Glucagon-like-peptide-1 receptor agonists versus dipeptidyl peptidase-4 inhibitors and cardiovascular outcomes in diabetes in relation to achieved glycemic control. A Danish nationwide study
Abstract
Aim
To compare the cardiovascular preventive effect associated with glucagon-like-peptide-1 receptor agonists (GLP-1 RA) versus dipeptidyl peptidase-4 inhibitors (DPP-4i) according to the achieved target level of glycated hemoglobin (HbA1c).
Methods
We used retrospective Danish registries to include type 2 diabetes patients already in metformin treatment initiating GLP-1 RA or DPP-4i between 2007 and 2021. Patients were included 6 months after GLP-1 RA or DPP-4i initiation. The last available HbA1c measurement before inclusion was collected. The achieved HbA1c level was categorized according to a target level below or above 53 mmol/mol (7%). The primary outcome was a composite of nonfatal myocardial infarction, nonfatal stroke, and all-cause death. We used a multivariable Cox proportional hazard model to estimate the effect of HbA1c levels on the outcome among GLP-1 RA users compared to DPP-4i users.
Results
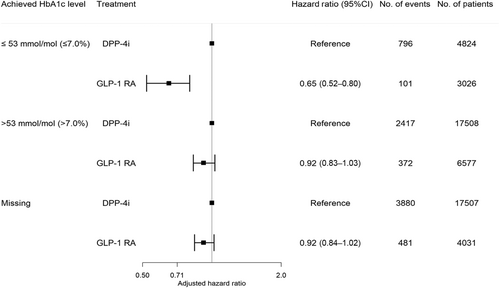
The study included 13 634 GLP-1 RA users (median age 56.9, interquartile range [IQR]: 48.5–65.5; 53% males) and 39 839 DPP-4i users (median age 63.4, IQR: 54.6–71.8; 61% males). The number of GLP-1 RA and DPP-4i users according to achieved HbA1c levels were as follows: HbA1c ≤ 53 mmol/mol (≤7.0%): 3026 (22%) versus 4824 (12%); HbA1c > 53 mmol/mol (>7.0%): 6577 (48%) versus 17 508 (44%); missing HbA1c: 4031 (30%) versus 17 507 (44%). During a median follow-up of 5 years (IQR: 2.6–5.0), 954 GLP-1 RA users experienced the primary outcome compared to 7093 DPP-4i users. The 5-year risk (95% confidence interval [CI]) of the outcome associated with GLP1-RA versus DPP-4i according to HbA1c categories was as follows: HbA1c ≤ 53 mmol/mol: 10.3% (8.2–12.3) versus 24.3% (22.7–25.8); HbA1c > 53 mmol/mol: 16.0% (14.3–17.6) versus 21.1% (20.3–21.9); missing HbA1c: 17.1% (15.7–18.5) versus 25.6% (24.9–26.3). The preventive effect associated with GLP-1 RA versus DPP-4i was significantly enhanced when achieving lower HbA1c levels: HbA1c ≤ 53 mmol/mol: 0.65 (0.52–0.80); HbA1c > 53 mmol/mol: 0.92 (0.83–1.03); missing HbA1c: 0.92 (0.84–1.02) (p value for interaction <.001).
Conclusion
GLP-1 RA use was associated with a lower rate of major adverse cardiovascular outcomes. The association was stronger in patients achieving the target glycemic level and weaker in patients not achieving the target glycemic level, suggestive of an interaction between achieved HbA1c level and GLP-1 RA.