Cutaneous balloon-cell melanoma metastases to the axillary lymph node: Exploring cytomorphologic features and differential diagnoses on fine needle aspiration biopsy
Abstract
Balloon cell melanoma (BCM) is an exceptionally uncommon histological variant, making up <1% of all malignant melanomas. Diagnosing balloon cell melanoma on cytological specimens can be challenging due to its scarcity and its similarity to other medical conditions. A comprehensive clinical assessment and histological analysis, coupled with immunohistochemical staining, play a crucial role in distinguishing balloon cell melanoma from various benign and malignant skin conditions. The differential diagnoses encompass spitz nevus, balloon cell nevus, clear cell sarcoma of tendons and aponeuroses (melanoma of soft tissues), metastatic clear cell renal cell carcinoma, sebaceous carcinoma, and benign adnexal tumours like clear cell hidradenoma.
Malignant melanoma encompasses a spectrum of histopathological subtypes, each with unique clinical and cytological characteristics. Notably, balloon-cell melanoma (BCM) emerges as an exceptionally rare and diagnostically challenging variant. Marked by the presence of distinct balloon-like, clear cytoplasmic vacuoles within melanoma cells, BCM stands apart from other melanoma subtypes. Despite its rarity, the distinctive cytological features of BCM make it a compelling subject of investigation, emphasizing the crucial role of Fine Needle Aspiration (FNA) cytology in ensuring accurate diagnosis and guiding subsequent management decisions.
1 CASE PRESENTATION
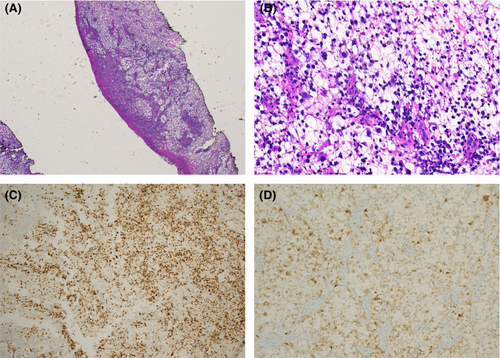
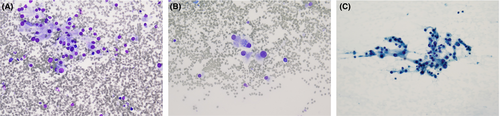
An 81-year-old male presented with a concerning skin lesion on his right thumb. The lesion had been causing pain, and bleeding, and had been progressively enlarging over time (Figure 1). A shave biopsy of the lesion and expression of Melan A and S100 is depicted in Figure 2A–D. Three years and a half following the initial diagnosis, the patient returned with a new concern of an enlarged right axillary lymph node. A fine needle aspiration (FNA) was performed. Diff Quik staining demonstrates epithelioid foamy cells with round to ovoid eccentrically located nuclei with low nuclear to cytoplasmic ratio (Figure 3A,B). Pap smear-stained slide demonstrates sheets of cohesive, large, and spindle-shaped foamy cells with abundant cytoplasm and a low nuclear to cytoplasmic ratio. No pigmentation was present (Figure 3C).

2 QUIZ
- What is your diagnosis?
- Clear cell hidradenoma
- Spitz nevus
- Balloon cell melanoma
- Metastatic clear cell renal cell carcinoma
- Clear cell sarcoma of tendons and aponeuroses (melanoma of soft tissues)
- What is the most useful immunohistochemical staining workup for the presented case?
- S-100, HMB-45, and Melan-A, PAX8
- CD34, D2-40, PAX8
- Cytokeratin, epithelial membrane antigen (EMA), desmin, myoglobin, smooth muscle actin
- Vimentin, CD99, NSE
- What are the significant prognostic factors in the presented case?
- The balloon cell variant confers a worse prognosis and adverse patient outcomes.
- Lymph node involvement is associated with an unfavourable prognosis when compared to internal organ involvement.
- Tumour thickness, higher stages T2-4, and positive surgical margins
- Ki67 proliferation rate index
ANSWERS TO THE QUIZZES
1. c. Balloon cell melanoma (BCM) is an exceptionally uncommon histological subtype, representing less than 1% of all malignant melanomas. It is characterized by the presence of balloon-like, clear cytoplasmic vacuoles within melanoma cells. The nuclei within may often display cellular atypia, nuclear enlargement, irregularity, and hyperchromasia. Furthermore, BCM may contain varying amounts of melanin pigmentation, presenting as granules or pigmentary inclusions within the vacuolated cytoplasm.
