Thoracic Cancer Exercise Services in Australia: A Point-Prevalence Survey
Funding: The authors received no specific funding for this work.
ABSTRACT
Background
Cancer guidelines recommend pre- and rehabilitation; however, current research shows these services are not well integrated into clinical practice. To date, there has been no prospective audit of Australian lung cancer exercise services or the people accessing these services. The aim of this study was to describe the exercise pre- and rehabilitation services available to people with thoracic cancer and the characteristics of people with thoracic cancer attending these services in Australia.
Methods
Prospective, observational, multicenter, 5-day, point-prevalence study. Australian healthcare services likely to provide exercise services to people with thoracic cancer were contacted to participate. Conduct and reporting followed the CROSS guidelines.
Results
A total of 397 services were contacted, and 203 responded (51%). Overall, 67% (n = 137) accepted thoracic cancer referrals, and 107 (78%) completed the survey. Most exercise services were targeted at respiratory disease (58%, n = 60) compared with 31% cancer-specific (n = 33) and 5% lung cancer-specific (n = 5). A total of 73 patients with thoracic cancer attended programs across 41 sites (38%). Mean (SD) age was 68.5 (9.7) years. Overall, 4% of patients (n = 3) were culturally and linguistically diverse, and none identified as Aboriginal or Torres Strait Islander. A total of 19 outcomes were used in 51 combinations to assess participants (n = 70), and 12 exercise interventions were delivered in 45 combinations (n = 67).
Conclusions
One-third of responding exercise programs did not offer exercise services to people with thoracic cancer. Almost two-thirds of services that accept referrals did not have a thoracic cancer patient attend their service. High heterogeneity in outcome measures and exercise interventions was observed.
1 Introduction
Lung cancer is the leading cause of cancer mortality and morbidity in Australia [1]. High symptom burden in people with lung cancer contributes to functional decline and reduced quality of life, with unmet physical and psychological care needs linked to worse outcomes compared to unmet emotional, informational, and spiritual needs [2, 3]. Exercise interventions have been shown to decrease symptom burden, minimize treatment side effects, and improve physical functioning and health-related quality of life across the lung cancer-care continuum [4]. Heterogeneity in exercise modalities, intensity, frequency, and duration complicates the ability to draw consistent conclusions across studies [4]. Data on exercise interventions provided in surgical lung cancer patients suggest that this heterogeneity also exists in clinical practice [5]. Data are not currently available for non-surgical lung cancer patients.
Optimal Lung Cancer Care Pathways are evidence-based standards of care developed to ensure the provision of standardized person-centered care for people with lung cancer. These pathways recommend pre- and rehabilitation to enhance the patient experience and performance status across the cancer care continuum [6]. Despite recommendations, Australian survey data show a gap between what is recommended in the evidence base and clinical practice [5]. A survey conducted with oncology physiotherapy services in Australia reports low availability across all cancer types, with approximately half (54%) of surveyed services accepting referrals for people with lung cancer [7]. More specifically in lung cancer, a recent survey reports that 11% (n = 8) and 55% (n = 39) of 70 responding services in Australia or New Zealand offered an exercise program to people with lung cancer in the pre- and postoperative setting, respectively [5]. Although these studies offer valuable insights into available exercise programs, they lack comprehensive reporting of the uptake of community-based exercise services by lung cancer patients across the cancer continuum. In addition to limited services, lung cancer clinical trials and qualitative research show that physical activity levels and exercise engagement in people with lung cancer are influenced by program cost support from caregivers and relatives, in addition to exercise program location and method of delivery, that is, home or clinic visit [8, 9].
Significant variation and gaps in lung cancer care and outcomes exist both internationally and within Australia. Social determinants of health are nonmedical factors that influence a person's health outcomes [10]. Current data show that people living in remote or rural locations, with lower socioeconomic status and identifying as Indigenous, are more likely to be diagnosed with lung cancer and have poorer outcomes, including reduced 5-year survival [1, 11]. Longitudinal data collected from national surveys of the general population report that lower income, unemployment, a lower education level, and living in a lower sociodemographic area are associated with lower levels of physical activity [12, 13]. Participant social determinants of health and the impact of these factors on physical activity or exercise program engagement are rarely reported in exercise clinical trials in lung cancer.
