Microbial and metabolomic profiles of type 1 diabetes with depression: A case–control study
Ziyu Liu
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Department of Endocrinology, The Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
Search for more papers by this authorTong Yue
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorXueying Zheng
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorSihui Luo
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorWen Xu
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Search for more papers by this authorJinhua Yan
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Search for more papers by this authorJianping Weng
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorCorresponding Author
Daizhi Yang
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Correspondence
Chaofan Wang and Daizhi Yang, Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, 600 Tianhe Road, Guangzhou 510630, China.
Email: [email protected] and [email protected]
Search for more papers by this authorCorresponding Author
Chaofan Wang
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Correspondence
Chaofan Wang and Daizhi Yang, Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, 600 Tianhe Road, Guangzhou 510630, China.
Email: [email protected] and [email protected]
Search for more papers by this authorZiyu Liu
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Department of Endocrinology, The Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
Search for more papers by this authorTong Yue
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorXueying Zheng
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorSihui Luo
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorWen Xu
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Search for more papers by this authorJinhua Yan
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Search for more papers by this authorJianping Weng
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of the Chinese Academy of Sciences (Hefei), University of Science and Technology of China, Hefei, China
Search for more papers by this authorCorresponding Author
Daizhi Yang
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Correspondence
Chaofan Wang and Daizhi Yang, Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, 600 Tianhe Road, Guangzhou 510630, China.
Email: [email protected] and [email protected]
Search for more papers by this authorCorresponding Author
Chaofan Wang
Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, Guangdong Diabetes Prevention and Control Research Center, Guangdong Provincial Key Laboratory of Diabetology, Guangzhou, China
Correspondence
Chaofan Wang and Daizhi Yang, Department of Endocrinology and Metabolism, The Third Affiliated Hospital of Sun Yat-sen University, 600 Tianhe Road, Guangzhou 510630, China.
Email: [email protected] and [email protected]
Search for more papers by this authorAbstract
Background
Depression is the most common psychological disorder in patients with type 1 diabetes (T1D). However, the characteristics of microbiota and metabolites in these patients remain unclear. This study aimed to investigate microbial and metabolomic profiles and identify novel biomarkers for T1D with depression.
Methods
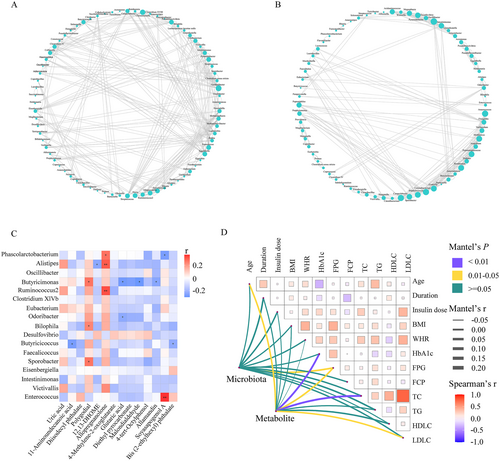
A case–control study was conducted in a total of 37 T1D patients with depression (TD+), 35 T1D patients without depression (TD−), and 29 healthy controls (HCs). 16S rRNA gene sequencing and liquid chromatography–mass spectrometry (LC–MS) metabolomics analysis were conducted to investigate the characteristics of microbiota and metabolites. The association between altered microbiota and metabolites was explored by Spearman's rank correlation and visualized by a heatmap. The microbial signatures to discriminate TD+ from TD− were identified by a random forest (RF) classifying model.
Results
In microbiota, 15 genera enriched in TD− and 2 genera enriched in TD+, and in metabolites, 14 differential metabolites (11 upregulated and 3 downregulated) in TD+ versus TD− were identified. Additionally, 5 genera (including Phascolarctobacterium, Butyricimonas, and Alistipes from altered microbiota) demonstrated good diagnostic power (area under the curve [AUC] = 0.73; 95% CI, 0.58–0.87). In the correlation analysis, Butyricimonas was negatively correlated with glutaric acid (r = −0.28, p = 0.015) and malondialdehyde (r = −0.30, p = 0.012). Both Phascolarctobacterium (r = 0.27, p = 0.022) and Alistipes (r = 0.31, p = 0.009) were positively correlated with allopregnanolone.