2. a. The utility of melanocytic markers such as S-100, HMB-45, and Melan-A is crucial for establishing a diagnosis of metastatic melanoma. PAX8 and CAIX are valuable for diagnosing clear cell renal cell carcinoma.
3. c. Tumour thickness and positive margins are often associated with an increased risk of distant metastasis and disease progression. The initial sampling exhibited a diagnosis of balloon cell melanoma with a minimum Breslow thickness of at least 0.41 mm. The risk of metastatic melanoma is higher in patients with cutaneous melanomas with increased thickness and higher stages of the disease (thickness of ≥1.0 mm, and higher stages T2-4). The outcome of metastatic melanoma is influenced by various factors, such as the stage of the disease, distant metastatic spread, and whether the primary melanoma originated on the skin or in non-cutaneous sites. Generally, metastasis to regional lymph nodes is associated with a favourable prognosis when compared to metastasis to internal organs.
3 DISCUSSION
Metastatic melanoma is a highly aggressive and potentially life-threatening form of cutaneous malignancy characterized by the spread of melanoma cells from the primary tumour site to distant organs or lymph nodes. In general, cutaneous metastases typically occur close to the primary tumour site with an often occurrence on the head and neck region and the extremities. Common extracutaneous sites of melanoma metastasis include the lymph nodes, lungs, liver, bones, central nervous system, and less frequently the gastrointestinal tract, kidneys, adrenal glands, and thyroid gland. Metastases of melanoma may occur via lymphatic, hematogenous, or perineural routes. The risk of metastatic melanoma is higher in patients with cutaneous melanomas with increased thickness and higher stages of the disease (thickness of ≥1.0 mm, and higher stages T2-4).
Balloon cell melanoma (BCM) is an exceedingly rare histological variant, accounting for <1% of all malignant melanomas.1 Its rarity presents a significant diagnostic challenge, mainly because it shares morphological characteristics with various other clear cell neoplasms, such as clear cell sarcoma, metastatic clear cell carcinomas, and malignant histiocytic neoplasms like xanthoma and atypical fibroxanthoma.2 This overlap in features underscores the importance of accurate diagnosis. Clinically, BCM often manifests as a subtle flesh-coloured, non-pigmented nodule or plaque.
This inconspicuous presentation may lead to delays in diagnosis, as it may not raise immediate suspicion compared to its pigmented melanoma counterparts. Balloon cell features have been described in the literature in various cases of metastatic melanoma. Recognizing these subtle clinical clues is vital for early detection and appropriate management.
Fine-needle aspiration biopsy (FNAB) cytology emerges as a crucial diagnostic tool, offering a minimally invasive means to aid in the identification of various variants of malignant melanoma. FNAB allows for the direct visualization of distinctive epithelioid cells characterized by their foamy clear cytoplasmic vacuoles, a hallmark feature of BCM. These vacuoles can vary in size and distribution, imparting a distinctive ‘balloon-like’ appearance to the cells. The nuclei often exhibit cellular atypia, nuclear enlargement, irregularity, and hyperchromasia. Additionally, BCM may contain variable amounts of melanin pigmentation, which can manifest as granules or pigmentary inclusions within the vacuolated cytoplasm.
In the presented case, due to these alarming symptoms of a rapidly enlarging thumb lesion, a shave biopsy of the lesion was performed to determine its nature and potential malignancy. A shave biopsy revealed the presence of spindle-shaped pleomorphic neoplastic cells with foamy and clear cytoplasm with a ‘balloon cell’ appearance comprising more than 80% of the tumour cells. A mitotic rate was 0 mitoses/mm2. Tumour cells extended to the lateral and deep margins. Immunohistochemical staining exhibited the positive expression of Melan A and S100. Figure 2A–D. Three years and a half following the initial diagnosis, the patient returned with a new concern of an enlarged right axillary lymph node. A fine needle aspiration (FNA) was performed. pap-stained smears from the axillary lymph node fine-needle aspiration effectively revealed the nuclear features characteristic of balloon cell melanoma, including anisonucleosis, round to ovoid eccentrically located nuclei, and prominent nucleoli. The Diff-Quik stain was particularly useful in highlighting the cytoplasmic features, such as distinct cell margins and finely dispersed, sharply delineated clear vacuoles. Although no pigmentation was observed, suspicion of melanoma arose during the comparison with a previously shaved biopsy specimen of the thumb lesion. To confirm the diagnosis of balloon cell melanoma, a comprehensive approach involving various ancillary methods was employed. Immunocytochemistry revealed S-100 and Melan A positivity consistent with metastatic melanoma.
