Recent drug development of dorzagliatin, a new glucokinase activator, with the potential to treat Type 2 diabetes: A review study
Yu Jiang
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorLuyao Wang
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorZhenhua Dong
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorBaotian Xia
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorCorresponding Author
Shuguang Pang
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Correspondence
Shuguang Pang, School of Clinical Medicine, Shandong Second Medical University, Weifang 261000, Shandong, China, Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, 105 Jiefang Road, Jinan, 250000, China.
Email: [email protected]
Search for more papers by this authorYu Jiang
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorLuyao Wang
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorZhenhua Dong
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorBaotian Xia
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Search for more papers by this authorCorresponding Author
Shuguang Pang
School of Clinical Medicine, Shandong Second Medical University, Weifang, China
Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, China
Correspondence
Shuguang Pang, School of Clinical Medicine, Shandong Second Medical University, Weifang 261000, Shandong, China, Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, 105 Jiefang Road, Jinan, 250000, China.
Email: [email protected]
Search for more papers by this authorAbstract
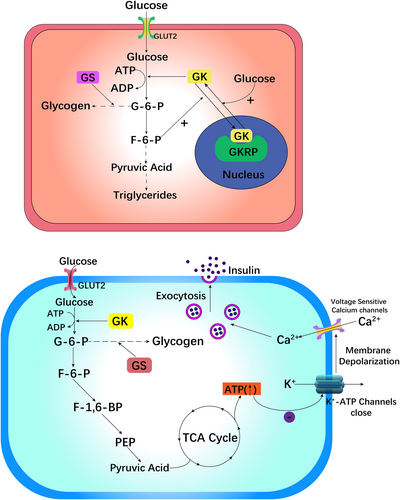
Type 2 diabetes mellitus (T2DM) is a complicated disease related to metabolism that results from resistance to insulin and sustained hyperglycemia. Traditional antidiabetic drugs cannot meet the demand of different diabetes patients for reaching the glycemic targets; thus, the identification of new antidiabetic drugs is urgently needed for the treatment of T2DM to enhance glycemic control and the prognosis of patients suffering from T2DM. Recently, glucokinase (GK) has attracted much attention and is considered to be an effective antidiabetic agent. Glucokinase activators (GKA) represented by dorzagliatin could activate GK and mimic its function that triggers a counter-regulatory response to blood glucose changes. Dorzagliatin has shown great potential for glycemic control in diabetic patients in a randomized, double-blind, placebo-controlled Phase 3 trial (SEED study) and had a favorable safety profile and was well tolerated (DAWN study). In the SEED study, dorzagliatin significantly reduced glycosylated hemoglobin (HbA1c) by 1.07% and postprandial blood glucose by 2.83 mol/L, showing the great potential of this drug to control blood glucose in diabetic patients, with good safety and good tolerance. An extension of the SEED study, the DREAM study, confirmed that dorzagliatin monotherapy significantly improved 24-h glucose variability and increased time in range (TIR) to 83.7% over 46 weeks. Finally, the clinical study of dorzagliatin combined with metformin (DAWN study) confirmed that dorzagliatin could significantly reduce HbA1c by 1.02% and postprandial blood glucose by 5.45 mol/L. The current review summarizes the development of GK and GKA, as well as the prospects, trends, applications, and shortcomings of these treatments, especially future directions of clinical studies of dorzagliatin.
CONFLICT OF INTEREST STATEMENT
No latent conflicts of interest were reported by the authors.
