Electrophysiologically verified effects of acupuncture on diabetic peripheral neuropathy in type 2 diabetes: The randomized, partially double-blinded, controlled ACUDIN trial
电生理验证针灸对2型糖尿病周围神经病变的影响:随机、部分双盲的ACUDIN对照试验
Funding information: HanseMerkur Insurance Group, Hamburg, Grant/Award Number: PNP/2011; Innovation Foundation, Hamburg, Grant/Award Number: 721.230-002; Laser devices were provided by Laserneedle GmbH, Glienicke/Nordbahn, Germany, Grant/Award Number: HH-PNP
Abstract
enBackground
Acupuncture is commonly used in Traditional Chinese Medicine for treatment of diabetic peripheral neuropathy (DPN), but data from randomized controlled trials are rare.
Methods
This randomized, placebo-controlled, partially double-blinded clinical trial randomly assigned adults with confirmed type 2 diabetes-induced DPN to receive 10 sessions of needle acupuncture, laser acupuncture, or placebo laser acupuncture for 10 consecutive weeks. Treatment was provided at bilateral acupoints Ex-LE-10 (Bafeng), Ex-LE-12 (Qiduan), and ST-34 (Lianqiu).
Neurological assessments, including nerve conduction studies (NCS) of sural and tibial nerves, were performed at baseline and weeks 6 and 15. Primary outcome was delta of sural sensory nerve action potential (SNAP). Secondary outcomes included further NCS values, clinical scores, and patient-reported outcome measures (PROMs).
Results
Of 180 participants, 172 completed the study. Sural SNAP and sural and tibial nerve conduction velocities improved significantly after 10 treatments when comparing needle acupuncture to placebo. Needle acupuncture showed earlier onset of action than laser acupuncture. PROMs showed larger improvements following needle and laser acupuncture than placebo, reaching significant differences for hyperesthesia and cramps following needle acupuncture and for heat sensation following laser acupuncture.
Conclusions
Classical needle acupuncture had significant effects on DPN. Improvement in NCS values presumably indicates structural neuroregeneration following acupuncture.
摘要
zh背景
针灸是中医常用的治疗糖尿病周围神经病变(DPN)的方法; 但来自随机对照试验的数据很少
方法
这项随机、安慰剂对照、部分双盲的临床试验将确诊为2型糖尿病所致DPN的成人患者随机分为针刺组、激光针刺组或安慰剂激光针刺组; 连续10周。在双侧穴位Ex-LE-10(八风)、EX-LE-12(气端)和ST-34(梁丘)进行治疗。在基线、第6周和第15周进行神经学评估; 包括腓肠神经和胫神经的神经传导研究(NCS)。主要结果是腓肠感觉神经动作电位(SNAP)的增量。次要结果包括进一步的NCS值、临床评分和患者报告的结果测量(PROMs)。
结果
在180名参与者中; 172人完成了研究。与安慰剂相比; 针灸治疗10次后; 腓肠神经SNAP、腓肠神经和胫神经传导速度均有明显改善。针刺起效早于激光针刺。与安慰剂相比; 针刺和激光针刺对PROMS有更大的改善; 针灸后的感觉过敏和痉挛具有显著差异; 激光针灸后的热感方面具有显著差异。
结论
经典针刺治疗DPN疗效显著。NCS值的改善可能表明针灸后存在结构性神经再生。
1 INTRODUCTION
Diabetic peripheral neuropathy (DPN) is a common complication of type 1 and type 2 diabetes mellitus. Duration of diabetes and hyperglycemia are major risk factors; however, rigorous glycemic control has shown to be insufficient to prevent DPN in type 2 diabetes.1 Metabolic sequelae directly affect neuronal tissues and the vasa nervorum,2 causing changes in nerve microvasculature with reduced nerve perfusion and endoneurial hypoxia.3 Several pathomechanisms contribute to peripheral nerve injury in DPN, including oxidative stress, mitochondrial dysfunction, inflammation, and altered gene regulation.4 Recent research focuses on endoplasmic reticulum stress (ERS) and mediated cell apoptosis in the pathophysiology of DPN.5, 6
DPN typically presents as a chronic, symmetrically distributed stocking glove, length-dependent sensorimotor polyneuropathy.7 Sensory clinical manifestations include neuropathic pain, paresthesia, hyperesthesia, or hypoesthesia.7 Motor symptoms occur less frequently.8 DPN is associated with increased risks of foot ulcers, Charcot arthropathy, and lower extremity amputation8 and a greater risk of falling due to gait insecurity.9 Overall, DPN causes elevated healthcare costs.10 Pharmacologic treatment is limited to palliating neuropathic pain and paresthesia,11 whereas neuronal degeneration remains unaffected.
