Temporal associations of diabetes-related complications with health-related quality of life decrements in Chinese patients with type 2 diabetes: A prospective study among 19 322 adults—Joint Asia Diabetes Evaluation (JADE) register (2007–2018)
Abstract
Background
Patients with type 2 diabetes (T2D) are at high risk of developing multiple complications, affecting their health-related quality of life (HRQoL). Existing studies only considered impact of complication on HRQoL in the year of occurrence but not its residual impacts in subsequent years. We investigated temporal impacts of diabetes-related complications on HRQoL in a 12-year prospective cohort of ambulatory Chinese patients with T2D enrolled in the clinic-based Joint Asia Diabetes Evaluation (JADE) Register.
Methods
HRQoL utility measures were derived from EuroQol five-dimensional three-level questionnaire (EQ-5D-3L) questionnaires completed by 19 322 patients with T2D in Hong Kong (2007–2018). Temporal EQ-5D utility decrements associated with subtypes of cardiovascular-renal events were estimated using generalized linear regression model after stepwise selection of covariates with p < .01 as cutoff.
Results
In this cohort (mean ± SD age:61.2 ± 11.5 years, 55.3% men, median [interquartile range] duration of diabetes:10.1 [3.0–15.0] years, glycated hemoglobin [HbA1C] 7.5 ± 1.5%), EQ-5D utility was 0.860 ± 0.163. The largest HRQoL decrements were observed in year of occurrence of hemorrhagic stroke (−0.230), followed by ischemic stroke (−0.165), peripheral vascular disease (−0.117), lower extremity amputation (−0.093), chronic kidney disease (CKD) G5 without renal replacement therapy (RRT) (−0.079), congestive heart failure (CHF) (−0.061), and CKD G3–G4 without RRT (−0.042). Residual impacts on HRQoL persisted for 2 years after occurrence of CHF or ischemic stroke and 1 year after hemorrhagic stroke or CKD G3–G4 without RRT.
Conclusion
This is the first comprehensive report on temporal associations of HRQoL decrements with subtypes of diabetes-related complications in ambulatory Asian patients with T2D. These data will improve the accuracy of cost-effectiveness analysis of diabetes interventions at an individual level in an Asian setting.
1 BACKGROUND
The global population with diabetes is predicted to increase from 537 million in 2021 to 783 million in 2045, with a quarter of them living in China.1 Patients with diabetes are at high risk of developing multiple co-morbidities such as cardiovascular, renal, neurological, visual and cancer events. These events pose significant burden on healthcare systems and negatively impact patients' health-related quality-of-life (HRQoL).2 Measurement of the latter is critical for estimating quality-adjusted life-years in health economic analysis. Most of the studies on HRQoL decrements related to diabetes complications were conducted in European populations.3-6 Diabetes-related complications impaired HRQoL in the year of index event and subsequent years.7 However, there are few prospective cohorts, such as the United Kingdom Prospective Diabetes Study, which quantified long-term health impacts of diabetes.8, 9 Given the growing epidemic of diabetes in Asia with its cultural, economic, and healthcare systems different from the West, there is a need to investigate the long-term temporal associations between diabetes-related complications and HRQoL in Asian populations. Such data will provide valuable insights into the dynamic interplay between complications and HRQoL over time.
In this study, we seek to close this knowledge gap by examining temporal associations of diabetes-related complications with HRQoL in a 12-year prospective cohort of Chinese patients with type 2 diabetes (T2D) enrolled in the Joint Asia Diabetes Evaluation (JADE) Register in 2007–2018. These data will allow more accurate cost-effectiveness analysis of interventions to inform long-term policy for improving the health and HRQoL in patients with T2D.
2 METHODS
2.1 Patient sample
The Hong Kong Hospital Authority (HA) governs all public hospitals and clinics that provide 95% hospital bed-days and 80% outpatient visits territory-wide. All HA facilities shared a territory-wide electronic medical record (EMR) system consisting of admission records, laboratory results, and prescriptions. The JADE Technology is a web-based diabetes risk assessment platform established in 2007 as an extension of the Hong Kong Diabetes Register established in 1995. The latter is a quality improvement program at Prince of Wales Hospital, the teaching hospital of the Chinese University of Hong Kong (CUHK). The JADE platform includes care protocol, data entry system, and risk engines to issue personalized report with decision support. Data were recorded during nurse-led structured assessment including medical history, eye and feet evaluation, self-care practices, and laboratory investigations (blood and urine).10 In 2007, the EuroQol five-dimensional three-level questionnaire (EQ-5D-3L) HRQoL questionnaire (Traditional Chinese version) was included as an assessment item when the JADE Technology was established.