REFERENCES
- 1Egan AM, Laurenti MC, Hurtado Andrade MD, et al. Limitations of the fasting proinsulin to insulin ratio as a measure of β-cell health in people with and without impaired glucose tolerance. Eur J Clin Invest. 2021; 51(6): e13469. doi:10.1111/eci.13469
- 2Schiavon M, Visentin R, Göbel B, et al. Improved postprandial glucose metabolism in type 2 diabetes by the dual glucagon-like peptide-1/glucagon receptor agonist SAR425899 in comparison with liraglutide. Diabetes Obes Metab. 2021; 23(8): 1795-1805. doi:10.1111/dom.14394
- 3Adams JD, Dalla Man C, Laurenti MC, et al. Fasting glucagon concentrations are associated with longitudinal decline of β-cell function in non-diabetic humans. Metabolism. 2020; 105:154175. doi:10.1016/j.metabol.2020.154175
- 4Suga T, Kikuchi O, Kobayashi M, et al. SGLT1 in pancreatic α cells regulates glucagon secretion in mice, possibly explaining the distinct effects of SGLT2 inhibitors on plasma glucagon levels. Mol Metab. 2018; 19: 1-12. doi:10.1016/j.molmet.2018.10.009
- 5Bi Y, Zhu D, Jing Y, et al. Decreased beta cell function and insulin sensitivity contributed to increasing fasting glucose in Chinese. Acta Diabetol. 2012; 49(Suppl 1): S51-S58. doi:10.1007/s00592-010-0194-4
- 6Campbell JE, Newgard CB. Mechanisms controlling pancreatic islet cell function in insulin secretion. Nat Rev Mol Cell Biol. 2021; 22(2): 142-158. doi:10.1038/s41580-020-00317-7
- 7Ogurtsova K, da Rocha Fernandes JD, Huang Y, et al. IDF Diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017; 128: 40-50. doi:10.1016/j.diabres.2017.03.024
- 8Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022; 183:109119. doi:10.1016/j.diabres.2021.109119
- 9ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes—2023. Diabetes Care. 2023; 46(Supplement_1): S140-S157. doi:10.2337/dc23-S009
- 10Di Mario C, Genovese S, Lanza GA, et al. Role of continuous glucose monitoring in diabetic patients at high cardiovascular risk: an expert-based multidisciplinary Delphi consensus. Cardiovasc Diabetol. 2022; 21: 164. doi:10.1186/s12933-022-01598-2
- 11Scheen AJ. New hope for glucokinase activators in type 2 diabetes? Lancet Diabetes Endocrinol. 2018; 6(8): 591-593. doi:10.1016/S2213-8587(18)30133-5
- 12Kahn SE, Montgomery B, Howell W, et al. Importance of Early Phase Insulin Secretion to Intravenous Glucose Tolerance in Subjects with Type 2 Diabetes Mellitus. :6.
- 13Georgakis MK, Harshfield EL, Malik R, et al. Diabetes mellitus, glycemic traits, and cerebrovascular disease. Neurology. 2021; 96(13): e1732-e1742. doi:10.1212/WNL.0000000000011555
- 14Dennis JM, Henley WE, Weedon MN, et al. Sex and BMI Alter the benefits and risks of sulfonylureas and thiazolidinediones in type 2 Diabetes: A framework for evaluating stratification using routine clinical and individual trial data. Diabetes Care. 2018; 41(9): 1844-1853. doi:10.2337/dc18-0344
- 15Wilson JE. Hexokinases. Rev Physiol Biochem Pharmacol. 1995; 126: 65-198. doi:10.1007/BFb0049776
- 16Grossbard L, Schimke RT. Multiple hexokinases of rat tissues. Purification and comparison of soluble forms. J Biol Chem. 1966; 241(15): 3546-3560.
- 17Zapater JL, Lednovich KR, Khan MW, Pusec CM, Layden BT. Hexokinase domain containing Protein-1 in metabolic diseases and beyond. Trends Endocrinol Metab. 2022; 33(1): 72-84. doi:10.1016/j.tem.2021.10.006
- 18Matschinsky FM, Wilson DF. The central role of glucokinase in glucose homeostasis: A perspective 50 years after demonstrating the presence of the enzyme in islets of Langerhans. Front Physiol. 2019; 10: 148. doi:10.3389/fphys.2019.00148
- 19Langer S, Waterstradt R, Hillebrand G, Santer R, Baltrusch S. The novel GCK variant p.Val455Leu associated with hyperinsulinism is susceptible to allosteric activation and is conducive to weight gain and the development of diabetes. Diabetologia. 2021; 64(12): 2687-2700. doi:10.1007/s00125-021-05553-w
- 20Emfinger CH, de Klerk E, Schueler KL, et al. β cell–specific deletion of Zfp148 improves nutrient-stimulated β cell Ca2+ responses. JCI Insight. 2022; 7(10):e154198. doi:10.1172/jci.insight.154198
- 21Matschinsky FM, Magnuson MA, Zelent D, et al. The network of glucokinase-expressing cells in glucose homeostasis and the potential of glucokinase activators for diabetes therapy. Diabetes. 2006; 55(1): 1-12.