During the last decades, acupuncture was empirically applied for treatment of DPN, yielding positive reports.12-14
The aim of the ACUDIN (ACUpuncture and laser acupuncture for treatment of DIabetic peripheral Neuropathy) trial was to quantify the effect of acupuncture on DPN in NCS and on patient-reported outcome measures (PROMs) and clinical variables compared with placebo.
The definition of adequate control interventions for a double-blind study design has, despite many efforts, remained a methodological challenge in acupuncture trials. Sham needling performed away from acupuncture points or shallow needling elicits unspecific physiological responses on skin penetration and cannot be regarded as an inactive placebo intervention.15-17 To date, there are no international standards regarding direct placebo procedures for the evaluation of acupuncture effects in a double-blind study.
Therefore, we chose an indirect control for the ACUDIN trial, using laser acupuncture as a second treatment intervention. Laserneedle is a particular type of laser acupuncture that has previously been shown to be equally effective as needle acupuncture18-21 and is suitable for placebo treatment, preventing any nonspecific physiological activation by deactivated laser irradiation.18 This can be completely concealed from the patient. Laser acupuncture has been previously evaluated as valid control for classifying the effect of acupuncture needling.22 Therefore, we included laser acupuncture as a second verum treatment and placebo intervention in a double-blind procedure in the ACUDIN trial. Particulars are detailed in the previously published trial protocol.23
2 METHODS
The prospective, randomized, partially double-blinded, placebo-controlled, three-armed, single-center ACUDIN study was conducted between January 2012 and August 2018 at the HanseMerkur Center for Traditional Chinese Medicine at the University Medical Center Hamburg-Eppendorf, Germany (German Clinical Trial Registry No. DRKS00008562, https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00008562). Hypotheses were previously established. The study protocol was approved by the Ethics Committee of the Chamber of Physicians Hamburg, Germany (No. PV3518, 13 Jul 2011). Written informed consent was obtained from all patients. The study was carried out in accordance with the Declaration of Helsinki.
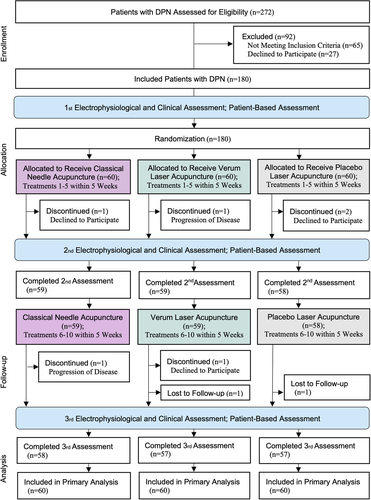
Figure 1 shows the ACUDIN study flowchart.
3 PARTICIPANTS
Participants were primarily recruited from regional outpatient centers. Additionally, 113 individuals (42% of a total of 272 potential participants) were recruited from the community by poster advertisements. Only patients with a confirmed history of type 2 diabetes and DPN including abnormal electrophysiological findings24 were assessed for eligibility. Patients were eligible if they were aged ≥18 years; presented with diabetes for ≥1 year; had a symptomatic symmetrical length-dependent sensorimotor DPN at the lower extremities, and showed abnormal results in NCS, sural sensory nerve action potential (SNAP) <10 μV, sural sensory nerve conduction velocity (SNCV) <42 m/s, tibial motor nerve conduction velocity (MNCV) <40 m/s, and tibial motor nerve action potential (MNAP) <8 mV).25 Exclusion criteria were neuropathies caused by other conditions, including alcohol abuse, chemotherapy, hereditary causes, and chronic inflammatory or idiopathic neuropathies; history of epilepsy; coagulopathies with prothrombin time < 40%; local bone fractures; local bacterial infections or skin lesions; analgesic or drug abuse; psychiatric illnesses; acupuncture in the last 3 months; pregnancy or breastfeeding; and incapacity or failure in giving informed consent. Current medications remained unchanged. Participants were offered 10 verum treatments free of charge after completion of the study if they were randomized to placebo.