To date, there has been no point–prevalence audit of Australian exercise services for people with thoracic cancer, managed surgically or nonsurgically, across all stages of the care continuum (from prehabilitation to survivorship). Point-prevalence surveys are cross-sectional and capture the prevalence of an intervention over a specific period of time, minimizing the potential for recall bias; hence, are more likely to provide a more accurate representation of prevalence compared to studies with extended timeframes [14]. Data are required to identify current care gaps and variations in exercise service delivery for patients with thoracic cancer to inform areas in need of future service implementation.
The aim of this study was to describe the current Australian exercise services available to people with thoracic cancers. Secondary aims were to understand the characteristics of the health professionals providing these services, the characteristics of people with thoracic cancers attending an exercise program, and the outcomes and interventions used within these services.
2 Methods
2.1 Study Design
A prospective, observational, multicenter, longitudinal (5-day), point-prevalence study was conducted between March 20 and 24, 2023 using Qualtrics, a secure online database hosted by the University of Melbourne. The 5-day period selected for the point-prevalence study was deemed representative of typical practice, as intervention frequency has been reported to vary between 1 and 5 days per week in exercise trials [4]. Furthermore, the dates selected avoided overlap with Australian holiday periods and circumvented peak seasonal conditions that may influence attendance.
The survey was divided into two sections relating to exercise services and exercise health professional characteristics and patient, outcome, and intervention characteristics. Postcodes were collected for all thoracic cancer exercise services and patients to enable the researchers to determine remoteness area per Australian Statistical Geography Standard Remoteness Structure [15] and socioeconomic advantage per Index of Relative Socio-Economic Disadvantage (see Supporting Information section 1) [16]. The survey contained between 6 and 39 questions depending on answers provided and is attached in Supporting Information section 2. The first section was completed once per responding exercise service, whereas the second section was completed once for each person with lung cancer who attended the exercise service during the point-prevalence period. The survey was trialed by two oncology physiotherapists working at two different outpatient departments offering exercise services to people with lung cancer. Both physiotherapists provided feedback on question clarity and recorded the time of completion. The study was reported in accordance with the Consensus-Based Checklist for Reporting of Survey Studies [17].
2.2 Participants and Recruitment
Eligible participants were exercise health professionals who worked at an Australian healthcare site at the time of the survey that provided exercise services to people who have received a confirmed diagnosis of thoracic cancer (non-small cell lung cancer, small cell lung cancer, or mesothelioma) at any timepoint on the cancer care continuum (prior to, during, and posttreatment) in the outpatient setting (center or home-based).
To determine potentially eligible participants, a comprehensive list of healthcare services likely to provide exercise services to people with thoracic cancer was generated from thoracic cancer health services and respiratory and oncology exercise services. This was achieved by searching for health services with a lung cancer multidisciplinary meeting or performing thoracic surgery, in addition to exercise health services listed on a cancer exercise online toolkit [18] and the Lung Foundation Australia exercise program providers list [19]. A manager or clinical lead at each site was contacted by email and asked to confirm service eligibility and provide the contact details of a single clinician within their organization to complete the survey. Four email reminders were sent to nonresponders. The study details were also advertised on social media platforms using accounts of the study researchers to reach additional healthcare sites that may not have been included in contact lists. In attempts to minimize selection bias, study details were advertised across multiple platforms and were shared on relevant interest group pages.
When used within this study, the term “healthcare service” refers to all healthcare sites that were contacted to be included in the study, in addition to sites that contacted the research team following social media advertisement. The term “thoracic cancer exercise service” refers to healthcare services that provide exercise assessment and intervention to people with thoracic cancer. The term “exercise professional” refers to any exercise health professional, that is, physiotherapist or allied health professional, who was involved in delivering an exercise intervention to a patient with thoracic cancer whose data were recorded during the survey period.
2.3 Study Procedure
A single survey link was generated for each thoracic cancer exercise service and sent to a single exercise health professional who had been identified by the healthcare service as being responsible for the provision of thoracic cancer exercise services. This exercise health professional was responsible for entering data for all people with thoracic cancer accessing exercise services at their healthcare service.
