Direct oral anticoagulants versus aspirin for primary thromboprophylaxis in patients with multiple myeloma undergoing outpatient therapy: A systematic review and updated meta-analysis
Summary
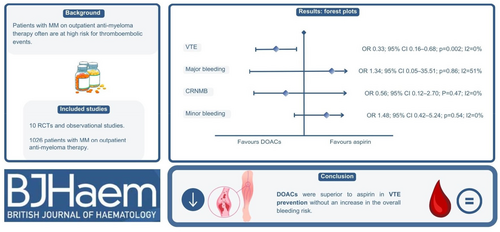
Patients with multiple myeloma (MM) are at an elevated risk of venous thromboembolism (VTE), which is further increased for those undergoing anti-myeloma therapy. Current guidelines suggest low-dose direct oral anticoagulants (DOACs) as an alternative to aspirin for primary thromboprophylaxis in this population, but data comparing these two therapies are limited. We performed a systematic review and meta-analysis to compare DOACs with aspirin for primary thromboprophylaxis in individuals undergoing outpatient anti-myeloma therapy. Studies were selected when comparing DOACs versus aspirin for thrombotic and haemorrhagic outcomes. We included 10 randomised controlled trials and observational studies comprising 1026 patients with MM who received primary thromboprophylaxis with DOACs (n = 337) or aspirin (n = 689). DOAC thromboprophylaxis was associated with a significantly lower incidence of VTE compared with aspirin (OR 0.33; 95% CI 0.16–0.68; p < 0.001). Major, clinically relevant non-major and minor bleeding event rates did not differ significantly between groups. Overall, our meta-analysis suggests that DOACs may be a preferable option to aspirin for the prevention of MM-related thrombosis. However, these results should be interpreted in the context of heterogeneous baseline population characteristics and potential bias from including observational studies. Further research is needed to evaluate the optimal thromboprophylaxis strategy, particularly in high-risk individuals.
Graphical Abstract
Patients with multiple myeloma (MM) undergoing disease-directed therapy are at an increased risk of venous thromboembolism (VTE) compared to the general population. In this setting, current guidelines suggest low-dose direct oral anticoagulants (DOACs) as an alternative to aspirin for primary thromboprophylaxis. Our systematic review and meta-analysis of selected randomised controlled trials and observational studies demonstrated a reduced occurrence of VTE with DOACs in comparison to aspirin, with no associated rise in bleeding events. However, these results should be interpreted with caution, considering the heterogeneous baseline population characteristics and potential biases/confounders from observational studies. Further research is essential to determine the optimal thromboprophylaxis strategy, especially for high-risk individuals.
CONFLICT OF INTEREST STATEMENT
A.R. has received advisory board fees from Celgene/Bristol Myers Squibb, Janssen, Sanofi and GlaxoSmithKline. The remaining authors have no conflicts of interest to disclose. All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Open Research
DATA AVAILABILITY STATEMENT
Because this meta-analysis was based on data extracted from previously published research, all of the data and study materials are available in the public domain. The authors of this meta-analysis do not have access to patient-level data of the individual studies. Researchers interested in individual-level data from the studies included in this meta-analysis are encouraged to contact the corresponding author from each individual study for such requests.