4 RANDOMIZATION AND BLINDING
Patients were randomly assigned to receive either classical needle acupuncture, verum laser acupuncture, or placebo laser acupuncture with a parallel 1:1:1 allocation ratio using random four-digit numbers generated with Microsoft Office Excel 2007 (Microsoft Cooperation, Redmond, WA, USA). Allocation concealment was implemented by envelope lottery using opaque sealed envelopes containing the assigned information. Randomization was performed by study nurse 1 who was later exclusively involved in the process of verum laser and placebo laser acupuncture as described later. Randomization was unstratified and well balanced. Patients of all groups were informed that they would receive either verum or placebo treatment. Needle acupuncture was performed in single-blind mode, and verum laser and placebo laser acupuncture were performed in a double-blind procedure.23 For patient blinding, acupuncture situs and laser device were shielded from the patient. For caregiver blinding, the acupuncturist fixed the laser needles at the acupuncture points but did not operate the laser device before leaving the room. Study nurse 1 entered the room and operated the laser device according to the randomization schedule. Thus, study nurse 1 was the only person who had knowledge about patients' allocation to verum or placebo laser. Neurologists and statisticians were blinded to patients' group allocation. Neurological assessments were conducted at a separate neurological practice. Patients agreed not to disclose treatment information to the neurologist. For data transfer and processing, pseudonym codes were used in order to mask patient identity and treatment groups from outcome assessors and statisticians. Data were matched only after completion of statistical analysis.
5 INTERVENTIONS
The ACUDIN treatment concept was developed by acupuncture experts based on Traditional Chinese Medicine meridian theory and previously tested in a study for neuropathy of unknown cause.26 The bilateral acupuncture point selection consisted of two multiple local points, Ex-LE-10 (Bafeng)27 and Ex-LE-12 (Qiduan),27 and ST-34 (Lianqiu)27 with a total of 20 needles. According to Chinese medicine theory, Bafeng enhances the peripheral blood flow, Qiduan promotes local activation of Qi, and Lianqiu improves the Qi flow through meridians and Luo channels.27 This concept was standardized for all patients owing to a relatively even effect on local meridians caused by DPN.
All participants received 10 identical treatment sessions weekly for 10 consecutive weeks. Needle acupuncture was performed with sterile disposable stainless-steel needles 0.2 × 15 mm for Ex-LE-10 and Ex-LE-12, and 0.3 × 30 mm for ST-34, both manufactured by Wujiang City Cloud & Dragon Medical Devise Co. Ltd, China. After skin disinfection, needles were inserted perpendicularly to a depth of 0.2-0.3 cm at Qiduan, 0.8-1.2 cm at Bafeng, and 1.5-2.0 cm at Lianqiu. Depth varied with the thickness of the skin and subcutaneous tissues at the site of the acupuncture points. Needles remained in place for 20 minutes. They were then removed by a staff member not involved in further study procedures and disposed in puncture-resistant containers. Verum laser acupuncture was performed with two Laserneedle devices (European patent PCT/DE 102006008774.7) using multichannel semiconductor laser diodes for simultaneous acupoint stimulation. Activated diodes emitted a wavelength of 685 nm in continuous mode. Each channel provided an optical power of 35 mW. Power density was 2.3 kJ/cm2 per channel with a spot diameter of 500 μm.18 After local disinfection, laser needles were placed at an angle of 90° directly on the skin. With activation, laser radiation was emitted for 20 minutes, then deactivated automatically; laser needles were removed by a staff member not involved in further procedures. Placebo laser acupuncture was performed under identical conditions, but manipulating an invalid point on the laser device touch screen meant no laser light was emitted.
Acupuncturists are members of one registered German physicians society for acupuncture. They have completed a standardized training course, undertaken formal accreditation by examination, a period of supervised medical experience for administering interventions, and have been trained for the implementation of laser acupuncture.
6 OUTCOMES
Clinical assessments including NCS of bilateral sural and tibial nerves were performed by independently trained neurologists at baseline, following five treatment sessions at weeks 6 and 15. Primary endpoint was the change of SNAP from baseline to week 15 compared with placebo. Key secondary endpoints were changes of SNCV, MNCV, and MNAP compared with placebo. NCS were performed bilaterally with standard orthodromic needle recording methods25 for the sural nerve and standard orthodromic surface electrode recording methods25 for the tibial nerve with Neuropack-Sigma, MEB-9400, EMG/NCV/EP-System (Nihon-Khoden, Japan). Values of nerve conduction velocities were adjusted for the effect of skin temperature.