Study information and a survey link were sent to participants on the first and last day of the point-prevalence period. Up to four survey reminder e-mails were sent in the 6 weeks following the point-prevalence period.
2.4 Ethical Considerations
The study was approved by the University of Melbourne Human Research Ethics Committee (ID: 2023-24403-35797-4). Informed consent was obtained from all participants in the opening page of the survey. Participants could withdraw consent at any time. Identifiable data were collected and used for response accountability. Data were de-identified prior to analysis.
2.5 Analyses
Non-identifiable data were analyzed descriptively and inferentially using Statistical Package for Social Sciences (SPSS) Version 29.0 software [20]. Continuous variables were summarized as mean (SD) or median (interquartile range) depending on the normality of distributions. Categorical variables were summarized as counts (percentages). Post hoc comparisons between responding and non-responding sites regarding service funding and remoteness area were performed using Chi-square or Fisher's exact test with p < 0.05 deemed a significant result. Incomplete responses were included in the data analysis. No imputation for missing data was performed.
3 Results
3.1 Exercise Health Services
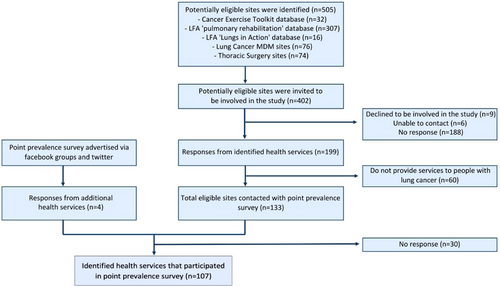
A total of 402 healthcare services were contacted, and 199 responded (50%). Overall, 69% (n = 137) of responding healthcare services accepted thoracic cancer referrals, and 78% (n = 107) of thoracic cancer exercise services completed the survey (see Figure 1). No significant differences were observed between responding and non-responding services when comparing remoteness area (p = 0.064) or center funding type (p = 0.056) using the chi-square test.
Exercise health services that participated in the point-prevalence survey all delivered exercise interventions in the outpatient clinic or community center setting. Virtual modes were employed by less than half of the services (videoconferencing 40%, n = 42; telephone 37%, n = 40), whereas home visits were offered by approximately one-quarter (26%, n = 28) (Table 1).
| Characteristics | n (%) |
|---|---|
| Location | |
| New South Wales | 32 (30) |
| Victoria | 31 (29) |
| Queensland | 16 (15) |
| South Australia | 12 (11) |
| Western Australia | 5 (5) |
| Tasmania | 5 (5) |
| Northern Territory | 4 (4) |
| Australian Capital Territory | 2 (2) |
| Service remoteness | |
| Major city | 62 (58) |
| Inner regional | 27 (25) |
| Outer regional | 13 (12) |
| Remote | 4 (4) |
| Very remote | 1 (1) |
| Service type | |
| Public hospital | 59 (55) |
| Private hospital | 8 (8) |
| Private clinic | 10 (9) |
| Community based rehab | 26 (24) |
| Other | 4 (4) |
| Intervention settings offered | |
| Outpatient clinic, community center, or gym | 107 (100) |
| Home visits | 28 (26) |
| Telehealth—video | 43 (40) |
| Telehealth—phone | 40 (37) |
| Timepoint on cancer care continuum service offered | |
| Prior to receiving treatment for cancer | 87 (81) |
| During treatment | 85 (79) |
| First 6 months after treatment | 88 (81) |
| Greater than 6 months after treatment | 77 (70) |
| Other | 14 (13) |
Most exercise health services were targeted to patients with general respiratory diseases and included people with lung cancer (58%, n = 60) compared with 31% cancer-specific (n = 33) and 5% lung cancer-specific (n = 5) programs. The majority of responding sites (n = 82, 77%) accepted referrals at all stages of the cancer care continuum.
3.2 Exercise Health Professionals
A total of 109 exercise health professionals delivered exercise therapy for people with thoracic cancer during the point-prevalence survey across 41 sites. Exercise professionals had a median (interquartile range [IQR]) of 6 (3–13) years’ experience and were predominantly physiotherapists (57%, n = 62). The majority worked in the public health setting (71%, n = 77) and practiced in a metropolitan area (75%, n = 82). Figure S1 provides further details.
