Determination of the minimally important difference in a nasal symptom score in house dust mite allergy
Abstract
Background
House dust mite (HDM) allergens are responsible for the most prevalent persistent respiratory allergies. Clinical trials in this field often use a four-component nasal symptom score (T4NSS) as a measure of efficacy.
Methods
The present observational, prospective, multinational, multicenter study determined the minimal important difference (MID) for a T4NSS in children, adolescents, and adults with physician-diagnosed HDM-induced allergic rhinoconjunctivitis (AR). Patients rated the T4NSS daily, a 15-point global rating of change scale (GRCS) and the Rhinoconjunctivitis Quality of Life Questionnaire weekly. The MID was determined primarily by using a regression method with a GRCS threshold of 2.
Results
A total of 546 patients (210 adults, 133 adolescents, and 203 children) were included; 92.6% of the patients had moderate-to-severe AR, and 30.1% had concomitant mild asthma. During the first week, the mean ± standard deviation T4NSS was 5.68 ± 2.76 in adults, 5.34 ± 2.66 in adolescents, and 5.07 ± 2.48 in children. In a GRCS regression analysis, the MID [95% confidence interval] for the T4NSS was −0.90 [−1.06;-0.75] overall (n = 509), −0.94 [−1.19;-0.69] in children (n = 187), −0.74 [−1.07;-0.41] in adolescents (n = 125), and −1.04 [−1.29;-0.79] in adults (n = 197). The MID did not differ greatly from one disease severity tertile to another. Confirmatory distribution-based analyses yielded overall MID values of −0.87 for the first week of the study and −0.93 for the week 2–week 1 difference.
Conclusion
The MID for improvement in the T4NSS is at least −0.90 units in children, adolescents, and adults suffering from HDM-induced AR This value could be rounded up to −1 unit for convenience.
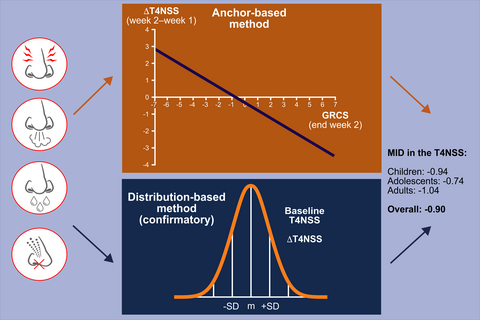
Graphical Abstract
In patients with house dust mite allergic rhinoconjunctivitis, the minimal important difference for improvement in a four-item nasal symptom score was at least 0.9 units. This value was estimated in children (n=187), adolescents (n=125), and adults (n=197) by both regression analyses using anchors and distribution-based analyses using the standard deviation (SD). The anchors in the regression analyses were either a 15-point global rating of change scale or the age-specific Rhinoconjunctivitis Quality of Life Questionnaires.
CONFLICT OF INTEREST
P. Devillier has received consulting fees, honoraria for lectures, and/or research funding from GlaxoSmithKline, AstraZeneca, Chiesi, Novartis, ALK, Meda Pharma, and Stallergenes. KC. Bergmann has received consulting fees, honoraria for lectures, and/or research funding from AstraZeneca, Lofarma, ALK, Novartis, Sanofi, Bencard, HAL, Allergopharma, Stallergenes, and HAL. H. Brüning has received consulting fees, honoraria for lectures, and/or research funding from Stallergenes GmbH.