Association of sedentary time and carotid atherosclerotic plaques in patients with type 2 diabetes
久坐时间与2型糖尿病患者颈动脉粥样硬化斑块的关系
Jing Ke, Kun Li, Tingyu Ke, and Xu Zhong contributed equally to the study.
Abstract
enBackground
Atherosclerosis is a common complication in patients with type 2 diabetes (T2DM). Multiple factors are involved in the development and progress of atherosclerosis. We evaluated the association of weekly sedentary time (WST) with carotid plaque formation.
Methods
After data cleaning, a total of 26 664 participants with T2DM from 10 National Metabolic Management Centers (MMCs) from June 2017 to April 2021 were enrolled. Self-reported lifestyle data including WST, sleeping time, smoking and drinking information, carotid artery ultrasound, and biochemical parameters were obtained. The independent association of carotid plaue with sedentary and other lifestyle behaviors was evaluated using multivariable logistic regression models, and odds ratio (OR) with 95% confidence interval (CI) were reported. Moreover, stratified analysis was conducted to demonstrate the influence of confounding factors.
Results
The mean (SD) age of the participants was 54.0 (11.6) years, and the median (interquartile range) WST was 35.0 (21.0, 42.0) h. Comparing with participants in the first tertile of WST, those in the second or third tertile of WST were younger and with a shorter duration of diabetes. There were positive associations between longer sedentary time and odds of artery plaque after adjustment, with corresponding ORs in the second and third tertile were 1.40 (95% CI: 1.31–1.50) and 1.67 (95% CI: 1.56–1.79), respectively. However, the effect of WST on plaque in patients aged 18–40 years old had no statistical significance; the p value in the third tertile was 0.163.
Conclusions
In summary, higher WST appears to be associated with higher prevalence of carotid plaque in patients with T2DM, especially in aged populations.
摘要
zh背景
动脉粥样硬化是2型糖尿病患者的常见并发症。动脉粥样硬化的发生发展涉及多种因素。我们评估了每周久坐时间(WST)与颈动脉斑块形成的关系。
方法
数据清理后, 纳入2017年6月至2021年4月10个国家代谢管理中心(MMC)的26664例2型糖尿病患者。自报生活方式资料包括WST, 睡眠时间, 吸烟和饮酒情况, 颈动脉超声和生化指标。用多变量Logistic回归模型评估久坐与其他生活方式行为之间的独立关联, 并报告95%可信区间(CI)的优势比(OR)。此外, 还对混杂因素进行了分层分析, 论证了混杂因素的影响。
结果
受试者的平均年龄为54.0(11.6)岁, WST的中位数(四分位数范围)为35.0(21.0, 42.0)小时。与WST前3分位数的受试者相比, WST第二或第三3分位数的受试者年龄更小, 糖尿病病程更短。调整后久坐时间与动脉斑块形成的OR值呈正相关, 调整后2, 3分位数的OR值分别为1.40(95%CI:1.31~1.50)和1.67(95%CI:1.56~1.79)。而WST对18~40岁患者斑块的影响无统计学意义, 第三3分位数P值为0.163。
结论
高WST似乎与T2 DM患者颈动脉斑块的高患病率有关, 尤其是在老年人群中。
1 INTRODUCTION
Atherosclerosis is the major cause of cardiovascular diseases (CVD) including coronary heart disease, stroke, peripheral vascular disease, and so on. It has been widely accepted that atherosclerosis is the basic and early pathophysiological change in CVD. Increased risk and accelerated development of atherosclerosis have been shown in studies on diabetic patients.1 Moreover, patients of diabetes mellitus with carotid plaques may develop more severe atherosclerotic disease.2 Exploring the risk factors of atherosclerosis and intervening can help to reduce the incidence of CVD, which has important public health significance.3
Lifestyle is related to cardiovascular and CVD. The Framingham Heart Study provided evidence that smoking was an independent risk factor of CVD.4 In addition, it has been reported that physical activity protects against atherosclerosis and limits coronary heart diseases as well as carotid artery diseases.5, 6 During the past several decades, people are spending increasing amounts of time in environments that not only limit physical activity but require prolonged sedentary time at work, in cars, and in public spaces.7 The shift from time spent in light activities to time being sedentary has likely contributed to obesity and type 2 diabetes (T2DM).8
Some studies have explored the association between sedentary time and CVD. In a cross-sectional epidemiological study based on 2043 inhabitants of the Corinthia region in Greece, higher television viewing time group has been found to be associated with 80% increased odds of carotid atheromatic plaque.9 Another study in Korean youth showed that screen-based sedentary behavior was associated with high risk of overweight, abdominal adiposity, and low high-density lipoprotein cholesterol.10 Moreover, Pauline Mury et al.11 have demonstrated that greater physical activity and sedentary time were associated with a lower prevalence of intraplaque hemorrhage in 90 asymptomatic patients. In addition, several studies explored the relationship between sedentary behavior and diabetes mellitus. An investigation in women over 65 years in the United States suggested that replacing sedentary time or light physical activity with moderate-to-vigorous physical activity was associated with lower diabetes risk.12
However, there were no multicenter studies estimating the effect size of sedentary and other behavior as risk factors for atherosclerosis in patients with T2DM. Therefore, we explored the association between self-reported sedentary time and other lifestyle behaviors and carotid atherosclerotic plaques in patients with T2DM using national multicenter data.
