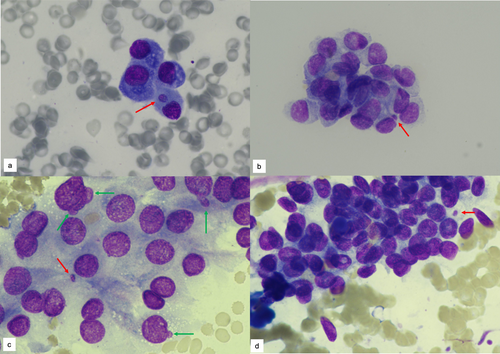
Micronucleus and Nuclear Budding Help to Identify Malignancy in Thyroid Fine Needle Aspiration Cytology
Funding: The authors received no specific funding for this work.
This study has been previously presented at 32nd National Pathology Congress in October 2023, in Antalya, Türkiye. There is no plagiarism in our paper.
ABSTRACT
Objective
Micronucleus (MN) and Nuclear Budding (NB) Have Been Used as an Important Stimulus for Nuclear Atypia in Revealing Chromosomal Damage and Cancer Risk. This Study Aims to Assess MN and NB as Nuclear Parameters and Explore Their Role in Differential Diagnosis of Thyroid FNA and “Bethesda System for Reporting Thyroid Cytology” (BSRTC).
Methods
The Study Included 350 Thyroid FNA Samples Categorised According to BSRTC. NB And MN Were Evaluated in 1000 Thyrocytes on FNA Slides. The Thyroidectomy Sections Were Divided Into Three Categories as ‘Malignant’, ‘Low-Risk’ and ‘Benign’.
Results
A Total of 350 Cases Were Classified as follows: 55 (15.71%) Benign, 159 (45.43%) Atypia of Undetermined Significance (AUS), 20 (5.71%) Follicular Neoplasm (FN), 48 (13.71%) Suspicious for Malignancy (SFM) and 68 (19.43%) Malignant. In comparison to all other cytopathologic diagnostic groups, the benign group had significantly lower levels of MN and NB (p < 0.001). The AUS group's MN and NB counts were significantly lower than those of the FN, SFM and malignant groups (MN for AUS-FN/SFM/M p < 0.001, NB for AUS-FN p = 0.01, NB for AUS-SFM/M p < 0.001, respectively). MN and NB counts were greater in the AUS group for cases with a malignant histopathologic diagnosis than for those with a benign histopathologic diagnosis (p < 0.001). MN and NB cut-off values > 5.50 and > 14.50, respectively, suggest high sensitivity and specificity of malignancy.
Conclusions
Increased Frequency of MN and NB closely associated with an increased risk of malignancy in thyroid FNA. Assessing MN and NB in thyroid FNA may help better stratify the risk in the AUS category.
Graphical Abstract
Increased frequency of micronucleus (MN) (red arrows) and nuclear budding (NB) (green arrows) closely associated with an increased risk of malignancy in thyroid FNA. The benign group have lower levels of MN and NB than other cytologic categories. MN and NB counts are greater in the AUS group for cases with a malignant histopathologic diagnosis than for those with a benign histopathologic diagnosis.
Conflicts of Interest
The authors decalre no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.