Additional secondary outcomes included clinical findings and PROMs. Clinical assessments included Achilles and patellar tendon reflexes, gait qualities, sensory qualities, for example, pain and temperature perception and pallesthesia, and DPN-related symptoms; neuropathic pain, numbness, burning and tingling sensations, muscle weakness, and cramps. Clinical findings were summarized according to the neuropathy disability score (NDS) and neuropathy symptom score (NSS).28 Further DPN-related symptoms were assessed by PROMs using 11-point numeric rating scale (NRS) questionnaires for neuropathic pain, impacts on daily activities and on sleep quality, and complaint frequency with the terminal descriptors “no complaint” and “worst complaint possible”.29 Patients were asked to complete the PROMs questionnaires, outlining changes of medication, including pain medication and possible adverse events at every appointment before the treatment or assessment session. Adverse events were categorized as treatment or nontreatment related and graded for severity.30 Glycosylated hemoglobin (GHb) levels were monitored at baseline and week 15.
7 STATISTICAL ANALYSIS
The null hypothesis was that the difference of sural SNAP from baseline to week 15 in the needle and laser acupuncture groups would be the same or smaller than in the placebo group. The alternative hypothesis was that the difference of SNAP would be larger in the needle and laser acupuncture groups than in the placebo group. An average difference of 1 μV was considered functionally relevant.31 Based on the previous case study,26 a sample size of 54 per group was estimated to detect the between-group difference of 1 μV with a SD of 1.83, an alpha of 0.05, and a power of 0.8. Assuming a conservative 10% dropout rate, the sample size was increased to 60 patients per arm, or 180 in total.
The primary endpoint was analyzed according to the intent-to-treat principle. Statistical analysis was done by one-way analysis of variance, followed by Tukey post hoc tests comparing the three groups pairwise. Homogeneity of variances was confirmed by Levene's test. P < .05 was regarded as statistically significant. Changes of SNAP were analyzed, evaluating the average values of each patient's legs. For unilateral results, only the evaluable leg was analyzed. Missing data were imputed by the next-observation-carried-backwards option for initial values and last-observation-carried-forwards option for closing values. Descriptive statistical analysis was used to characterize mean, SD, SE of the mean (SEM), variance, and range. The same approach was used for secondary endpoints. Data are presented as mean (SD) with 95% confidence interval (CI); figures show mean changes (SEM). Statistical analysis was conducted after completion of data collection. Data assessment was performed with SPSS (IBM SPSS Statistics 22) and OriginPro 9.
8 DATA AND RESOURCE AVAILABILITY
The datasets generated during the current study and the resources analyzed are available from the corresponding authors upon reasonable request.
9 RESULTS
We screened 272 patients for eligibility; 180 participants (aged 70 [10] years, 42-89 years; 80 [44%] females, 100 [55%] males) were randomly assigned to three groups of 60 participants each, that is, to needle acupuncture, laser acupuncture, or placebo laser acupuncture. Of these, 172 participants completed the study. Demographic baseline parameters, including gender, age, body mass index (BMI), duration of type 2 diabetes and DPN, GHb values, and severity of DPN-related signs and symptoms as measured by NDS and NSS, did not differ significantly between groups. Furthermore, demographic characteristics were not affected by recruitment methods. GHb values remained stable over the study period.
Table 1 summarizes participants' baseline characteristics.
| Placebo (n = 60) | Laser (n = 60) | Acupuncture (n = 60) | |
|---|---|---|---|
| Gender female/male (n [% per group]) | 24/36 (40/60) | 31/29 (52/48) | 25/35 (42/58) |
| Age (years) | 70 [8] | 72 [8] | 70 [10] |
| Body mass index (kg/m2) | 29.3 [5.1] | 28.7 [5.5] | 28.9 [4.6] |
| Duration of diabetes (years) | 10 [7] | 11 [8] | 12 [10] |
| Duration of DPN (years) | 6.26 [5.73] | 6.36 [4.88] | 6.85 [5.63] |
| GHb at baseline (% (mmol/mol) | 6.8 [0.9] (51 [10]) | 6.8 [0.7] (51 [8]) | 7.0 [1.0] (53 [11]) |
| GHb at week 15 (% (mmol/mol) | 6.8 [0.8] (51 [9]) | 6.8 [0.8] (51 [9]) | 7.0 [1.1] (53 [12]) |
| NDS at baseline | 7.98 [2.42] | 8.26 [2.31] | 8.07 [2.44] |
| NSS at baseline | 6.88 [1.54] | 7.15 [1.48] | 7.16 [1.50] |
- Note: Data presented as mean values [SD] unless indicated otherwise.
- Note: Baseline values did not differ significantly between treatment groups.
- Abbreviations: DPN, diabetic peripheral neuropathy; GHb, glycosylated hemoglobin; NDS, neuropathy disability score (mild = 3–5, moderate = 6–8, severe = 9-10 points); NSS, neuropathy symptom score (mild = 3–4, moderate = 5–6, severe = 7–10 points); n, number of participants.