Conclusions
T1D patients with depression were characterized by unique profiles of gut microbiota and serum metabolites. Phascolarctobacterium, Butyricimonas, and Alistipes could predict the risk of T1D with depression. These findings provide further evidence that the microbiota–gut–brain axis is involved in T1D with depression.
REFERENCES
- 1Atkinson MA, Mirmira RG. The pathogenic “symphony” in type 1 diabetes: a disorder of the immune system, β cells, and exocrine pancreas. Cell Metab. 2023; 35(9): 1500-1518.
- 2Turin A, Drobnič RM. Psychosocial factors affecting the etiology and management of type 1 diabetes mellitus: a narrative review. World J Diabetes. 2021; 12: 1518-1529.
- 3Garey CJ, Clements MA, McAuliffe-Fogarty AH, et al. The association between depression symptom endorsement and glycemic outcomes in adolescents with type 1 diabetes. Pediatr Diabetes. 2022; 23: 248-257.
- 4Stahl-Pehe A, Selinski S, Bächle C, et al. Screening for generalized anxiety disorder (GAD) and associated factors in adolescents and young adults with type 1 diabetes: cross-sectional results of a Germany-wide population-based study. Diabetes Res Clin Pract. 2022; 184:109197.
- 5Ducat L, Rubenstein A, Philipson LH, Anderson BJ. A review of the mental health issues of diabetes conference. Diabetes Care. 2015; 38: 333-338.
- 6Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A. Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology. 2016; 70: 70-84.
- 7Castellano-Guerrero AM, Guerrero R, Relimpio F, et al. Prevalence and predictors of depression and anxiety in adult patients with type 1 diabetes in tertiary care setting. Acta Diabetol. 2018; 55: 943-953.
- 8Wang K, Li F, Cui Y, et al. The association between depression and type 1 diabetes mellitus: inflammatory cytokines as ferrymen in between? Mediators Inflamm. 2019; 2019:e2987901.
- 9Sharif K, Watad A, Coplan L, Amital H, Shoenfeld Y, Afek A. Psychological stress and type 1 diabetes mellitus: what is the link? Expert Rev Clin Immunol. 2018; 14: 1081-1088.
- 10Jamshidi P, Hasanzadeh S, Tahvildari A, et al. Is there any association between gut microbiota and type 1 diabetes? A systematic review. Gut Pathog. 2019; 11(1): 1-10.
- 11Zhou H, Zhao X, Sun L, et al. Gut microbiota profile in patients with type 1 diabetes based on 16S rRNA gene sequencing: a systematic review. Dis Markers. 2020; 2020: 1-11.
- 12Leiva-Gea I, Sánchez-Alcoholado L, Martín-Tejedor B, et al. Gut microbiota differs in composition and functionality between children with type 1 diabetes and MODY2 and healthy control subjects: a case-control study. Diabetes Care. 2018; 41(11): 2385-2395.
- 13De Groot PF, Belzer C, Aydin Ö, et al. Distinct fecal and oral microbiota composition in human type 1 diabetes, an observational study. PloS One. 2017; 12(12):e0188475.
- 14Pellegrini S, Sordi V, Bolla AM, et al. Duodenal mucosa of patients with type 1 diabetes shows distinctive inflammatory profile and microbiota. J Clin Endocrinol Metab. 2017; 102(5): 1468-1477.
- 15Mayneris-Perxachs J, Castells-Nobau A, Arnoriaga-Rodríguez M, et al. Microbiota alterations in proline metabolism impact depression. Cell Metab. 2022; 34: 681-701.
- 16Li Z, Lai J, Zhang P, et al. Multi-omics analyses of serum metabolome, gut microbiome and brain function reveal dysregulated microbiota-gut-brain axis in bipolar depression. Mol Psychiatry. 2022; 1-13: 4123-4135.
10.1038/s41380-022-01569-9 Google Scholar
- 17Yuan X, Chen B, Duan Z, et al. Depression and anxiety in patients with active ulcerative colitis: crosstalk of gut microbiota, metabolomics and proteomics. Gut Microbes. 2021; 13(1):e1987779.
- 18Musazadeh V, Zarezadeh M, Faghfouri AH, et al. Probiotics as an effective therapeutic approach in alleviating depression symptoms: an umbrella meta-analysis. Crit Rev Food Sci Nutr. 2022; 1-9: 8292-8300.