2 METHOD
2.1 Study design and population
The present study was a cross-sectional design. From June 2017 to April 2021, patients with diabetes were registered at 10 National Metabolic Management Centers (MMC) in various administrative regions of China, which are located in Beijing (one site), Zhejiang (two sites), Shanghai (two sites), Henan (two sites), Guizhou (one site), Yunnan (one site), and Jiangsu (one site). All of the patients accepted systematic physical examination, blood sample collection, and oral questionnaire interviews. The protocol of this project was published previously.11 In the present study, participants were limited to adult patients (≥18 years) diagnosed with T2DM.
The study protocol was approved by the Medical Ethics Committee of Ruijing Hospital, Shanghai Jiaotong University, and other participating centers if necessary. This study was performed in accordance with the Declaration of Helsinki and all study participants provided written informed consent.
2.2 Data collection
Data collection was performed at each study center according to the standard protocol of MMC, which is a national project to manage metabolic patients based on the concept of “One Center, One Step, and One Standard Model.”13 All of people engaged in data collection and laboratory detection were trained according to the same standard. In addition, some indicators were detected using same the model of machine, such as pulse wave velocity (PWV), visceral fat area (VFA), and subcutaneous fat area (SFA). More measures for quality control could be seen in the protocol of MMC.13
The questionnaire containing the information of demographic characteristics, lifestyle factors (including alcohol drinking and cigarette smoking), medical history, and family history was administered by trained interviewers. The history of hypertension and dyslipidemia was defined by a self-reported physician diagnosis. For the participants who drank alcohol weekly or almost weekly, drinking status was defined as “yes.” Educational attainment was categorized as less than high school and high school or more. Height and body weight were measured with a standard protocol, and body mass index (BMI) was calculated as weight divided by height squared. Ankle brachial index (ABI) was measured noninvasively by an automated recording apparatus with participants in the supine position after at least 5 min of rest (BP-203RPE III, form PWV/ABI, Omron Healthcare Co.). SFA and VFA were measured at the level of umbilicus by a dual bioelectrical impedance analyzer (HDS2000, Omron Healthcare Co.). Each participant's blood pressure was measured by using an automated electronic device. Fasting blood glucose (FBG), glycated hemoglobin (HbA1c), uric acid, lipid profiles, and the urinary albumin-to-creatinine ratio (UACR) were tested in each center. Carotid plaque was detected by ultrasound in local MMCs. Each patient's bilateral carotid arteries were examined by ultrasound physicians using a Doppler apparatus. Carotid plaque was defined as “yes” when plaque was reported in either side of the carotid and the branches.14
We used the International Physical Activity Questionnaire to assess physical activity.15 Sedentary time was evaluated by weekly sitting time (WST), which was calculated by the following formula: WST = [(daily sitting time for the weekday) × (number of weekdays per week) + (daily sitting time of rest day) × (number of rest days off per week)]. Other lifestyle behaviors were defined from the items of Ideal Cardiovascular Health Metrics, which were adapted from the recommendations of the Goals and Metrics Committee of the Strategic Planning Task Force of the American Heart Association.16 “Ideal smoking” was defined as never smoking or stopped smoking >12 months; “physical activity at goal” was defined as performing ≥150 min/week of moderate-intensity physical activity, ≥75 min/week of vigorous-intensity physical activity, or ≥150 min/week of moderate-intensity and vigorous-intensity physical activity.