10 PRIMARY OUTCOME
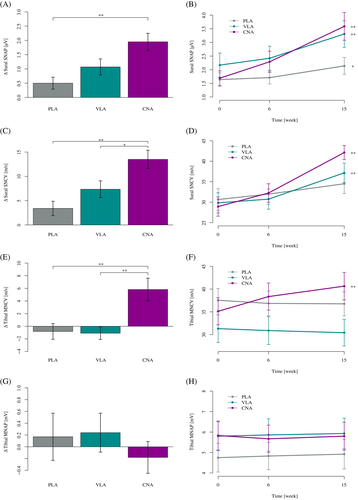
In the needle acupuncture group, the mean sural SNAP improved significantly from baseline to week 15 with a difference of 1.95 [2.36] μV, CI 95%, P < .001. In the laser acupuncture group, the mean sural SNAP improved significantly with a difference of 1.07 [2.21] μV, CI 95%, P < .001. In the placebo group, the mean sural SNAP improved significantly with a difference of 0.50 [1.62] μV, CI 95%, P = .016. The group comparison of mean sural SNAP at week 15 showed a significant difference of 1.45 μV, CI 95%, P < .001 between needle acupuncture and placebo, and a nonsignificant difference of 0.57 μV, CI 95%, P = .30 between laser acupuncture and placebo.
11 KEY SECONDARY OUTCOMES
In the needle acupuncture group, the mean sural SNCV improved significantly from baseline to week 15 with a difference of 13.49 [14.59] m/s, CI 95%, P < .001. In the laser acupuncture group, the mean sural SNCV improved significantly with a difference of 7.35 [13.32] m/s, CI 95%, P < .001. In the placebo group, the mean sural SNCV achieved a nonsignificant difference of 3.40 [11.5] m/s, CI 95%, P = .110. The group comparison of mean sural SNCV at week 15 showed a significant difference of 10.09 m/s, CI 95%, P < .001 between needle acupuncture and placebo, and a nonsignificant difference of 3.95 m/s, CI 95%, P = .23 between laser acupuncture and placebo.
In the needle acupuncture group, the mean tibial MNCV improved significantly from baseline to week 15 with a difference of 5.82 [13.52] m/s, CI 95%, P < .001. In the laser acupuncture group, the mean tibial MNCV achieved a nonsignificant difference of −0.10 [7.45] m/s, CI 95%, P = .63. In the placebo group, the mean tibial MNCV achieved a nonsignificant difference of −0.82 [9.44] m/s, CI 95%, P = .76. The group comparison of mean tibial MNCV at week 15 showed a significant difference of 6.64 m/s, CI 95%, P = .003 between needle acupuncture and placebo, and a nonsignificant difference of −0.27 m/s, CI 95%, P = .99 between laser acupuncture and placebo.
There were no significant changes of the mean tibial MNAP in any group at the P < .05 level.
Tables 2 and 3 summarize the results obtained by NCS. Figure 2 illustrates the results obtained by NCS.
| Baseline | Week 6 | Week 15 | Week 15–Baseline | |
|---|---|---|---|---|
| Placebo | ||||
| Sural SNAP (μV) | 1.64 [1.93] | 1.71 [1.82] | 2.14 [2.43] | 0.50 [1.62], P = .016 |
| Sural SNCV (m/s) | 30.65 [20.59] | 31.79 [19.38] | 34.05 [18.69] | 3.40 [11.5], P = .110 |
| Tibial MNCV (m/s) | 37.55 [20.05] | 36.86 [21.04] | 36.77 [20.48] | −0.82 [9.44], P = .76 |
| Tibial MNAP (mV) | 4.75 [5.41] | 4.83 [5.20] | 4.92 [5.60] | 0.17 [3.11], P = .90 |
| Laser | ||||
| Sural SNAP (μV) | 2.17 [3.45] | 2.42 [3.44] | 3.31 [3.78] | 1.07 [2.21], P < .001 |
| Sural SNCV (m/s) | 29.84 [19.11] | 30.74 [19.02] | 37.16 [18.38] | 7.35 [13.32], P < .001 |
| Tibial MNCV (m/s) | 31.31 [23.52] | 30.89 [23.74] | 30.42 [22.62] | −0.10 [7.45], P = .63 |
| Tibial MNAP (mV) | 5.80 [5.40] | 5.86 [6.11] | 5.93 [5.77] | 0.24 [2.51], P = .91 |
| Acupuncture | ||||
| Sural SNAP (μV) | 1.69 [2.13] | 2.29 [3.03] | 3.59 [3.97] | 1.95 [2.36], P < .001 |
| Sural SNCV (m/s) | 28.92 [18.22] | 32.24 [17.50] | 42.12 [13.40] | 13.49 [14.59], P < .001 |
| Tibial MNCV (m/s) | 35.13 [22.98] | 38.36 [23.05] | 40.65 [23.48] | 5.82 [13.52], P < .001 |
| Tibial MNAP (mV) | 5.83 [5.53] | 5.67 [5.18] | 5.80 [5.28] | −0.18 [2.11], P = .99 |
- Note: Data presented as mean values [SD], confidence interval 95%.