- 19Moludi J, Khedmatgozar H, Nachvak SM, Abdollahzad H, Moradinazar M, Sadeghpour TA. The effects of co-administration of probiotics and prebiotics on chronic inflammation, and depression symptoms in patients with coronary artery diseases: a randomized clinical trial. Nutr Neurosci. 2021; 1-10: 1659-1668.
- 20Ansari F, Pourjafar H, Tabrizi A, Homayouni A. The effects of probiotics and prebiotics on mental disorders: a review on depression, anxiety, Alzheimer, and autism Spectrum disorders. Curr Pharm Biotechnol. 2020; 21: 555-565.
- 21Nicolas GR, Chang PV. Deciphering the chemical lexicon of host-gut microbiota interactions. Trends Pharmacol Sci. 2019; 40: 430-445.
- 22Nicholson JK, Holmes E, Kinross J, et al. Host-gut microbiota metabolic interactions. Science. 2012; 336: 1262-1267.
- 23Lyra e Silva NDM, Lam MP, Soares CN, Munoz DP, Milev R, De Felice FG. Insulin resistance as a shared pathogenic mechanism between depression and type 2 diabetes. Front. Psychiatry. 2019; 10: 57.
- 24Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015; 3: 461-471.
- 25Petrak F, Herpertz S, Hirsch J, et al. Gut microbiota differs in composition between adults with type 1 diabetes with or without depression and healthy control participants: a case-control study. BMC Microbiol. 2022; 22: 169.
- 26Pon Velayutham AB, Mokhtari P, Metos JM, Jambal P, Shankar K. Gut microbial and metabolic signatures are altered in adolescents with type 1 diabetes. FASEB J. 2022; 36: S1.
- 27Zheng SJ, Luo Y, Xiao JH. The impact of intestinal microorganisms and their metabolites on type 1 diabetes mellitus. Diabetes Metab Syndr Obes. 2022; 15: 1123-1139.
- 28Weng J, Zhou Z, Guo L, et al. Incidence of type 1 diabetes in China, 2010-13: population based study. BMJ. 2018; 360:j5295.
- 29Yang D, Deng H, Luo G, et al. Demographic and clinical characteristics of patients with type 1 diabetes mellitus: a multicenter registry study in Guangdong, China. J Diabetes. 2016; 8: 847-853.
- 30Zung WW. The depression status inventory: an adjunct to the self-rating depression scale. J Clin Psychol. 1972; 28: 539-543.
10.1002/1097-4679(197210)28:4<539::AID-JCLP2270280427>3.0.CO;2-S CAS PubMed Web of Science® Google Scholar
- 31Dunstan DA, Scott N. Clarification of the cut-off score for Zung's self-rating depression scale. BMC Psychiatry. 2019; 19(177): 1-7.
- 32Bolyen E, Rideout JR, Dillon MR, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019; 37: 852-857.
- 33Magoč T, Salzberg SL. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics. 2011; 27: 2957-2963.
- 34Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJ, Holmes SP. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods. 2016; 13: 581-583.
- 35Sarafian MH, Gaudin M, Lewis MR, et al. Objective set of criteria for optimization of sample preparation procedures for ultra-high throughput untargeted blood plasma lipid profiling by ultra performance liquid chromatography-mass spectrometry. Anal Chem. 2014; 86: 5766-5774.
- 36Dunn WB, Broadhurst D, Begley P, et al. Procedures for large-scale metabolic profiling of serum and plasma using gas chromatography and liquid chromatography coupled to mass spectrometry. Nat Protoc. 2011; 6: 1060-1083.
- 37Segata N, Izard J, Waldron L, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011; 12: R60.
- 38Calle ML, Urrea V, Boulesteix AL, Malats N. AUC-RF: a new strategy for genomic profiling with random forest. Hum Hered. 2011; 72(2): 121-132.
- 39Wu Y, Jiao N, Zhu R, et al. Identification of microbial markers across populations in early detection of colorectal cancer. Nat Commun. 2021; 12(1): 3063.
- 40Pang Z, Chong J, Zhou G, et al. MetaboAnalyst 5.0: narrowing the gap between raw spectra and functional insights. Nucleic Acids Res. 2021; 49: W388-W396.
