Renal effects and safety between Asian and non-Asian chronic kidney disease and type 2 diabetes treated with nonsteroidal mineralocorticoid antagonists
Xiaoming Xu
Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Search for more papers by this authorJing Feng
Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Search for more papers by this authorYuying Cui
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan, China
Search for more papers by this authorPingjiang Li
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Shandong First Medical University and Shandong Academy of Medical Sciences, Jinan, China
Search for more papers by this authorCorresponding Author
Jianjun Dong
Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, China
Correspondence
Lin Liao, Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Shandong Key Laboratory of Rheumatic Disease and Translational Medicine, Shandong Institute of Nephrology, Jinan, 250014, China.
Email: [email protected]
Jianjun Dong, Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, 250012, China.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Lin Liao
Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Correspondence
Lin Liao, Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Shandong Key Laboratory of Rheumatic Disease and Translational Medicine, Shandong Institute of Nephrology, Jinan, 250014, China.
Email: [email protected]
Jianjun Dong, Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, 250012, China.
Email: [email protected]
Search for more papers by this authorXiaoming Xu
Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Search for more papers by this authorJing Feng
Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Search for more papers by this authorYuying Cui
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan, China
Search for more papers by this authorPingjiang Li
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Shandong First Medical University and Shandong Academy of Medical Sciences, Jinan, China
Search for more papers by this authorCorresponding Author
Jianjun Dong
Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, China
Correspondence
Lin Liao, Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Shandong Key Laboratory of Rheumatic Disease and Translational Medicine, Shandong Institute of Nephrology, Jinan, 250014, China.
Email: [email protected]
Jianjun Dong, Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, 250012, China.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Lin Liao
Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Department of Endocrinology and Metabology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China
Correspondence
Lin Liao, Department of Endocrinology and Metabology, Shandong Provincial Qianfoshan Hospital, Shandong University, Shandong Key Laboratory of Rheumatic Disease and Translational Medicine, Shandong Institute of Nephrology, Jinan, 250014, China.
Email: [email protected]
Jianjun Dong, Department of Endocrinology, Qilu Hospital of Shandong University, Jinan, 250012, China.
Email: [email protected]
Search for more papers by this authorAbstract
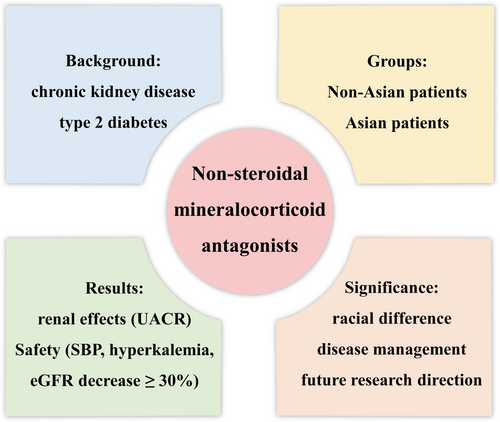
Background
Asians bear a heavier burden of chronic kidney disease (CKD), a common comorbidity of type 2 diabetes mellitus (T2DM), than non-Asians. Nonsteroidal mineralocorticoid receptor antagonists (MRAs) have garnered attention for their potential advantages in renal outcomes. Nevertheless, the impact on diverse ethnic groups remains unknown.
Methods
The PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang database, and clinical trial registries were searched through August 2023 with the following keywords: nonsteroidal MRAs (finerenone, apararenone, esaxerenone, AZD9977, KBP-5074), CKD, T2DM, and randomized controlled trial (RCT). A random effects model was used to calculate overall effect sizes.
Results
Seven RCTs with 14 997 participants were enrolled. Nonsteroidal MRAs reduced urinary albumin to creatinine ratio (UACR) significantly more in Asians than non-Asians: (weighted mean difference [WMD], −0.59, 95% CI, −0.73 to −0.45, p < .01) vs (WMD, −0.29, 95% CI, −0.32 to −0.27, p < .01), respectively. The average decline of estimated glomerular filtration rate (eGFR) was similar in Asians and non-Asians (p > .05). Regarding systolic blood pressure (SBP), nonsteroidal MRAs had a better antihypertension performance in Asians (WMD, −5.12, 95% CI, −5.84 to −4.41, p < .01) compared to non-Asians (WMD, −3.64, 95% CI, −4.38 to −2.89, p < .01). A higher incidence of hyperkalemia and eGFR decrease ≥30% was found in Asians than non-Asians (p < .01).