3.3 People With Thoracic Cancer Attending an Exercise Program
Data were collected for 74 patients with thoracic cancer attending programs at the 41 sites (Table 2). Mean (SD) age was 69 (9.7) years [1]. Over half (n = 40) had non-small cell lung cancer, and one-quarter (n = 20) of patients had been diagnosed in the 6 months prior to data collection. Overall, 96% (n = 70) lived in major cities or inner regional areas, 70% (n = 52) lived with family or a caregiver, and 68% (n = 49) lived in a socioeconomically advantaged area. Few patients (4%, n = 3) were culturally and linguistically diverse, and no participants identified as Aboriginal or Torres Strait Islander. All patients identifying as CALD lived in metropolitan areas with low socioeconomic disadvantage. Level of education was reported for 45% (n = 33) of patients, with all finishing either secondary (30%, n = 22) or tertiary (15%, n = 11) education.
| Characteristics | n (%) |
|---|---|
| Gender | |
| Male | 44 (59) |
| Female | 30 (41) |
| Age | |
| 30–39 | 1 (1) |
| 40–49 | 1 (1) |
| 50–59 | 14 (19) |
| 60–69 | 20 (27) |
| 70–79 | 30 (41) |
| 80–89 | 8 (11) |
| Location of residence | |
| Queensland | 22 (30) |
| New South Wales | 20 (27) |
| Victoria | 14 (19) |
| Western Australia | 10 (14) |
| Tasmania | 5 (7) |
| South Australia | 2 (3) |
| Northern Territory | 1 (1) |
| Remoteness area | |
| Major cities | 41 (56) |
| Inner regional | 29 (40) |
| Outer regional | 1 (1) |
| Remote | 2 (3) |
| Missing | 1 (1) |
| Sociodemographic disadvantage | |
| Quintile 1 (most disadvantaged) | 17 (24) |
| Quintile 2 | 6 (8) |
| Quintile 3 | 15 (21) |
| Quintile 4 | 15 (21) |
| Quintile 5 (Least disadvantaged) | 19 (26) |
| Missing | 2 (3) |
| Time since diagnosis of lung cancer | |
| <1 month | 1 (1) |
| 1–5 months | 19 (26) |
| 6–11 months | 13 (18) |
| 12–23 months | 11 (15) |
| 2–5 years | 12 (16) |
| >5 years | 12 (16) |
| Unknown | 5 (7) |
| Missing | 1 (1) |
| Type of lung cancer | |
| NSCLC (n = 40) | |
| Stage 1 | 6 (15) |
| Stage 2 | 3 (8) |
| Stage 3 | 6 (15) |
| Stage 4 | 11 (28) |
| Unknown | 14 (35) |
| SCLC (n = 10) | |
| Limited | 3 (30) |
| Extensive | 6 (60) |
| Unknown | 1 (10) |
| Mesothelioma (n = 5) | |
| Stage 1 | 3 (60) |
| Unknown | 2 (40) |
| Unknown (n = 17) | |
| Missing (n = 2) | |
| Timepoint on the cancer care continuum | |
| Pretreatment | 6 (8) |
| Receiving treatment | 31 (42) |
| (Curative or palliative) | |
| Maintenance/Remission | 21 (28) |
| No further treatment | 16 (22) |
| Level of education | |
| High school (Inc. TAFE) | 22 (30) |
| Tertiary education | 11 (15) |
| Unknown | 40 (55) |
| Missing | 1 (1) |
| Aboriginal or Torres Strait Islander | |
| Does not identify | 71 (96) |
| Unknown | 1 (1) |
| Missing | 2 (3) |
| Culturally and linguistically diverse | |
| Culturally and linguistically diverse | 3 (4) |
| Not culturally and linguistically | 68 (93) |
| Diverse | |
| Missing | 2 (3) |
| Smoking history | |
| Ex-smoker | 42 (57) |
| Never smoker | 25 (34) |
| Current smoker | 5 (7) |
| Missing | 2 (3) |
| Living situation | |
| Lives with family or caregiver | 52 (70) |
| Lives alone | 18 (24) |
| Lives in residential care | 1 (1) |
| No fixed abode | 1 (1) |
| Missing | 2 (3) |
| Employment | |
| Retired | 49 (66) |
| Part-time employment | 7 (9) |
| Unemployment | 7 (9) |
| Unknown | 9 (12) |
| Missing | 2 (3) |
Most patients (97%, n = 72) were referred to an exercise program by a health professional (Table 3). Overall, 17% (n = 12) were attending exercise programs with an out-of-pocket expense with an average cost per session of $21 AUD. Over half of the exercise programs had a duration of 2 months (58%, n = 42) and exactly half of the patients (n = 36) attended their program twice during the week. Two-thirds of patients (65%, n = 46) had access to a referral for an ongoing exercise service following the completion of their current exercise program. The majority of patients attended a face-to-face appointment in an outpatient clinic or community center setting (93%, n = 65) (Table 3).