On histopathological examination, BCM typically demonstrates an infiltrative growth pattern, with extensions into the dermis or subcutaneous tissue. While immunohistochemical stains like S-100, HMB-45, and Melan-A are often used to aid in melanoma diagnosis, metastatic melanoma may not consistently express these markers. This inconsistency further complicates the identification of BCM and underscores the importance of FNAB cytology in its accurate diagnosis.
The diagnosis of balloon cell melanoma can be challenging due to its rarity and resemblance to other conditions. A thorough clinical evaluation and histological examination, along with immunohistochemical staining aid in the differentiation of balloon cell melanoma from other benign and malignant skin lesions. The main differential diagnoses include spitz nevus, balloon cell nevus, clear cell sarcoma of tendons and aponeuroses (melanoma of soft parts), metastatic clear cell renal cell carcinoma, sebaceous carcinoma, and benign adnexal tumours such as clear cell hidradenoma (refer to Table 1 for detailed differential diagnosis).
| Diagnosis | Features | Cytomorphologic features | Immunohistochemical Staining |
|---|---|---|---|
| Balloon cell melanoma | Rare variant of malignant melanoma, challenging diagnosis with lymph node metastasis5; clear cytoplasm with nuclear atypia; may contain melanin pigmentation | Distinctive epithelioid cells are characterized by their foamy clear cytoplasmic vacuoles, a hallmark feature of BCM. These vacuoles can vary in size and distribution, imparting a distinctive ‘balloon-like’ appearance to the cells. The nuclei often exhibit cellular atypia, nuclear enlargement, irregularity, and hyperchromasia. Additionally, BCM may contain variable amounts of melanin pigmentation, which can manifest as granules or pigmentary inclusions within the vacuolated cytoplasm | Immunohistochemistry aids in differentiation; melanocytic markers include S100, HMB-45, Melan-A |
| Spitz Nevus6 | Spitz nevi are benign neoplasms composed of large epithelioid or spindled melanocytes. Primary affects young adults.7 |
Rare on cytology specimens. Melanocytes exhibit a substantial size, appearing either spindled or epithelioid, with cytoplasm that is abundant, pale, or has a ground glass texture. If melanin pigment is present, it is finely dispersed within the cytoplasm There might be mild nuclear pleomorphism, and the occurrence of mitoses is infrequent or absent |
S100, MART1/MelanA, SOX10 HMB45, Ki67 proliferation index is low, p16, ALK, ROS, NTRK (in spitz nevus with fusions involving ALK, ROS or NTRK).8, 9 Non-reactive stains to cytokeratin, SMA, EMA, and BRAF |
| Melanocytic nevus with balloon-cell changes10, 11 | Resembles balloon cell melanoma; lacks cellular atypia. Maybe a precursor to malignant melanoma | Resembles balloon cell melanoma; lacks cellular atypia | Immunohistochemistry may include melanocytic markers for confirmation. S100, MART1/MelanA, SOX10 HMB45, Ki67 proliferation index, and p16 |
| Clear Cell Sarcoma of Tendons and Aponeuroses (Melanoma of Soft Parts) | Aggressive soft tissue sarcoma; uniform epithelioid and spindle cells with clear to eosinophilic cytoplasm; melanocytic characteristics; EWSR1-ATF1/CREB1 rearrangement | Uniform epithelioid and spindle cells with clear to eosinophilic cytoplasm | Immunohistochemical staining for melanocytic markers, EWSR1, and ATF1/CREB1 |
| Sebaceous Carcinoma12 | A malignant neoplasm with sebaceous differentiation is typically categorized into periocular and extraocular types. Classified into well-differentiated and poorly differentiated carcinoma |
Well-differentiated sebaceous carcinoma is characterized by the presence of mature sebocytes, exhibiting multivacuolated cytoplasm and nuclear indentation compared to basaloid undifferentiated cells. It displays mild pleomorphism, minimal mitotic activity, and lacks necrosis In contrast, moderately to poorly differentiated sebaceous carcinoma demonstrates an increased proportion of atypical basaloid (undifferentiated) cells with limited differentiation towards multivacuolated cells. Prominent pleomorphism, significant atypia, frequent mitotic figures, and necrosis are hallmarks of this stage |