Conclusions
Nonsteroidal MRAs exhibited significant renal benefits by decreasing UACR and lowering SBP in Asian than that of non-Asian patients with CKD and T2DM, without increase of adverse events except hyperkalemia and eGFR decrease ≥30%.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supporting Information
| Filename | Description |
|---|---|
| jdb13566-sup-0001-FigureS1.tifTIFF image, 7.4 MB | Figure S1. GRADE approach to assess the overall confidence for urinary albumin to creatinine ratio (UACR). GRADE, Grading of Recommendations Assessment, Development and Evaluation; MRA, mineralocorticoid antagonist. |
| jdb13566-sup-0002-FigureS2.tifTIFF image, 7.5 MB | Figure S2. GRADE approach to assess the overall confidence for estimated glomerular filtration rate (eGFR). GRADE, Grading of Recommendations Assessment, Development and Evaluation; MRA, mineralocorticoid antagonist. |
| jdb13566-sup-0003-FigureS3.tifTIFF image, 6.7 MB | Figure S3. GRADE approach to assess the overall confidence for systolic blood pressure (SBP). GRADE, Grading of Recommendations Assessment, Development and Evaluation; MRA, mineralocorticoid antagonist. |
| jdb13566-sup-0004-FigureS4.tifTIFF image, 7.9 MB | Figure S4. GRADE approach to assess the overall confidence for hyperkalemia. GRADE, Grading of Recommendations Assessment, Development and Evaluation; MRA, mineralocorticoid antagonist. |
| jdb13566-sup-0005-FigureS5.tifTIFF image, 7.9 MB | Figure S5. GRADE approach to assess the overall confidence for estimated glomerular filtration rate (eGFR) decrease ≥ 30%. GRADE, Grading of Recommendations Assessment, Development and Evaluation; MRA, mineralocorticoid antagonist. |
| jdb13566-sup-0006-FigureS6.tifTIFF image, 7.9 MB | Figure S6. GRADE approach to assess the overall confidence for total adverse events. GRADE, Grading of Recommendations Assessment, Development and Evaluation; MRA, mineralocorticoid antagonist. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001; 414(6865): 782-787. doi:10.1038/414782a
- 2Ke C, Narayan KMV, Chan JCN, Jha P, Shah BR. Pathophysiology, phenotypes and management of type 2 diabetes mellitus in Indian and Chinese populations. Nat Rev Endocrinol. 2022; 18(7): 413-432. doi:10.1038/s41574-022-00669-4
- 3Magliano DJ, Boyko EJ. IDF diabetes Atlas 10th edition scientific committee. IDF Diabetes Atlas. 10th ed. International Diabetes Federation; 2021. http://www.ncbi.nlm.nih.gov/books/NBK581934/
- 4 GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2020; 395(10225): 709-733. doi:10.1016/S0140-6736(20)30045-3
- 5Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS One. 2016; 11(7):e0158765. doi:10.1371/journal.pone.0158765
- 6Afkarian M, Zelnick LR, Hall YN, et al. Clinical manifestations of kidney disease among US adults with diabetes, 1988-2014. JAMA. 2016; 316(6): 602-610. doi:10.1001/jama.2016.10924
- 7Jaisser F, Farman N. Emerging roles of the mineralocorticoid receptor in pathology: toward new paradigms in clinical pharmacology. Pharmacol Rev. 2016; 68(1): 49-75. doi:10.1124/pr.115.011106
- 8Barrera-Chimal J, Girerd S, Jaisser F. Mineralocorticoid receptor antagonists and kidney diseases: pathophysiological basis. Kidney Int. 2019; 96(2): 302-319. doi:10.1016/j.kint.2019.02.030
- 9Kintscher U, Bakris GL, Kolkhof P. Novel non-steroidal mineralocorticoid receptor antagonists in cardiorenal disease. Br J Pharmacol. 2022; 179(13): 3220-3234. doi:10.1111/bph.15747
- 10Pitt B, Filippatos G, Agarwal R, et al. Cardiovascular events with Finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021; 385(24): 2252-2263. doi:10.1056/NEJMoa2110956
- 11Bakris GL, Agarwal R, Anker SD, et al. Effect of Finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020; 383(23): 2219-2229. doi:10.1056/NEJMoa2025845
- 12Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. 2022; 43(6): 474-484. doi:10.1093/eurheartj/ehab777
- 13Chen Q, Liang Y, Yan J, et al. Efficacy and safety of non-steroidal mineralocorticoid receptor antagonists for renal outcomes: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2023; 195:110210. doi:10.1016/j.diabres.2022.110210