| Exercise program characteristics | n (%) |
|---|---|
| Duration of exercise program | |
| Single contact | 3 (4) |
| 1–2 weeks | 1 (1) |
| 3–7 weeks | 10 (14) |
| 2 months | 42 (58) |
| 3–6 months | 8 (11) |
| 7–12 months | 1 (1) |
| Ongoing | 7 (10) |
| Program referral | |
| Self-referred | 2 (3) |
| General practitioner | 16 (22) |
| Allied health | 16 (22) |
| Specialist doctor (cancer) | 12 (16) |
| Specialist nurse (cancer) | 10 (14) |
| Specialist doctor (non-cancer) | 17 (23) |
| Specialist nurse (non-cancer) | 1 (1) |
| Intervention delivery | |
| Individual | |
| Group | |
| Combination of both | |
| Intervention setting | |
| Outpatient clinic, community center, or gym | 66 (92) |
| Outpatient clinic and telehealth—phone call | 1 (1) |
| Outpatient clinic and telehealth—video call | 1 (1) |
| Telehealth—phone call | 4 (6) |
| Cost of program | |
| Costa | 12 (17) |
| No cost | 56 (78) |
| Unknown | 4 (6) |
| Intervention characteristics | n (%) |
|---|---|
| Visit type | |
| Initial assessment | 11 (15) |
| Initial and ongoing review | 1 (1) |
| Ongoing review | 56 (78) |
| Final review | 4 (6) |
| Visits per week/per participant | |
| 1 visit | 34 (47) |
| 2 visits | 36 (50) |
| 3 visits | 2 (3) |
| Aerobic exercise (n = 59) | |
| Intensity | |
| Light | 8 (14) |
| Moderate | 46 (78) |
| Not measured | 5 (8) |
| Type | |
| Continuous | 32 (54) |
| Intermittent | 23 (39) |
| Mixed | 2 (3) |
| Not known | 2 (3) |
| Resistance training (n = 57) | |
| Intensity | |
| Light | 10 (18) |
| Moderate | 43 (75) |
| Not measured | 4 (7) |
| Type | |
| Functional strength | 16 (28) |
| Free weights or bands | 10 (18) |
| Mixed | 29 (51) |
| Not known | 2 (4) |
| Home exercise program (n = 36) | |
| Aerobic only | 2 (6) |
| Strength only | 3 (8) |
| Both | 31 (86) |
- a Program costs per session: $5 (1 program), $8 (1 program), $10 (2 programs), $12 (2 programs), $35 (5 programs). One program cost $120 per month.
3.4 Interventions and Outcomes of the Exercise Programs
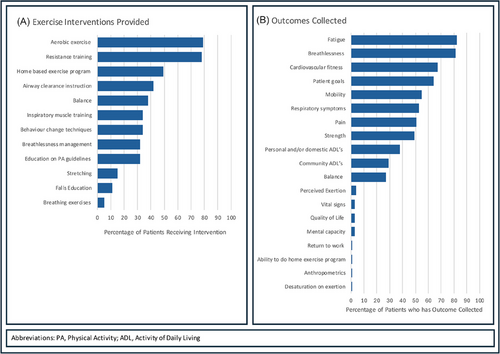
During the point-prevalence survey, 12 different exercise interventions were delivered in 45 combinations for 67 patients. Most patients completed aerobic (n = 58, 87%) and resistance training (n = 57, 85%) at a moderate intensity (Table 3). Approximately half received a home-based exercise program and airway clearance instruction. A total of 51 different combinations of 18 different outcomes were recorded for 70 patients. The most commonly collected outcomes were fatigue (86%, n = 60), breathlessness (84%, n = 59), and cardiovascular fitness (70%, n = 49) (Figure 2).