2.3 Statistical analysis
Data are presented as mean ± SD or median [interquartile range (IQR)] values for continuous variables, and as the frequency (%) for categorical variables. Data were tested for normal distribution and logarithmically transformed for statistical analysis when required. The p values for trend were calculated by using the Cochran-Armitage trend test and linear regression analyses for categorical and continuous variables across the three groups, respectively.
The independent association of carotid plaque with sedentary time and other lifestyle behaviors was evaluated using multivariable logistic regression models, and odds ratio (OR) and 95% confidence interval (CI) were reported.
We constructed three models with adjustments for major covariables: model 1 input major variables of sedentary and other lifestyle behaviors; obesity, history of hypertension, and history of hyperlipidemia were main factors in the cardiovascular research and associated with artery plaque, which was reported in previous studies.11 To avoid the confounding effects of these variable, we adjusted for obesity, history of hypertension, and history of hyperlipidemia in model 2. The model 3 included all variables in model 2 plus demographic variables (age, sex, education level) and diabetes-related variables (duration of diabetes, HbA1c) to further adjust for possible confounding factors. Moreover, we performed stratified analysis on the association between carotid plaque and sedentary and other lifestyle behaviors with subgroups of sex and age using multivariable logistic regression models with full adjustment in model 3.
Percentiles of WST were estimated using the generalized additive models for location, shape, and scale (GAMLSS) method, which was implemented in the GAMLSS package of R. The GAMLSS method is an extension of the Lambda-Median-Sigma method, which was introduced by Rigby and Stasinopoulos to address some of the limitations associated with generalized linear models and generalized additive models. All analyses were performed using R software version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria). A two-sided p value <0.05 was considered statistically significant.
3 RESULTS
3.1 Baseline demographic and clinical parameters of the study participants
In the present study, missing values were defined as lacking information of sedentary time, HbA1c, and carotid ultrasound. If any of the variables were missing, the record was excluded. As a result, 26 968 participants without the aforementioned missing values were available for the main analysis. After excluding patients with diabetic foot (n = 304), a total of 26 664 T2DM patients (nonpregnant) were finally enrolled. The detail of the data cleaning procedure could be seen in Figure S1.
Table 1 described the demographic and clinical characteristics of participants according to the tertiles of WST. The mean (SD) age of the participants was 54.0 (11.6) years, and 15 496 were male (58.1%). The median (interquartile range) WST was 35.0 (21.0, 42.0) h. With the increase of WST, most of the demographic and clinical variables showed an upward or downward trend (Table 1). Compared with the participants in the first tertile of WST, those in the second or third tertile of WST were younger with a shorter duration of diabetes, lower HbA1c, fasting blood glucose, HDL cholesterol, and ABI (all p < .01). The participants in the higher tertile of WST tend to be obese, which has a larger value of physical measurement index including BMI, body weight, and VFA, and waist circumference.
| Variables | Overall | Weekly sedentary time (h) | p | ||
|---|---|---|---|---|---|
| Tertile 1 | Tertile 2 | Tertile 3 | |||
| n | 26 664 | 8 692 | 8 669 | 9 303 | - |