- 14Filippatos G, Anker SD, Pitt B, et al. Finerenone and heart failure outcomes by kidney function/albuminuria in chronic kidney disease and diabetes. JACC Heart Failure. 2022; 10(11): 860-870. doi:10.1016/j.jchf.2022.07.013
- 15Lerma E, White WB, Bakris G. Effectiveness of nonsteroidal mineralocorticoid receptor antagonists in patients with diabetic kidney disease. Postgrad Med. 2023; 135(3): 224-233. doi:10.1080/00325481.2022.2060598
- 16Yang S, Shen W, Zhang HZ, Wang CX, Yu WQ, Wu QH. Efficacy and safety of Finerenone for prevention of cardiovascular events in type 2 diabetes mellitus with chronic kidney disease: a meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol. 2023; 81(1): 55-62. doi:10.1097/FJC.0000000000001364
- 17Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4(1): 1. doi:10.1186/2046-4053-4-1
- 18Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019; 10(10):ED000142. doi:10.1002/14651858.ED000142
- 19Ito S, Kashihara N, Shikata K, et al. Esaxerenone (CS-3150) in patients with type 2 diabetes and microalbuminuria (ESAX-DN): phase 3 randomized controlled clinical trial. Clin J Am Soc Nephrol. 2020; 15(12): 1715-1727. doi:10.2215/CJN.06870520
- 20Wada T, Inagaki M, Yoshinari T, et al. Apararenone in patients with diabetic nephropathy: results of a randomized, double-blind, placebo-controlled phase 2 dose-response study and open-label extension study. Clin Exp Nephrol. 2021; 25(2): 120-130. doi:10.1007/s10157-020-01963-z
- 21Katayama S, Yamada D, Nakayama M, et al. A randomized controlled study of finerenone versus placebo in Japanese patients with type 2 diabetes mellitus and diabetic nephropathy. J Diabetes Complications. 2017; 31(4): 758-765. doi:10.1016/j.jdiacomp.2016.11.021
- 22Bakris GL, Agarwal R, Chan JC, et al. Effect of Finerenone on albuminuria in patients with diabetic nephropathy: a randomized clinical trial. JAMA. 2015; 314(9): 884-894. doi:10.1001/jama.2015.10081
- 23Bakris G, Pergola PE, Delgado B, et al. Effect of KBP-5074 on blood pressure in advanced chronic kidney disease: results of the BLOCK-CKD study. Hypertension. 2021; 78(1): 74-81. doi:10.1161/HYPERTENSIONAHA.121.17073
- 24Selby NM, Taal MW. An updated overview of diabetic nephropathy: diagnosis, prognosis, treatment goals and latest guidelines. Diabetes Obes Metab. 2020; 22(Suppl 1): 3-15. doi:10.1111/dom.14007
- 25Skolnik NS, Style AJ. Importance of early screening and diagnosis of chronic kidney disease in patients with type 2 diabetes. Diabetes Ther. 2021; 12(6): 1613-1630. doi:10.1007/s13300-021-01050-w
- 26Hené RJ, Boer P, Koomans HA, Mees EJ. Plasma aldosterone concentrations in chronic renal disease. Kidney Int. 1982; 21(1): 98-101. doi:10.1038/ki.1982.14
- 27Schjoedt KJ, Andersen S, Rossing P, Tarnow L, Parving HH. Aldosterone escape during blockade of the renin-angiotensin-aldosterone system in diabetic nephropathy is associated with enhanced decline in glomerular filtration rate. Diabetologia. 2004; 47(11): 1936-1939. doi:10.1007/s00125-004-1542-0
- 28Cicoira M, Zanolla L, Rossi A, et al. Failure of aldosterone suppression despite angiotensin-converting enzyme (ACE) inhibitor administration in chronic heart failure is associated with ACE DD genotype. J Am Coll Cardiol. 2001; 37(7): 1808-1812. doi:10.1016/s0735-1097(01)01237-2
- 29Khurana N, James S, Coughlan MT, MacIsaac RJ, Ekinci EI. Novel therapies for kidney disease in people with diabetes. J Clin Endocrinol Metab. 2022; 107(1): e1-e24. doi:10.1210/clinem/dgab639
- 30Bauersachs J, Jaisser F, Toto R. Mineralocorticoid receptor activation and mineralocorticoid receptor antagonist treatment in cardiac and renal diseases. Hypertension. 2015; 65(2): 257-263. doi:10.1161/HYPERTENSIONAHA.114.04488
- 31Kolkhof P, Jaisser F, Kim SY, Filippatos G, Nowack C, Pitt B. Steroidal and novel non-steroidal mineralocorticoid receptor antagonists in heart failure and cardiorenal diseases: comparison at bench and bedside. Handb Exp Pharmacol. 2017; 243: 271-305. doi:10.1007/164_2016_76