4 Discussion
This point-prevalence survey is the first study to report on the prevalence of exercise programs available to people with thoracic cancer and to report on the sociodemographic characteristics of people with thoracic cancer attending Australian exercise programs across all treatment types and stages of disease.
The number of exercise services that reported offering a service for people with thoracic cancer was low. With 137 exercise services for people with thoracic cancer identified, our findings indicate that there is 1 exercise service per 108 predicted new lung cancer diagnoses in 2023 [1] and 1 exercise service per 274 people living with lung cancer in Australia, based on 2018 prevalence data [21]. Considering these services are not solely for people with lung cancer but also for those with chronic diseases such as chronic obstructive pulmonary disease (COPD) (n = 60, 56%) or other cancers (n = 33, 31%), our results indicate that current service availability is not able to meet the needs of people with lung cancer in Australia.
The number of people accessing services during the study period was also low, with attendance of 74 people. These data indicate that this study included 0.2% of people in Australia with thoracic cancer who were attending an exercise program during the survey time period. Similarly low exercise program attendance levels are reported for people with comparable chronic diseases that involve lung tissue damage and result in respiratory symptoms such as those with COPD [22]. Multimorbidity is common for people with lung cancer, and a prior diagnosis of COPD, emphysema, chronic bronchitis, asthma, pneumonia, or tuberculosis approximately doubles a person's risk of being diagnosed with lung cancer [23]. Almost 50% of people with lung cancer have a concurrent diagnosis of COPD [24]. It has been reported that only 3% of people with COPD who are hospitalized access a pulmonary rehabilitation program within 1 year of hospital discharge [22]. This is despite pulmonary rehabilitation being recommended in COPD clinical practice guidelines with the highest level of evidence (Level 1) [22]. Lower attendance in pulmonary rehabilitation for people with COPD is reported for people with a higher comorbidity index and with increased numbers of hospitalizations [22]. This may partially account for lower attendance in exercise programs in the lung cancer population when compared to COPD, as lung cancer is associated with higher comorbid burden [25] and hospitalization rates [26].
Over 80% of exercise services and health professionalswere located in metropolitan or inner regional areas; by comparison, 96% of people accessing an exercise service during the point prevalence period were from metropolitan or inner regional areas. This indicates that although the proportion of services available to people with thoracic cancer in remote areas is comparable to the distribution of the Australian population, uptake of exercise programs in these areas is disproportionately low. Although telerehabilitation is a safe and feasible method of delivering exercise programs to people with lung cancer living a greater distance from an exercise program, our research indicates that use of this technology is low. Despite nearly half of services offering exercise interventions via telehealth (videoconferencing or telephone), only six patients (6%) engaged with exercise therapy via virtual mode. Low recruitment and attendance rates with telerehabilitation are observed in randomized controlled trials conducted with people with lung cancer [27], suggesting further research is needed to enable the uptake and implementation of telerehabilitation to overcome barriers to accessing care for people living in remote and outer regional areas.
Sociodemographic factors and geographical distance from an exercise service are reported to impact a person's attendance and engagement with exercise programs in COPD and breast cancer populations [12, 22]. Although Australian age-standardized lung cancer incidence is 76% higher in lower socioeconomic status areas, our study shows the reverse relationship where one-quarter (24%, n = 17) of patients who attended an exercise service lived in the most socioeconomically disadvantaged area [1]. A similar relationship is seen with remoteness area, where the age-standardized incidence rate is 21% higher in remote and very remote areas than metropolitan areas, and yet 3% (n = 2) of patients who attended an exercise service in this study lived in remote areas, and no participants lived in very remote areas [1]. Although low participation from people living in outer regional or remote areas may be attributed to geographical distance from services [28], the relationship between remoteness area and sociodemographic factors should not be ignored, as the most advantaged areas in Australia are commonly located around metropolitan areas and inner regional areas [16]. Cigarette smoking is another factor that may impact exercise participation, linked to geographical area and socioeconomic status [29]. Smoking is associated with delayed medical help-seeking behavior [30] and lower adherence with exercise programs in an oncology population following completion of treatment [31]. Although Australian data show that over one-third of Australians with lung cancer are current smokers [32], our results show that 7% (n = 5) of people attending exercise services were current smokers.