- 22Moede T, Leibiger B, Vaca Sanchez P, et al. Glucokinase intrinsically regulates glucose sensing and glucagon secretion in pancreatic alpha cells. Sci Rep. 2020; 10(1): 20145. doi:10.1038/s41598-020-76863-z
- 23Ren Y, Li L, Wan L, Huang Y, Cao S. Glucokinase as an emerging anti-diabetes target and recent progress in the development of its agonists. J Enzyme Inhib Med Chem. 2022; 37(1): 606-615. doi:10.1080/14756366.2021.2025362
- 24Klein KR, Freeman JL, Dunn I, et al. The SimpliciT1 study: a randomized, double-blind, placebo-controlled phase 1b/2 adaptive study of TTP399, a hepatoselective glucokinase activator, for adjunctive treatment of type 1 diabetes. Diabetes Care. 2021; 44(9): 960-968.
- 25Toulis KA, Nirantharakumar K, Pourzitaki C, Barnett AH, Tahrani AA. Glucokinase activators for type 2 Diabetes: challenges and future developments. Drugs. 2020; 80(5): 467-475. doi:10.1007/s40265-020-01278-z
- 26Li W, Zhang X, Sun Y, Liu Z. Recent clinical advances of glucokinase activators in the treatment of diabetes mellitus type 2. Pharmazie. 2020; 75(6): 230-235. doi:10.1691/ph.2020.0409
- 27Walker D, Rao S. The role of glucokinase in the phosphorylation of glucose by rat liver. Biochem J. 1964; 90(2): 360-368. doi:10.1042/bj0900360
- 28Sharma P, Singh S, Sharma N, Singla D, Guarve K, Grewal AS. Targeting human glucokinase for the treatment of type 2 diabetes: an overview of allosteric glucokinase activators. J Diabetes Metab Disord. 2022; 21(1): 1129-1137. doi:10.1007/s40200-022-01019-x
- 29Nakamura A, Omori K, Terauchi Y. Glucokinase activation or inactivation: which will lead to the treatment of type 2 diabetes? Diabetes Obes Metab. 2021; 23(10): 2199-2206. doi:10.1111/dom.14459
- 30Iynedjian PB, Möbius G, Seitz HJ, Wollheim CB, Renold AE. Tissue-specific expression of glucokinase: identification of the gene product in liver and pancreatic islets. Proc Natl Acad Sci U S A. 1986; 83(7): 1998-2001. doi:10.1073/pnas.83.7.1998
- 31Yang ML, Horstman S, Gee R, et al. Citrullination of glucokinase is linked to autoimmune diabetes. Nat Commun. 2022; 13(1): 1870. doi:10.1038/s41467-022-29512-0
- 32Del Guerra S, Lupi R, Marselli L, et al. Functional and molecular defects of pancreatic islets in human type 2 diabetes. Diabetes. 2005; 54(3): 727-735. doi:10.2337/diabetes.54.3.727
- 33Lu B, Kurmi K, Munoz-Gomez M, et al. Impaired β-cell glucokinase as an underlying mechanism in diet-induced diabetes. Dis Model Mech. 2018; 11(6): dmm033316. doi:10.1242/dmm.033316
- 34Shah N, Abdalla MA, Deshmukh H, Sathyapalan T. Therapeutics for type-2 diabetes mellitus: a glance at the recent inclusions and novel agents under development for use in clinical practice. Ther Adv Endocrinol Metab. 2021; 12:20420188211042145. doi:10.1177/20420188211042145
- 35Softic S, Gupta MK, Wang GX, et al. Divergent effects of glucose and fructose on hepatic lipogenesis and insulin signaling. J Clin Invest. 2017; 127(11): 4059-4074. doi:10.1172/JCI94585