- Abbreviations: MNAP, motor nerve action potential; MNCV, motor nerve conduction velocity; SNAP, sensory nerve action potential; SNCV, sensory nerve conduction velocity.
| Acupuncture–Placebo | Laser–Placebo | Acupuncture–Laser | |
|---|---|---|---|
| Sural SNAP (μV) | 1.45, P < .001 | 0.57, P = .30 | 0.88, P = .058 |
| Sural SNCV (m/s) | 10.09, P < .001 | 3.95, P = .23 | 6.13, P = .032 |
| Tibial MNCV (m/s) | 6.64, P = .003 | −0.27, P = .99 | 6.92, P = .002 |
| Tibial MNAP (mV) | −0.35, P = .75 | 0.07, P = .99 | −0.42, P = .66 |
- Note: Data presented as mean values [SD], confidence interval 95%.
- Abbreviations: MNAP, motor nerve action potential; MNCV, motor nerve conduction velocity; NCS, nerve conduction studies; SNAP, sensory nerve action potential; SNCV, sensory nerve conduction velocity.
12 CLINICAL SCORES
The ACUDIN study population showed mean-moderate to severe stages of DPN of both NDS and NSS at baseline, which did not change significantly at the P < .05 level in any group.
Table 4 summarizes the results obtained from NDS and NSS.
| Placebo | Laser | Acupuncture | |
|---|---|---|---|
| NDS at baseline | 7.98 [2.42] | 8.26 [2.31] | 8.07 [2.44] |
| NDS at week 15 | 7.85 [2.32] | 8.0 [2.35] | 8.05 [2.30] |
| NDS week 15–baseline | −0.13 [2.09] | −0.25 [1.82] | −0.05 [2.02] |
| NSS at baseline | 6.88 [1.54] | 7.15 [1.48] | 7.16 [1.50] |
| NSS at week 15 | 6.57 [1.61] | 6.83 [1.60] | 7.10 [1.51] |
| NSS week 15–baseline | −0.32 [1.53] | −0.32 [1.72] | −0.05 [1.70] |
- Note: Data presented as mean values [SD].
- Abbreviations: NDS, neuropathy disability score (mild = 3–5, moderate = 6–8, severe = 9–10 points); NSS, neuropathy symptom score (mild = 3–4, moderate = 5–6, severe = 7–10 points). Neither NDS nor NSS changed significantly during the treatment.
13 PROMS
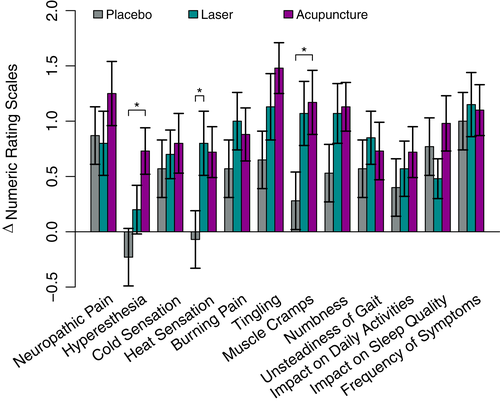
Patient-related outcomes showed significant changes from baseline to week 15 in all queried items induced by needle acupuncture, in 11 of 12 items induced by laser acupuncture, and in nine of 12 induced by placebo laser. Needle acupuncture induced the largest improvement in neuropathic symptoms, impact on daily activities, and sleep quality. Laser acupuncture induced the largest improvement in heat sensation, burning pain, unsteadiness of gait, and symptom frequency. Placebo laser induced the fewest changes. However, significant group differences were reached only for hyperesthesia and cramps in the needle acupuncture group and for heat sensation in the laser acupuncture group. PROMs improved in all groups without statistical differences at the P < .05 level.
Table 5 summarizes significant group differences obtained by PROMs. Figure 3 illustrates the overall results obtained by PROMs.
| Acupuncture–Placebo | Laser–Placebo | |
|---|---|---|
| Hyperesthesia (NRS) | 0.97, P = .007 | 0.43, P = .35 |
| Cramps (NRS) | 0.88, P = .047 | 0.78, P = .088 |
| Heat sensation (NRS) | 0.78, P = .056 | 0.87, P = .030 |
- Note: Data presented as mean values [SD], confidence interval 95%.