Immunostaining for adipophilin, Ber-EP4, and EMA; high molecular weight cytokeratin |
| Clear Cell Hidradenoma13 | Benign adnexal tumour; clear cytoplasm; ductal and myoepithelial differentiation | Clear cytoplasm; ductal and myoepithelial differentiation | Positive staining for AE1 / AE3, EMA, and CEA, and p63 |
| Metastatic Clear Cell Renal Cell Carcinoma14 | Skin involvement resembling balloon cell melanoma; clinical history and immunohistochemical staining needed for differentiation | Clusters of relatively uniform cells with pale cytoplasm are interspersed with stromal components, capillaries, and necrosis. Well-defined cell membrane cells with round centrally or eccentrically located nuclei. High-grade cases exhibit prominent nucleoli, and intranuclear vacuoles are frequently observed. The cytoplasm appears pale, vacuolated, or granular. | Immunostaining for renal markers (CD10 and PAX8); negative for melanocytic markers; negative for p63 |
Spitz nevi is a benign melanocytic tumour that can have large, round, or polyhedral balloon cells in their histological appearance. The lack of cellular atypia seen in spitz nevus is crucial for differentiation.
Clear cell sarcoma of tendons and aponeuroses (melanoma of soft parts) is characterized by uniform epithelioid and spindle cells featuring clear to eosinophilic cytoplasm, notable for its melanocytic characteristics and the presence of EWSR1-ATF1/CREB1 rearrangement. Cellular smears exhibit a high cellular density, primarily comprising individual or ‘arranged in clusters’ uniform epithelioid or polygonal cells, often alongside spindle-shaped cells with prominent nucleoli. The cytoplasm is notably vacuolated, presenting well-defined boundaries. Approximately half of the cells may feature binucleation or multinucleation, while around 10% display focal intracytoplasmic pigment.
Well-differentiated cases of sebaceous carcinoma are characterized by an increased proportion of mature appearing sebocytes, characterized by their multivacuolated cytoplasm, mild pleomorphism, and minimal mitotic activity and necrosis. On the other hand, moderately to poorly differentiated cases, have a higher proportion of atypical basaloid cells with limited differentiation towards multivacuolated cells, prominent pleomorphism and atypia, frequent mitotic figures, and necrosis.
In rare cases, metastatic renal cell carcinoma can involve the skin and appear histologically like balloon cell melanoma. Clinical history and additional immunohistochemical staining may help differentiate between these two entities.
Certain benign tumours originating from skin adnexal structures (such as sweat glands or sebaceous glands) may have balloon cell changes, but they generally lack the malignant features of melanoma such as clear cell hidradenoma.
The prognosis of metastatic melanoma hinges on several factors, including the disease stage, the extent of metastatic involvement, and the primary site of melanoma (cutaneous or noncutaneous).3 Metastasis to regional lymph nodes generally carries a more favourable prognosis compared to metastasis to visceral organs.4
4 CONCLUSION
Balloon-cell melanoma is a rare and represents a diagnostically challenging variant of malignant melanoma. Essential cytomorphological features, includes clear cytoplasmic vacuoles, nuclear atypia, and variable melanin pigmentation. While BCM may resemble other benign and malignant clear cell neoplasms, FNAB cytology plays a pivotal role in its accurate diagnosis, facilitating early diagnosis and timely clinical management. This article emphasizes the significance of recognizing the cytological characteristics of BCM in the context of melanoma diagnosis and management.
AUTHOR CONTRIBUTIONS
Nada Shaker: Conceptualization; Data curation; Writing—original draft; Writing—review & editing; Zaibo Li: Conceptualization; Writing—review & editing; Judith Bamporiki: Conceptualization; Writing—review; Omar P. Sangueza: Conceptualization; Writing—review & editing; Abdul Abid: Conceptualization; Data curation; Writing—original draft; Writing—review & editing.
ACKNOWLEDGEMENTS
Authors acknowledged the manuscript submission.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
Data is available upon response from the corresponding author.