| Sex, male n (%) | 15 496 (58.12%) | 4 667 (53.71%) | 5 140 (59.30%) | 5 689 (61.16%) | <0.001 |
| Age, years | 54.0 ± 11.6 | 56.0 ± 10.5 | 53.9 ± 11.6 | 52.2 ± 12.3 | <0.001 |
| Carotid plaque, n (%) | 11 284 (42.32%) | 3 316 (38.15%) | 3 765 (43.43%) | 4 203 (45.18%) | <0.001 |
| Duration of diabetes, years | 6.8 ± 6.9 | 7.3 ± 7.0 | 6.7 ± 6.9 | 6.5 ± 6.8 | <0.001 |
| High school education and above, n (%) | 11 766 (44.14%) | 2 675 (30.78%) | 4 104 (47.36%) | 4 987 (53.61%) | <0.001 |
| History of hypertension n (%) | 11 106 (41.92%) | 3 843 (44.45%) | 3 614 (41.87%) | 3 649 (39.60%) | <0.001 |
| Hypertensive medication use, n (%) | 10 468 (39.32%) | 3 543 (40.81%) | 3 395 (39.22%) | 3 530 (38.02%) | <0.001 |
| History of dyslipidemia, n (%) | 7 986 (30.15%) | 2 563 (29.71%) | 2 563 (29.71%) | 2 860 (30.97%) | 0.064 |
| Ideal smoking status, n (%) | 19 307 (72.67%) | 6 621 (76.38%) | 6 233 (72.21%) | 6 453 (69.63%) | <0.001 |
| Drinking, n (%) | 3 217 (12.08%) | 1 023 (11.78%) | 1 037 (11.98%) | 1 157 (12.46%) | 0.161 |
| BMI, kg/m2 | 26.1 ± 3.9 | 25.8 ± 3.7 | 26.0 ± 3.8 | 26.4 ± 4.1 | <0.001 |
| Body weight, kg | 70.9 ± 13.4 | 68.9 ± 12.4 | 71.0 ± 13.1 | 72.6 ± 14.4 | <0.001 |
| Visceral fat area, cm2 | 102.1 ± 41.7 | 97.9 ± 41.4 | 101.9 ± 41.7 | 106.5 ± 41.6 | <0.001 |
| Waist circumference, cm | 92.0 ± 10.1 | 90.8 ± 9.8 | 91.9 ± 9.8 | 93.2 ± 10.5 | <0.001 |
| SBP, mmHg | 132.5 ± 18.7 | 133.8 ± 19.3 | 132.0 ± 18.6 | 131.8 ± 18.1 | <0.001 |
| Fasting blood glucose, mmol/L | 9.5 ± 3.8 | 10.0 ± 4.1 | 9.5 ± 3.7 | 9.2 ± 3.5 | <0.001 |
| Fasting serum C peptide, ng/ml | 2.04 (1.40, 2.83) | 2.04 (1.40, 2.84) | 2.00 (1.37, 2.79) | 2.07 (1.42, 2.87) | 0.708 |
| HbA1c, % | 8.7 ± 2.2 | 8.8 ± 2.2 | 8.7 ± 2.1 | 8.6 ± 2.1 | <0.001 |
| Triglycerides, mmol/L | 1.60 (1.10, 2.43) | 1.53 (1.05, 2.33) | 1.61 (1.11, 2.44) | 1.66 (1.15, 2.51) | <0.001 |
| Total cholesterol, mmol/L | 4.99 ± 1.32 | 5.07 ± 1.31 | 4.98 ± 1.34 | 4.91 ± 1.30 | 0.011 |
| HDL cholesterol, mmol/L | 1.18 ± 0.33 | 1.22 ± 0.36 | 1.17 ± 0.32 | 1.15 ± 0.31 | <0.001 |
| LDL cholesterol, mmol/L | 3.02 ± 1.00 | 3.07 ± 1.03 | 3.02 ± 1.00 | 2.98 ± 0.97 | <0.001 |
| UACR, mg/mmol | 2.14 (0.93, 4.93) | 2.30 (1.02, 6.00) | 1.99 (0.89, 4.54) | 2.10 (0.90, 4.45) | 0.191 |
| TSH, μIU/ml | 1.88 (1.24, 2.85) | 1.79 (1.15, 2.73) | 1.91 (1.28, 2.88) | 1.94 (1.30, 2.93) | 0.034 |
| ABI | 1.11 ± 0.10 | 1.11 ± 0.10 | 1.10 ± 0.10 | 1.10 ± 0.10 | <0.001 |
- Note: Data are expressed as mean ± SD, median (interquartile range), or n (%). The p values for trend were calculated by using the Cochran–Armitage trend test and linear regression analyses for categorical and continuous variables across the three groups, respectively.
- Abbreviations: ABI, ankle brachial index; BMI, body mass index; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure; TSH, thyroid stimulating hormone; UACR, urine albumin-to-creatinine ratio.
3.2 The association between artery plaque and lifestyle behaviors
The sedentary time and other lifestyles were associated with artery plaque in T2DM patients. The prevalence of artery plaque was 42.32% in all the participants. Table 2 gave the model information of artery plaque in T2DM, and the effect of WST and other factors on artery plaque was present as ORs and 95% CI. There were positive associations between longer WST and odds of artery plaque after adjustment, and the corresponding ORs in the second and third tertiles were 1.40 (95% CI: 1.31–1.50) and 1.67 (95% CI: 1.56–1.79), respectively. The ORs of physical activity at goal and sleeping hours was 0.98 (95% CI: 0.96–1.00) and 0.89 (95% CI: 0.81–0.98) after adjusting for covariates. Both smoking and drinking were risk factors for artery plaque. More details of model 2 can be seen in Table 2.