- 41Kahn LS, McIntyre RS, Rafalson L, Berdine DE, Fox CH. Fasting blood glucose and depressive mood among patients with mental illness in a Medicaid managed care program. Depress Res Treat. 2011; 2011:862708.
- 42Majumdar S, Sinha B, Dastidar BG, et al. Assessing prevalence and predictors of depression in type 2 diabetes mellitus (DM) patients - the DEPDIAB study. Diabetes Res Clin Pract. 2021; 178:108980.
- 43Mukherjee N, Chaturvedi SK. Depressive symptoms and disorders in type 2 diabetes mellitus. Curr Opin Psychiatry. 2019; 32: 416-421.
- 44Liu Y, Zhang L, Wang X, et al. Similar fecal microbiota signatures in patients with diarrhea-predominant irritable bowel syndrome and patients with depression. Clin Gastroenterol Hepatol. 2016; 14: 1602-1611.
- 45Huang Y, Shi X, Li Z, et al. Possible association of firmicutes in the gut microbiota of patients with major depressive disorder. Neuropsychiatr Dis Treat. 2018; 14: 3329-3337.
- 46Jiang H, Ling Z, Zhang Y, et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav Immun. 2015; 48: 186-194.
- 47Valles-Colomer M, Falony G, Darzi Y, et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol. 2019; 4: 623-632.
- 48Humbel F, Rieder JH, Franc Y, et al. Association of alterations in intestinal microbiota with impaired psychological function in patients with inflammatory bowel diseases in remission. Clin Gastroenterol Hepatol. 2020; 18(9): 2019-2029. e11.
- 49Yang J, Zheng P, Li Y, et al. Landscapes of bacterial and metabolic signatures and their interaction in major depressive disorders. Sci Adv. 2020; 6(49): eaba8555.
- 50Caso JR, MacDowell KS, González-Pinto A, et al. Gut microbiota, innate immune pathways, and inflammatory control mechanisms in patients with major depressive disorder. Transl Psychiatry. 2021; 11: 645.
- 51Yao Y, Qi X, Jia Y, et al. Evaluating the interactive effects of dietary habits and human gut microbiome on the risks of depression and anxiety. Psychol Med. 2022; 53(7): 3047-3055.
- 52Zhang Y, Zhang R, Liu P, et al. Characteristics and mediating effect of gut microbiota with experience of childhood maltreatment in major depressive disorder. Front Neurosci. 2022; 16:926450.
- 53Zhang Q, Yun Y, An H, et al. Gut microbiome and daytime function in Chinese patients with major depressive disorder. J Psychosom Res. 2022; 157:110787.
- 54Liu P, Gao M, Liu Z, et al. Gut microbiome composition linked to inflammatory factors and cognitive functions in first-episode, drug-naive major depressive disorder patients. Front Neurosci. 2021; 15:800764.
- 55Girdler SS, Lindgren M, Porcu P, Rubinow DR, Johnson JL, Morrow AL. A history of depression in women is associated with an altered GABAergic neuroactive steroid profile. Psychoneuroendocrinology. 2012; 37(4): 543-553.
- 56Slopien R, Pluchino N, Warenik-Szymankiewicz A, et al. Correlation between allopregnanolone levels and depressive symptoms during late menopausal transition and early postmenopause. Gynecol Endocrinol. 2018; 34(2): 144-147.
- 57Hink HU, Fukai T. Extracellular superoxide dismutase, uric acid, and atherosclerosis. Cold Spring Harb Symp Quant Biol. 2002; 67: 483-490.
- 58Ortiz R, Ulrich H, Zarate CJ, Machado-Vieira R. Purinergic system dysfunction in mood disorders: a key target for developing improved therapeutics. Prog Neuropsychopharmacol Biol Psychiatry. 2015; 57: 117-131.
- 59Zhang C, Mo YY, Feng SS, et al. Urinary metabonomics study of anti-depressive mechanisms of Millettia speciosa champ on rats with chronic unpredictable mild stress-induced depression. J Pharm Biomed Anal. 2021; 205:114338.