- 36Matschinsky FM, Zelent B, Doliba NM, et al. Research and Development of glucokinase activators for Diabetes therapy: theoretical and practical aspects. In: M Schwanstecher, ed. Diabetes – Perspectives in Drug Therapy. Vol 203. Handbook of Experimental Pharmacology. Springer; 2011: 357-401. doi:10.1007/978-3-642-17214-4_15
10.1007/978-3-642-17214-4_15 Google Scholar
- 37Doliba NM, Liu Q, Li C, et al. Inhibition of cholinergic potentiation of insulin secretion from pancreatic islets by chronic elevation of glucose and fatty acids: protection by casein kinase 2 inhibitor. Mol Metab. 2017; 6(10): 1240-1253. doi:10.1016/j.molmet.2017.07.017
- 38Bonadonna RC, Heise T, Arbet-Engels C, et al. Piragliatin (RO4389620), a novel glucokinase activator, lowers plasma glucose both in the postabsorptive state and after a glucose challenge in patients with type 2 diabetes mellitus: a mechanistic study. J Clin Endocrinol Metab. 2010; 95(11): 5028-5036. doi:10.1210/jc.2010-1041
- 39Zhi J, Zhai S. Effects of piragliatin, a glucokinase activator, on fasting and postprandial plasma glucose in patients with type 2 diabetes mellitus. J Clin Pharmacol. 2016; 56(2): 231-238. doi:10.1002/jcph.589
- 40Meininger GE, Scott R, Alba M, et al. Effects of MK-0941, a novel glucokinase activator, on glycemic control in insulin-treated patients with type 2 diabetes. Diabetes Care. 2011; 34(12): 2560-2566. doi:10.2337/dc11-1200
- 41Wilding JPH, Leonsson-Zachrisson M, Wessman C, Johnsson E. Dose-ranging study with the glucokinase activator AZD1656 in patients with type 2 diabetes mellitus on metformin. Diabetes Obes Metab. 2013; 15(8): 750-759. doi:10.1111/dom.12088
- 42Kiyosue A, Hayashi N, Komori H, Leonsson-Zachrisson M, Johnsson E. Dose-ranging study with the glucokinase activator AZD1656 as monotherapy in Japanese patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2013; 15(10): 923-930. doi:10.1111/dom.12100
- 43Amin NB, Aggarwal N, Pall D, et al. Two dose-ranging studies with PF-04937319, a systemic partial activator of glucokinase, as add-on therapy to metformin in adults with type 2 diabetes. Diabetes Obes Metab. 2015; 17(8): 751-759. doi:10.1111/dom.12474
- 44Denney WS, Denham DS, Riggs MR, Amin NB. Glycemic effect and safety of a systemic, partial glucokinase activator, PF-04937319, in patients with type 2 Diabetes mellitus inadequately controlled on metformin-A randomized, crossover, active-controlled study. Clin Pharmacol Drug Dev. 2016; 5(6): 517-527. doi:10.1002/cpdd.261
- 45Katz L, Manamley N, Snyder WJ, et al. AMG 151 (ARRY-403), a novel glucokinase activator, decreases fasting and postprandial glycaemia in patients with type 2 diabetes. Diabetes Obes Metab. 2016; 18(2): 191-195. doi:10.1111/dom.12586
- 46Vella A, Freeman JLR, Dunn I, Keller K, Buse JB, Valcarce C. Targeting hepatic glucokinase to treat diabetes with TTP399, a hepatoselective glucokinase activator. Sci Transl Med. 2019; 11(475): eaau3441. doi:10.1126/scitranslmed.aau3441
- 47Ramanathan V, Vachharajani N, Patel R, Barbhaiya R. GKM- 001, a liver-directed/pancreas-sparing glucokinase modulator (GKM), lowers fasting and post-prandial glucose without hypoglycemia in type 2 diabetic (T2D) patients. Diabetes. 2012; 61: A76.