Social determinants of health, such as level of education and social supports, are linked to low service utilization, lower access to treatment, and poorer overall outcomes [33]. In this study, all patients with a known level of education had completed either a secondary or tertiary level qualification. Higher education levels may lead to increased awareness of educational needs and benefits of supportive care interventions [34]. This may also be linked to geographical area, as people living in metropolitan areas are more than twice as likely to have a tertiary education compared with people living in regional and remote areas in Australia [35].
Culturally adapted exercise programs are likely to improve engagement and uptake for Indigenous Australians and people from CALD backgrounds; however, access to these resources remains low [36, 37]. There were no patients recorded as identifying as Aboriginal and/or Torres Strait Islander attending an exercise program, and only three identified as CALD during the point-prevalence period. Common barriers to exercise include transport difficulties, lack of access to optimal care pathways, and lack of culturally appropriate care and education [38, 39]. An additional barrier for people from CALD backgrounds may be the lack of awareness of services and lack of interpreting services available when attending exercise services [40, 41]. Research conducted with Aboriginal health workers and exercise physiologists found that using co-design principles to develop culturally adapted COPD resources promoted participation and collaboration [42]. Highlighting the need for implementation research conducted with CALD and Indigenous Australian lung cancer populations to improve understanding and uptake of culturally safe exercise programs.
The high heterogeneity in exercise interventions and outcome measures observed in our study is analogous to the heterogeneity observed in clinical trials of exercise and lung cancer [4]. High heterogeneity in the prescription of exercise interventions in research limits the capacity of clinicians to translate findings into their clinical practice and may lead to ineffective exercise interventions being delivered to patients. When compared with cross-sectional data in a surgical lung cancer population, variability in exercise intervention type is comparable; however, the number of outcomes reported is increasingly variable when not limited to a surgical cohort [5]. Variability in medical treatment side effects and disease burden experienced by people with unresectable lung cancer may impact these differences. Limited standardization of outcome collection in clinical practice may lead to the collection of less relevant and patient-centered outcomes and limit the ability of health services to evaluate clinical programs [43]. Furthermore, the lack of consensus restricts the development of clear recommendations for exercise prescription and outcome measure collection in lung cancer, hindering clinicians’ ability to design and implement a consistent model of care.
4.1 Limitations
There are several limitations to this study. Point-prevalence data represent clinical practice over a 5-day period and may not be representative of usual practice throughout the year. The initial nonresponse rate was 50%, indicating that data collected may not be representative of all exercise services across Australia. However, following recruitment to the point-prevalence survey, the response rate was 78%, and no significant difference was observed between responder and nonresponder services in terms of funding or remoteness area. We were unable to compare the location of responding sites with the density of culturally and linguistically diverse populations across Australia as data were not available.
5 Conclusion and Future Research
Despite a high level of evidence for the benefits of exercise for people with lung cancer, the results of our point-prevalence survey indicate that both the availability of exercise services for and attendance levels at exercise programs by people with lung cancer in Australia are low.
Future research should aim to understand and overcome service and patient barriers to providing and accessing exercise services for a thoracic cancer population. This research should be leveraged to design and implement exercise interventions to support CALD populations and Indigenous Australians, as well as people with lower levels of education and those who live alone. Future research should explore methods for leveraging telehealth exercise programs for people who are unable to access center-based pre- or rehabilitation.
To standardize clinical practice, a core-outcome set with rehabilitation outcomes should be developed and implemented. Furthermore, additional interventional studies should be conducted to compare the impact of different exercise interventions on outcomes for people with lung cancer.
Acknowledgments
We would like to thank Sangeeta Sathyanath and Claire O-Donnell for piloting the survey, in addition to the University of Melbourne Statistical Consulting Centre.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.