- Note: Significant group differences were reached for hyperesthesia and cramps in the needle acupuncture group and for heat sensation in the laser acupuncture group as compared with placebo. Further PROMs improved in all groups without statistical differences at the P < 0.05 level. Abbreviations: NRS, 11-point numeric rating scales; PROM, patient-reported outcome measures.
14 PATIENTS' ASSUMPTION OF TREATMENT ALLOCATION
Patients were asked if they received a verum or placebo treatment at the final assessment. In the acupuncture group, 39 patients (65%) estimated their intervention as active treatment, 15 (25%) deemed their intervention placebo, and six (10%) were indecisive. In the laser acupuncture group, 41 patients (68%) estimated their intervention as active treatment, 16 (27%) deemed their intervention placebo, and three (5%) were indecisive. In the placebo group, 28 patients (47%) estimated their intervention as active treatment, 25 (42%) deemed their intervention placebo, and seven (11%) were indecisive. Results did not differ statistically between the three groups.
15 DROPOUTS
Eight participants discontinued the treatment (two needle acupuncture, three laser acupuncture, three placebo patients). Two patients withdrew because of symptom progression, four declined to participate, and two were lost to follow-up.
16 ADVERSE EVENTS
Minor hematomas following needle acupuncture were observed in 13 of 60 patients (22%) with a total of 67 incidences in 589 treatment sessions (11%) without requiring medical intervention. Seven of 180 patients (4%) reported a temporary increase of neuropathic pain and decreasing hypoesthesia during the treatment course. All events were classified as mild.30
17 DISCUSSION
DPN is a common complication of type 1 and type 2 diabetes mellitus with severe clinical sequelae.1-10 Pharmaceutical management palliates neuropathic pain and paresthesia11 but does not address decreased nerve function. Furthermore, patients have to tolerate medication side effects.32 Longitudinal observations show a natural decline of sensory qualities and NCS values over time.33, 34 At present, there is no disease modifying therapy established for DPN.35 Recently, regenerative therapy approaches have achieved more attention.35, 36 Acupuncture is a promising complementary treatment, but its evidence is limited.12-14
The aim of the ACUDIN study was to quantify the effect of acupuncture on type 2 diabetes-induced DPN as compared with placebo. Laser acupuncture was implemented in the study to allow a double-blind treatment with an inert placebo procedure and thus avoid a noninert sham acupuncture for control.
Over a 15-week period, needle acupuncture induced significant improvement in the primary outcome variable sural SNAP and sural SNCV and tibial MNCV compared with placebo. Laser acupuncture induced improvement in both sural SNAP and SNCV compared with the baseline; however, it showed a later onset of effect compared with needle acupuncture and did not reach significance compared with placebo on completion of the study. Study design and power calculation were generated for needle acupuncture based on a prior case study.26 Laser acupuncture was implemented for the purpose of a double-blind comparison. Based on other publications,19, 20, 37 laser acupuncture was expected to yield equivalent effects to needle acupuncture. However, the results remained below those of needle acupuncture.
DPN affects primarily sensory rather than motor nerves.8 This was confirmed by fewer impaired baseline values and minimal, insignificant changes of tibial MNAP in all groups. Following needle acupuncture significant improvements could, compared with placebo, be demonstrated only for sural SNAP and SNCV and for tibial MNCV.
In a diabetic rat model, Pan et al38 demonstrated less impairment of sensory and motor nerve conduction velocities of the sciatic nerve in the electroacupuncture treatment group. Improved NCS values were accompanied by reduced myelinated nerve fiber damage and decreased proportions of cell apoptosis due to the ERS pathway, in comparison with a nontreatment group indicating structural enhancement. Our ACUDIN study confirms these findings on a clinical level. Because changes in nerve conduction studies are associated with neural fiber density differences,31 the observed improvement in NCS values indicates structural regeneration of nerve fibers. Hence, acupuncture might induce regenerative processes that could represent disease modification in DPN.
Clinical variables showed improvement in a number of subitems such as pain perception and localization of symptoms. However, NDS and NSS in total did not reach statistically significant changes during the study. Our study participants presented a mean age of 70 with a range of 42 to 89 years. Given that most patients suffered from progressed DPN and comorbidities including restrictions of mobility, we presume that higher clinical effects could be achieved in patients in earlier stages of DPN.