2.2 Inclusion and exclusion criteria
The JADE Register enrolled patients with diabetes attending two public-hospital diabetes centers and a CUHK-affiliated nonprofit diabetes center between 2007 and 2018. All patients underwent structured assessment using case report forms with predefined items followed by data entry into the JADE Platform (n = 22 787). Patients were referred by public and private doctors or through self-referral.11 In this analysis, we excluded patients aged <18 years, non-Chinese, and those who underwent assessment before 2007 (when EQ-5D-3L assessment was included) and after 2019 (when all events were censored) from the analysis. Patients with type 1 diabetes defined as continuous use of insulin within 1 year of diagnosis or presentation with acute ketosis or diabetic ketoacidosis were excluded. All patients had a unique identifier that was used to retrieve clinical outcomes based on hospitalization records in the HA EMR. All patients gave written informed consent for analysis of anonymized data and publication. The study was approved by the CUHK Clinical Research Ethics Committee (CREC number: 2007.339).
2.3 HRQoL assessment
EQ-5D-3L comprises five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression rated by three responses: 1-no problem, 2-some problems, and 3-severe problems. We included data from completed EQ-5D-3L surveys. EQ-5D-3L utility scores were reverse cross-walked into EQ-5D-5L scores,12 then mapped to Hong Kong EQ-5D-5L valuation set.13 HRQoL utility score of 1 corresponds to full health, 0 represents a health-state equivalent to death and negative values imply health-states worse than death.
2.4 Temporality of diabetes complications
Diabetes complications of interest included coronary heart disease (CHD), congestive heart failure (CHF), ischemic stroke, hemorrhagic stroke, peripheral vascular disease (PVD), lower extremity amputation (LEA), end-stage kidney disease (ESKD), and any type of cancer. Events were defined by International Classification of Disease, Ninth Revision codes of all admissions and procedures14 (Supplementary Table S1).
To estimate temporal impacts of events on HRQoL, ordered time categories were generated with reference to time period between date of complication event closest to the date of structured assessment and EQ-5D-3L survey. Time categories were assigned as “no event,” event experienced “within 1 year,” “within 2 to 3 years,” “within 3 to 4 years,” “within 4 to 5 years,” and “more 5 five years” prior to the measurement of HRQoL. For each complication, time categories with ≤5 events were combined with previous time category level. Consecutive time categories (adjusted for patients' personal and clinical characteristics) without significant differences were combined (F-test at 1% significance level).
2.5 Definitions and covariates
T2D was defined as lack of history of ketoacidosis or nonrequirement of continuous insulin treatment within 1 year of diagnosis. Variables including demographics, lifestyle, types of care (public/ private), clinical and biochemical characteristics, complications, medical treatments, and histories were adjusted in our model. All data were collected in structured case report forms with codes and definitions as listed in Supplementary Table S2.
2.6 Statistical analysis
2.6.1 Specification of regression models
Data are expressed as mean (SD) or median (interquartile range). HRQoL regression was modeled using generalized linear model with Gaussian family distribution and linear link function, adjusting for patients' demographic and clinical characteristics, temporal diabetes complication events and Elixhauser Comorbidity Index (ECI).15
Stepwise selection of covariates was carried out to evaluate associations of HRQoL with temporality of diabetes complications and other risk factors. Covariates including age, sex, duration of diabetes, year of assessment, smoking habit, and drug use were kept stable during covariate selection. Covariates with significance at 1% level were included in the final model. Missing data were imputed for 10 iterations. All analyses were conducted using R 3.4.2. A P-value<0.01 was considered significant.
3 RESULTS
Of 22 787 Chinese patients with T2D enrolled in the JADE Register between 2007 and 2018, 19 322 (84.8%) completed all items in the EQ-5D-3L questionnaire. Table 1 summarizes the clinical profile of these patients, of whom 55.3% were men. The mean age of the cohort was 61.2 years (SD: 11.5); mean age of diagnosis, 51.1 years (SD:11.8), and mean diabetes duration, 10.1 years (interquartile range: 3.0–15.0). More than half attended middle school or above (58.8%) and had regular physical activity (57.4%). Nearly one third were occasional or regular alcohol drinkers (28.5%) and 1 in 10 patients were current smokers (11.4%). Over half were overweight or obese (body mass index [BMI]≥25 kg/m2; 55.3%), had a diastolic blood pressure (BP) ≥75 mm Hg (55.5%), fasting plasma glucose (FPG) ≥7 mmol/L (54.4%), or HbA1C ≥ 7.0% (57.7%. One in five patients had reduced kidney function with estimated glomerular filtration rate (eGFR) ≤60 mL/min/1.73m2 (20.8%). The majority of patients were on glucose-lowering drugs (GLDs, 85.7%), 26.2% on insulin, 52.9% on statins, 35.8% on angiotensin-converting enzyme (ACE) inhibitors, 15.3% on angiotensin receptor blocker (ARB), and 19.9% on BP lowering drugs (excluding ACE inhibitors/ARB). Most patients (87.6%) visited public hospital clinics for baseline assessment. One in four patients (21.3%) self-reported having experienced hypoglycemia in the last 3 months.