- 48Zhu D, Li X, Ma J, et al. Dorzagliatin in drug-naïve patients with type 2 diabetes: a randomized, double-blind, placebo-controlled h 3 trial. Nat Med. 2022; 28(5): 965-973. doi:10.1038/s41591-022-01802-6
- 49Yang W, Zhu D, Gan S, et al. Dorzagliatin add-on therapy to metformin in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled phase 3 trial. Nat Med. 2022; 28(5): 974-981. doi:10.1038/s41591-022-01803-5
- 50Xx Z, Dl Z, Xy L, et al. Dorzagliatin (HMS5552), a novel dual-acting glucokinase activator, improves glycaemic control and pancreatic β-cell function in patients with type 2 diabetes: A 28-day treatment study using biomarker-guided patient selection. Diabetes Obes Metab. 2018; 20(9): 2113-2120. doi:10.1111/dom.13338
- 51Zhu D, Gan S, Liu Y, et al. Dorzagliatin monotherapy in Chinese patients with type 2 diabetes: a dose-ranging, randomised, double-blind, placebo-controlled, phase 2 study. Lancet Diabetes Endocrinol. 2018; 6(8): 627-636. doi:10.1016/S2213-8587(18)30105-0
- 52Zhu D, Zhang Y, Chen L. 182-OR: A novel dual-acting glucokinase activator (GKA) Dorzagliatin (HMS5552) achieved primary efficacy endpoint with good safety profiles in T2DM patients after 24 weeks of treatment in a phase III monotherapy trial. Diabetes. 2020; 69(Supplement_1):182-OR. doi:10.2337/db20-182-OR
- 53 Dorzagliatin add-on therapy to metformin in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled phase 3 trial – PubMed. Accessed July 6, 2022 https://pubmed.ncbi.nlm.nih.gov/35551292/
- 54Fonseca VA. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009; 32(Suppl 2): S151-S156. doi:10.2337/dc09-S301
- 55 Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group – PubMed. Accessed July 6, 2022 https://pubmed.ncbi.nlm.nih.gov/10359389/
- 56 The mechanisms of action of metformin – PubMed. Accessed July 6, 2022 https://pubmed.ncbi.nlm.nih.gov/28776086/
- 57Yang W, Weng J. Early therapy for type 2 diabetes in China. Lancet Diabetes Endocrinol. 2014; 2(12): 992-1002. doi:10.1016/S2213-8587(14)70136-6
- 58Zeng J, Gan S, Mi N, et al. Diabetes remission in drug-naïve patients with type 2 diabetes after dorzagliatin treatment: A prospective cohort study. Diabetes Obes Metab. 2023; 25: 2878-2887. doi:10.1111/dom.15179
- 59 117-LB: Glucokinase Activator Dorzagliatin (HMS5552) Regulates GLP-1 Release in T2D Patients and Is Synergistic with Sitagliptin and Empagliflozin in Optimizing Beta-Cell Function | Diabetes | American Diabetes Association. Accessed July 8, 2022 https://diabetesjournals.org/diabetes/article/70/Supplement_1/117-LB/139583/117-LB-Glucokinase-Activator-Dorzagliatin-HMS5552
- 60Yu Y, Yang X, Tong K, et al. Efficacy and safety of dorzagliatin for type 2 diabetes mellitus: A meta-analysis and trial sequential analysis. Front Cardiovasc Med. 2022; 9:1041044. doi:10.3389/fcvm.2022.1041044
- 61Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the Management of Blood Cholesterol: A report of the American College of Cardiology/American Heart Association task Force on clinical practice guidelines. Circulation. 2019; 139(25):e1143. doi:10.1161/CIR.0000000000000625
- 62Packard C, Chapman MJ, Sibartie M, Laufs U, Masana L. Intensive low-density lipoprotein cholesterol lowering in cardiovascular disease prevention: opportunities and challenges. Heart. 2021; 107(17): 1369-1375. doi:10.1136/heartjnl-2020-318760
- 63Ye J, Wu Y, Yang S, et al. The global, regional and national burden of type 2 diabetes mellitus in the past, present and future: a systematic analysis of the global burden of disease study 2019. Front Endocrinol. 2023; 14:1192629. doi:10.3389/fendo.2023.1192629
- 64Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020; 396(10258): 1204-1222. doi:10.1016/S0140-6736(20)30925-9