| Model 1 | Model 2a | Model 3b | |
|---|---|---|---|
| Weekly sedentary time | |||
| Tertile 1 | Reference | - | - |
| Tertile 2 | 1.22 (1.15, 1.30) | 1.27 (1.19, 1.35) | 1.40 (1.31, 1.50) |
| Tertile 3 | 1.30 (1.22, 1.38) | 1.37 (1.29, 1.46) | 1.67 (1.56, 1.79) |
| Sleeping hours | 1.00 (0.99, 1.02) | 1.00 (0.98, 1.01) | 0.98 (0.96, 1.00) |
| Activity at goal | 0.83 (0.76, 0.90) | 0.86 (0.78, 0.94) | 0.89 (0.81, 0.98) |
| Ideal smoking status | 0.91 (0.86, 0.96) | 0.85 (0.80, 0.90) | 0.81 (0.76, 0.87) |
| Drinking | 1.19 (1.10, 1.28) | 1.16 (1.07, 1.26) | 1.11 (1.01, 1.21) |
- a Model 2: Adjusted for variables in model 1 plus obesity, history of hypertension, history of hyperlipidemia.
- b Model 3: Adjusted for variables in model 2 plus age, sex, education level, duration of diabetes, and HbA1c.
3.3 Stratified analysis for association of artery plaque and lifestyle behaviors
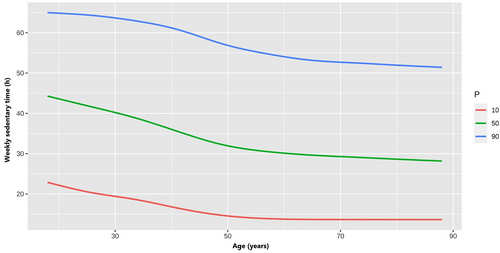
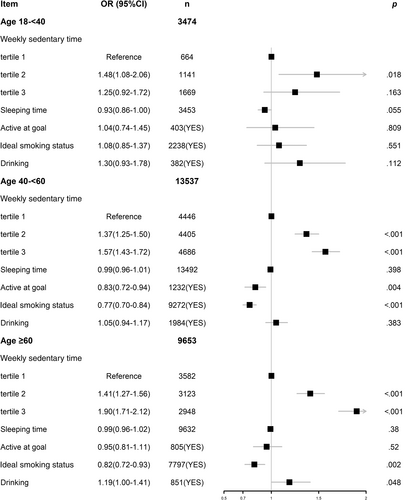
Considering that the participants' age was not uniformly distributed in each sedentary tertile, we fit an age-dependent trend plot of WST using the GAMLSS model (Figure 1). There was a negative association between age and WST, and the median WST decreased from 45 h to 30 h in T2DM patients between 18 and 80 years old. We also did interaction effect test for age and sedentary time with carotid plaque; results indicated that the age and sedentary time may have positive interactive effect on carotid plaque (Figure S2). Moreover, the stratified analysis showed that both the middle aged (40–<60 years) and older aged (≥60 years) groups have a positive associative between WST and the odds of artery plaque, which was consistent with the result overall. However, there was no statistical significance for the effect of WST on the plaque in the patients aged 18–40 years old, the p value in the third tertile was 0.163. Similar results could also be found in activity at goal, ideal smoking status (Figure 2).
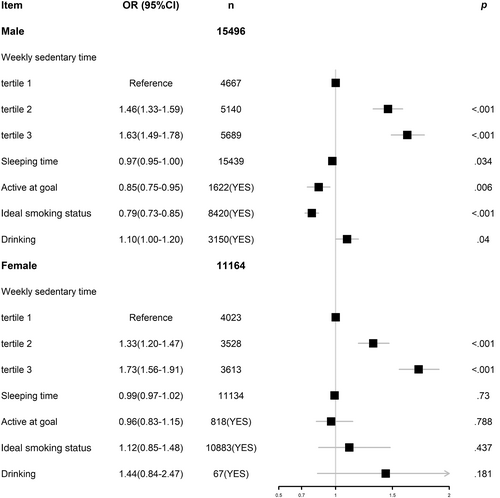
In addition, we conducted a stratified analysis of the relationship between artery plaque and lifestyle behaviors for sex. The result was much similar in the sex subgroup, the corresponding ORs of third tertiles in male and female were 1.63 (95% CI: 1.49–1.78) and 1.73 (95% CI: 1.56–1.91), respectively (Figure 3).
