少蛋白尿24。然而,后面这些结果是在相对健康的高滤过糖尿病患者中观察到的,并不是在更严重的CKD患者中看到的。
4 结论
在过去的几年中,我们在不断地努力以延缓血糖控制受损或者确诊糖尿病患者的心血管疾病以及肾脏疾病的进展,目前已经取得了很大进展。新近数据表明,将血压、LDL-C以及血糖都控制在更为严格的目标下,加上矫正多种其他危险因素,这样做可能对减少心血管事件的风险有显著的益处。然而,一些较新的机遇相对于传统的治疗方法可能更有利于减少心血管与肾脏事件。偶然观察到的SGLT2抑制剂与GLP-1激动剂的相关结果可能有助于我们进一步了解糖尿病患者合并血管疾病的病理生理学,并有助于我们优化治疗方案。此外,在未来的临床试验中,特别针对血管炎症的治疗可能会带来明显的获益。
ACKNOWLEDGEMENTS
This paper did not receive any specific funding received. The author has received grants from the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK066013, U01DK116095, and U01DK106102) and National Heart, Lung, and Blood Institute (R01HL127422 and R01HL132732).
DISCLOSURE
The author has acted as a scientific advisor to Janssen, Astra, boehringer-ingelheim, merck sharp and dohme, Akebia, Relypsa, Boston Scientific, Lexicon, Bayer, Vifor, and CareDx.