- 65Ong KL, Stafford LK, McLaughlin SA, et al. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of disease study 2021. Lancet. 2023; 402(10397): 203-234. doi:10.1016/S0140-6736(23)01301-6
- 66Kahn SE, Cooper ME, Del Prato S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 2014; 383(9922): 1068-1083. doi:10.1016/S0140-6736(13)62154-6
- 67Chan JCN, Lim LL, Wareham NJ, et al. The lancet commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2020; 396(10267): 2019-2082. doi:10.1016/S0140-6736(20)32374-6
- 68Squires E, Duber H, Campbell M, et al. Health care spending on Diabetes in the U.S., 1996–2013. Diabetes Care. 2018; 41(7): 1423-1431. doi:10.2337/dc17-1376
- 69Afroz A, Alramadan MJ, Hossain MN, et al. Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: a systematic review. BMC Health Serv Res. 2018; 18(1): 972. doi:10.1186/s12913-018-3772-8
- 70Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. Jama. 2020; 323(9): 863-884. doi:10.1001/jama.2020.0734
- 71 Emerging Risk Factors Collaboration, Sarwar N, Gao P, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010; 375(9733): 2215-2222. doi:10.1016/S0140-6736(10)60484-9
- 72Ibsen DB, Steur M, Imamura F, et al. Replacement of red and processed meat with other food sources of protein and the risk of type 2 Diabetes in European populations: the EPIC-InterAct study. Diabetes Care. 2020; 43(11): 2660-2667. doi:10.2337/dc20-1038
- 73Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international Diabetes federation Diabetes atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843. doi:10.1016/j.diabres.2019.107843
- 74Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020; 41(2): 255-323. doi:10.1093/eurheartj/ehz486
- 75 American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment. Diabetes Care. 2017; 40(Supplement_1): S64-S74. doi:10.2337/dc17-S011
- 76Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK prospective Diabetes study (UKPDS) group. Jama. 1999; 281(21): 2005-2012. doi:10.1001/jama.281.21.2005
- 77Frias JP, Gonzalez-Galvez G, Johnsson E, et al. Efficacy and safety of dual add-on therapy with dapagliflozin plus saxagliptin versus glimepiride in patients with poorly controlled type 2 diabetes on a stable dose of metformin: results from a 52-week, randomized, active-controlled trial. Diabetes Obes Metab. 2020; 22(7): 1083-1093. doi:10.1111/dom.13997
- 78 RISE Consortium. Lack of durable improvements in β-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 Diabetes. Diabetes Care. 2019; 42(9): 1742-1751. doi:10.2337/dc19-0556
- 79Nakamura A, Terauchi Y. Present status of clinical deployment of glucokinase activators. J Diabetes Investig. 2015; 6(2): 124-132. doi:10.1111/jdi.12294
- 80Riddle MC, Cefalu WT, Evans PH, et al. Consensus report: definition and interpretation of remission in type 2 Diabetes. Diabetes Care. 2021; 44(10): 2438-2444. doi:10.2337/dci21-0034
- 81Chen L, Zhang J, Yang R, Feng L, Medicine H. 117-LB: glucokinase activator Dorzagliatin (HMS5552) regulates GLP-1 release in T2D patients and is synergistic with sitagliptin and empagliflozin in optimizing Beta-cell function. Diabetes. 2021; 70:117-LB. doi:10.2337/db21-117-LB
- 82Zeng J, Gan S, Dong X, et al. 115-LB: Dorzagliatin showed sustained remission in an observational study after discontinuation of treatment in T2D patients who achieved good glycemic control with Dorzagliatin monotherapy. Diabetes. 2022; 71(Supplement_1): 115-LB. doi:10.2337/db22-115-LB
10.2337/db22-115-LB Google Scholar
- 83Chen L, Zhang J, Sun Y, et al. A phase I open-label clinical trial to study drug-drug interactions of Dorzagliatin and sitagliptin in patients with type 2 diabetes and obesity. Nat Commun. 2023; 14(1): 1405. doi:10.1038/s41467-023-36946-7