Tissue and nerve regenerative capacity has been shown to be decreased in diabetic patients.36 Acupuncture increases the blood flow in the extremities.39, 40 The selected acupoints at the distal end of the extremities27 were chosen to improve the perfusion of the vasa nervorum and dependent capillary beds supplying local neurons.40 Shin et al41 demonstrated a positive effect of electroacupuncture on painful DPN, using distal acupuncture points (Bafeng) as facultative points. All obligatory points were located proximal to the toes. There was a significant decrease in pain intensity as measured by NRS but no changes in NCS. However, in the ACUDIN protocol, points located at the toes were obligatory (Bafeng and Qiduan). This approach resulted in significant changes in NCS values, suggesting that local microcirculatory effects could be the predominant mechanism of acupuncture-induced peripheral nerve repair, combined with modulation of cortical network connectivity contributing to the analgesic effect.42 In this context, needle acupuncture may represent a stronger stimulus than laser acupuncture.
Mild adverse events confirm that professionally administered local acupuncture is a safe treatment procedure in DPN conditions.
PROMs showed superior effects of needle acupuncture to placebo in all 12 variables and of laser acupuncture in 10 of 12 variables, reaching significance for hyperesthesia and cramps following needle acupuncture and for heat sensation following laser acupuncture. Because these are pain-related symptoms, our results provide evidence for the value of acupuncture in pain therapy in DPN. Hyperesthesia and heat sensation can be signs of C-nociceptor hyperexcitability caused by fiber degeneration and alterations in channel expression,43 producing orthodromic and antidromic conduction and multiplication of spontaneously generated nerve impulses and receptor threshold reduction.44 Moreover, severity of muscle cramps in DNP correlates with small and large fiber measures.45 Hence, clinical improvement can be a sign of fiber repair,31 corresponding to positive NCS results in our study.
Nevertheless, PROMs showed fewer distinct group differences than NCS results together with a higher evidence for placebo effects. This indicates the necessity to measure acupuncture effects by variables less susceptible to placebo, such as NCS.
Effects measured by NCS were more pronounced after 15 weeks compared with 6 weeks in an overproportional manner for both needle acupuncture and laser acupuncture. Hence, prolonged treatment protocols may induce further nerve regeneration and may be essential for better group distinctions of PROMs.
18 LIMITATIONS
The ACUDIN study had some limitations. First, data were obtained for patients with type 2 diabetes. The transferability of these results to patients with type 1 diabetes has to be further evaluated. Second, there is no reliable direct but inactive placebo control available for needle acupuncture, requiring an indirect pathway for double-blinding the procedure via laser acupuncture. Third, power calculation could be performed for needle acupuncture but not for laser acupuncture. This may have contributed to the disparity of needle and laser acupuncture results. Fourth, long-term treatment efficacy and mechanisms of action were not investigated.
19 CONCLUSIONS
The ACUDIN trial showed significant effects of acupuncture as compared with placebo on type 2 diabetes-induced DPN after 10 acupuncture sessions. Improvement in the primary outcome variable sural SNAP amplitude indicates structural neuroregeneration following acupuncture. This is of major importance because there have been, as yet, no disease modifying therapies for DPN. Furthermore, acupuncture applied at the lower extremities is a safe treatment in DPN. Electrophysiologically quantified data showed clearer group distinctions than PROMs. Effects detected by NCS increased with time in a linear manner, suggesting that prolonged acupuncture protocols may be necessary for better results of PROMs, which should be examined in future studies.
20 ACKNOWLEDGMENTS
The authors gratefully acknowledge the valuable contributions from the participants with DPN; from Andreas Bey and Antje Ziegs, outpatient clinic for Neurology Jarrestadt for data collection through neurological investigation. The ACUDIN trial was financially supported during the clinical phase by the Innovation Foundation, Hamburg (721.230-002) and the HanseMerkur Insurance Group, Hamburg. Laser devices were provided by Laserneedle GmbH, Glienicke/Nordbahn, Germany. Open access funding enabled and organized by Projekt DEAL. Open access funding enabled and organized by Projekt DEAL.
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
SVS had the original idea for the ACUDIN trial and is the guarantor of this work. As such, he had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. However, he remained blinded to patients' group allocation until completion of the statistical analysis. SVS and CG are responsible for the study design, definition of primary and secondary outcomes, and preparation of the trial protocol. TF is responsible for sample size calculation and statistical analysis. SVS performed neurological assessments including nerve conduction studies. SVS and JG contributed to the determination of acupuncture point selection. GMH performed the participants' enrollment and study treatments and wrote the manuscript. All authors have critically reviewed and approved the final version of the manuscript.