4 DISCUSSION
Previous studies have explored the association between lifestyle and CVD. Some cohort and cross-sectional studies have suggested that sedentary time is associated with CVD, coronary heart disease, stroke, hypertension, and hypercholesterolemia.17
Using a large nationally representative sample of diabetic patients, our study suggested the sedentary time is a risk factor for carotid plaque. Previous research with 7 days using ActiGraph accelerometers was consistent with the finding in this study on the association of sedentary time and carotid intima-media thickness in the Spanish healthy adult population.18 Another study in 100 patients with T2DM complicated with peripheral artery disease showed that the reduction of sedentary time can significantly improve the effectiveness of exercise therapy.19 In the meantime, a meta-analysis suggested that reducing sedentary behavior among clinical populations could improve cardiometabolic risk markers such as waist circumference, fat percentage, and glycemic control.20
Moreover, we found that differences in age were associated with the different levels of sedentary time. Surprisingly and interestingly, our data showed that older adults have the least sedentary time than other age groups, which is contrary to our speculation and studies in other countries.21 With the changes of times, older adults have abundant and colorful life in their retirement, whereas young populations are more prone to be bound to work and families. This may explain the lower exposure to sedentary behaviors in elderly in our study. Sedentary time has emerged as a new health risk for cardiometabolic diseases and all-cause mortality, independent of time spent in exercise.22 One study including 3319 old patients free of CVD (mean age = 68.9 years in 2012 and 2013) showed that moderate to vigorous physical activity was associated with lower incidence of CVD.23 Another cohort study in 2014 and 2018 including 6785 elderly persons in South Korea showed that prolonged sedentary behavior is related to cardiovascular diseases and cancers.24 A meta-analysis containing 24 studies showed that greater sedentary time was related to an increased risk of all-cause mortality in adults over 60 years of age, which is based on high exposure to sedentary time in the elderly.25 From our analysis of ORs, we found that sedentary time was significantly associated with a higher risk of carotid plaque in elderly patients. Moreover, in the subgroup analysis, we showed that sedentary time was related to carotid plaque in middle-aged and aged populations instead of patients aged between 18 and 40 years. Therefore, the development of carotid plaque may be related to prolonged exposure to sedentary time, and the outcome appears after years of sedentary exposure, which may explain the interaction effect shown in statistically.
A long-term cohort study is needed to verify the result of the present study. In addition, the effect sizes of smoking and drinking show a great difference in sex subgroup, which may be because of the relative inadequacy of exposure sample size in female group. The 95% CI of ORs of smoking and drinking in the female subgroup was much wider, which also confirmed this result.
Limited researches have explored the biological mechanism of sedentary time and plaque; one study that examined the neovascularization, macrophage infiltration in the plaque found no significant difference.9 Another study has tested the urinary metabolites in different levels of sedentary time, and results showed increased levels of glycine, L-valine, L-threonine, L-phenylalanine, L-leucine, L-alanine, succinic acid, 2-ketoglutaric acid, xylitol, and ribitol in female patients with T2DM.26 This study may allow us to hypothesize that sedentary time may exert a harmful effect on the development and progress of carotid plaque through metabolic signatures, and further studies are needed to illuminate the specific mechanism.
Finally, some limitations existed in our study. First, the use of self-reported data on sedentary time and other lifestyles may have misreporting and bias. Second, our cross-sectional study does not allow us to draw any causal relationship between sedentary time and carotid plaque. Prospective studies will advance this field in further study.
5 CONCLUSIONS
In this cross-sectional study, we showed that sedentary time is the independent risk factor for carotid plaque in multicenter and large sample in Chinese diabetic patients, which is the main finding and novelty of the study. As the results relied on cross-sectional data in which there was no experimental intervention for replacement of behaviors, it should be interpreted as associations, and future studies are needed to prove whether interventions to reduce sedentary time prevent incidence of carotid plaque of T2DM.
ACKNOWLEDGEMENT
This study was supported by grants from the National Key Research and Development Program of China (No. 2018YFC1311800, No. 2016YFC0901200), National Natural Science Foundation of China (Grant No. 81800768), Chinese Academy of Engineering (2019-XZ-42), and the Program for Shanghai Outstanding Medical Academic Leader (No. 2019LJ07).
CONFLICT OF INTEREST
The authors report no conflicts of interest in this work.