- 60Zhang L, Zou W, Huang Y, et al. A preliminary study of uric metabolomic alteration for postpartum depression based on liquid chromatography coupled to quadrupole time-of-flight mass spectrometry. Dis Markers. 2019; 2019:e4264803.
- 61Kang JS, Baek JH, Jung S, Chung HJ, Lee DK, Kim HJ. Ingestion of bis (2-ethylhexyl) phthalate (DEHP) during adolescence causes depressive-like behaviors through hypoactive glutamatergic signaling in the medial prefrontal cortex. Environ Pollut. 2021; 289:117978.
- 62Liu Z, Zhu Z, Zhao J, et al. Malondialdehyde: a novel predictive biomarker for post-stroke depression. J Affect Disord. 2017; 220: 95-101.
- 63Moludi J, Alizadeh M, Mohammadzad MHS, Davari M. The effect of probiotic supplementation on depressive symptoms and quality of life in patients after myocardial infarction: results of a preliminary double-blind clinical trial. Psychosom Med. 2019; 81(9): 770-777.
- 64Faust K, Raes J. Microbial interactions: from networks to models. Nat Rev Microbiol. 2012; 10(8): 538-550.
- 65Gao Y, Davis B, Zhu W, Zheng N, Meng D, Walker WA. Short-chain fatty acid butyrate, a breast milk metabolite, enhances immature intestinal barrier function genes in response to inflammation in vitro and in vivo. Am J Physiol Gastrointest Liver Physiol. 2021; 320(4): G521-G530.
- 66Del Rizzo M, Galderisi A, Celato A, et al. The long-term treatment of a patient with type 1 diabetes mellitus and glutaric aciduria type 1: the effect of insulin. Eur J Pediatr. 2016; 175: 1123-1128.
- 67Lu J, Zhou J, Bao Y, et al. Serum metabolic signatures of fulminant type 1 diabetes. J Proteome Res. 2012; 11(9): 4705-4711.
- 68Goodarzi MT, Navidi AA, Rezaei M, Babahmadi-Rezaei H. Oxidative damage to DNA and lipids: correlation with protein glycation in patients with type 1 diabetes. J Clin Lab Anal. 2010; 24(2): 72-76.
- 69Lin CC, Huang HH, Hu CW, et al. Trace elements, oxidative stress and glycemic control in young people with type 1 diabetes mellitus. J Trace Elem Med Biol. 2014; 28(1): 18-22.
- 70Michalakeas CA, Parissis JT, Douzenis A, et al. Effects of sertraline on circulating markers of oxidative stress in depressed patients with chronic heart failure: a pilot study. J Card Fail. 2011; 17(9): 748-754.
- 71Wei YC, Zhou FL, He DL, et al. Oxidative stress in depressive patients with gastric adenocarcinoma. Int J Neuropsychopharmacol. 2009; 12(8): 1089-1096.
- 72Wu F, Guo X, Zhang J, Zhang M, Ou Z, Peng Y. Phascolarctobacterium faecium abundant colonization in human gastrointestinal tract. Exp Ther Med. 2017; 14(4): 3122-3126.
- 73Huang Y, Li SC, Hu J, et al. Gut microbiota profiling in Han Chinese with type 1 diabetes. Diabetes Res Clin Pract. 2018; 141: 256-263.
- 74Gavin PG, Mullaney JA, Loo D, et al. Intestinal metaproteomics reveals host-microbiota interactions in subjects at risk for type 1 diabetes. Diabetes Care. 2018; 41(10): 2178-2186.
- 75Ma Q, Li Y, Wang J, et al. Investigation of gut microbiome changes in type 1 diabetic mellitus rats based on high-throughput sequencing. Biomed Pharmacother. 2020; 124:109873.
- 76Reddy DS. Neurosteroids: endogenous role in the human brain and therapeutic potentials. Prog Brain Res. 2010; 186: 113-137.
- 77Diviccaro S, Falvo E, Piazza R, et al. Gut microbiota composition is altered in a preclinical model of type 1 diabetes mellitus: influence on gut steroids, permeability, and cognitive abilities. Neuropharmacology. 2022; 2022:109405.
- 78Schüle C, Nothdurfter C, Rupprecht R. The role of allopregnanolone in depression and anxiety. Prog Neurobiol. 2014; 113: 79-87.