- 32Barrera-Chimal J, Gerarduzzi C, Rossignol P, Jaisser F. The non-steroidal mineralocorticoid receptor antagonist finerenone is a novel therapeutic option for patients with type 2 diabetes and chronic kidney disease. Clin Sci. 2022; 136(12): 1005-1017. doi:10.1042/CS20220212
- 33Savarese G, Lindberg F, Filippatos G, Butler J, Anker SD. Mineralocorticoid receptor overactivation: targeting systemic impact with non-steroidal mineralocorticoid receptor antagonists. Diabetologia. 2024; 67(2): 246-262. doi:10.1007/s00125-023-06031-1
- 34Kolkhof P, Bärfacker L. 30 Years of the mineralocorticoid receptor: Mineralocorticoid receptor antagonists: 60 years of research and development. J Endocrinol. 2017; 234(1): T125-T140. doi:10.1530/JOE-16-0600
- 35Agarwal R, Kolkhof P, Bakris G, et al. Steroidal and non-steroidal mineralocorticoid receptor antagonists in cardiorenal medicine. Eur Heart J. 2021; 42(2): 152-161. doi:10.1093/eurheartj/ehaa736
- 36Vardeny O, Cavallari LH, Claggett B, et al. Race influences the safety and efficacy of spironolactone in severe heart failure. Circ Heart Fail. 2013; 6(5): 970-976. doi:10.1161/CIRCHEARTFAILURE.113.000530
- 37Collard D, Brouwer TF, Olde Engberink RHG, Zwinderman AH, Vogt L, van den Born BJH. Initial estimated glomerular filtration rate decline and long-term renal function during intensive antihypertensive therapy: a post hoc analysis of the SPRINT and ACCORD-BP randomized controlled trials. Hypertension. 2020; 75(5): 1205-1212. doi:10.1161/HYPERTENSIONAHA.119.14659
- 38Shikata K, Ito S, Kashihara N, et al. Reduction in the magnitude of serum potassium elevation in combination therapy with esaxerenone (CS-3150) and sodium-glucose cotransporter 2 inhibitor in patients with diabetic kidney disease: subanalysis of two phase III studies. J Diabetes Invest. 2022; 13(7): 1190-1202. doi:10.1111/jdi.13778
- 39Kotchen TA, Cowley AW, Frohlich ED. Salt in health and disease—a delicate balance. N Engl J Med. 2013; 368(13): 1229-1237. doi:10.1056/NEJMra1212606
- 40Khor BH, Komnenov D, Rossi NF. Impact of dietary fructose and high salt diet: are preclinical studies relevant to Asian societies? Nutrients. 2022; 14(12): 2515. doi:10.3390/nu14122515
- 41Shibata S, Mu S, Kawarazaki H, et al. Rac1 GTPase in rodent kidneys is essential for salt-sensitive hypertension via a mineralocorticoid receptor-dependent pathway. J Clin Invest. 2011; 121(8): 3233-3243. doi:10.1172/JCI43124
- 42Hirohama D, Kawarazaki W, Nishimoto M, et al. PGI2 analog attenuates salt-induced renal injury through the inhibition of inflammation and Rac1-MR activation. Int J Mol Sci. 2020; 21(12): 4433. doi:10.3390/ijms21124433
- 43Fuller PJ, Yang J, Young MJ. Mechanisms of mineralocorticoid receptor signaling. Vitam Horm. 2019; 109: 37-68. doi:10.1016/bs.vh.2018.09.004
- 44Valinsky WC, Touyz RM, Shrier A. Aldosterone, SGK1, and ion channels in the kidney. Clin Sci. 2018; 132(2): 173-183. doi:10.1042/CS20171525
- 45Bienvenu LA, Reichelt ME, Delbridge LMD, Young MJ. Mineralocorticoid receptors and the heart, multiple cell types and multiple mechanisms: a focus on the cardiomyocyte. Clin Sci. 2013; 125(9): 409-421. doi:10.1042/CS20130050
- 46Cavallari LH, Groo VL, Viana MAG, Dai Y, Patel SR, Stamos TD. Association of aldosterone concentration and mineralocorticoid receptor genotype with potassium response to spironolactone in patients with heart failure. Pharmacotherapy. 2010; 30(1): 1-9. doi:10.1592/phco.30.1.1
- 47Dumeny L, Vardeny O, Edelmann F, Pieske B, Duarte JD, Cavallari LH. NR3C2 genotype is associated with response to spironolactone in diastolic heart failure patients from the Aldo-DHF trial. Pharmacotherapy. 2021; 41(12): 978-987. doi:10.1002/phar.2626
- 48Chan JCN, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009; 301(20): 2129-2140. doi:10.1001/jama.2009.726
- 49Bomback AS, Klemmer PJ. The incidence and implications of aldosterone breakthrough. Nat Clin Pract Nephrol. 2007; 3(9): 486-492. doi:10.1038/ncpneph0575