| Variable | Mean or n (SD or %) |
|---|---|
| Personal characteristics | |
| Men (n [%]) | 10 678 (55.3) |
| Age at assessment (years) (n [%]) | 61.2 (11.5) |
| <40 years old | 796 (4.1) |
| 40–59 years old | 7870 (40.7) |
| ≥60 years old | 10 656 (55.1) |
| Age at diabetes diagnosis (years) (n [%]) | 51.1 (11.8) |
| <40 years old | 3055 (15.8) |
| 40–59 years old | 11 770 (60.9) |
| ≥60 years old | 4383 (22.7) |
| Missing | 114 (0.6) |
| Duration of diabetes (years) (n [%]) | 10.1 (8.4) |
| <5 years | 6180 (32.0) |
| 5–9 years | 4388 (22.7) |
| 10–14 years | 3574 (18.5) |
| ≥15 years | 5064 (26.2) |
| Missing | 116 (0.6) |
| Type of care model | |
| Public | 16 918 (87.6) |
| Private | 2053 (10.6) |
| Missing | 351 (1.8) |
| Year of structured assessment with EQ-5D-3 L data (year) [mean (SD)] | 2012.76 (2.32) |
| Education (n [%]) | |
| Primary, illiterate or others | 7897 (40.9) |
| Middle or high school | 9052 (46.8) |
| College or above | 2319 (12.0) |
| Missing | 54 (0.3) |
| Lifestyle factors | |
| Alcohol use (n [%]) | |
| Never | 11 446 (59.2) |
| Occasional | 4889 (25.3) |
| Regular | 616 (3.2) |
| Ex-drinker | 2335 (12.1) |
| Missing | 36 (0.2) |
| Smoking (n [%]) | |
| Never | 13 124 (67.9) |
| Current smoker | 2196 (11.4) |
| Ex-smoker | 3985 (20.6) |
| Missing | 17 (0.1) |
| Physical activity (per week) (n [%]) | |
| No regular activity | 7442 (38.5) |
| <3 times | 2654 (13.7) |
| 3–4 times | 1475 (7.6) |
| 5 times | 812 (4.2) |
| >5 times | 6173 (31.9) |
| Missing | 766 (4.0) |
| Frequency of hypoglycemia (n [%]) | |
| At least daily | 30 (0.2) |
| At least once monthly | 1288 (6.7) |
| At least once weekly | 460 (2.4) |
| Less than once monthly | 2322 (12.0) |
| None | 15 156 (78.4) |
| Missing | 66 (0.3) |
| Clinical characteristics | |
| Body mass index (kg/m2) (n [%]) | 26.1 (4.4) |
| <25 | 8561 (44.3) |
| 25–30 | 7593 (39.3) |
| ≥30 or more | 3095 (16.0) |
| Missing | 73 (0.4) |
| Diastolic blood pressure (mm Hg) (n [%]) | 76.5 (11.0) |
| <75 | 8574 (44.4) |
| ≥75 < 85 | 6557 (33.9) |
| ≥85 | 4182 (21.6) |
| Missing | 9 (0.0) |
| Visual acuity (n [%]) | |
| No significant visual impairment | 18 495 (95.1) |
| Severe visual impairment (counting fingers, hand movement, light perception) | 821 (4.2) |
| Blind (no light perception) | 125 (0.6) |
| Complications and comorbidities | |
| Sensory neuropathy (n [%]) | |
| True | 1211 (6.3) |
| Diabetic retinopathy | |
| None | 14 249 (73.3) |
| Nonproliferative/ preproliferative retinopathy | 4668 (24.0) |
| Proliferative retinopathy, maculopathy, or advanced eye disease | 524 (2.7) |
| History of retinal, cataract surgery, or laser treatment | |
| True | 3513 (18.1) |
| Renal disease | |
| CKD G3–G4 (No dialysis or transplant) (n [%]) | |
| < 1 year | 1255 (6.5) |
| ≥1 year | 1665 (8.6) |
| CKD G5 (No dialysis or transplant) (n [%]) | |
| Any year | 29 (0.2) |
| Cardiovascular disease | |
| Congestive heart failure (n [%]) | |
| <1 year | 164 (0.8) |
| ≥1 < 2 years | 104 (0.5) |
| ≥2 < 3 years | 71 (0.4) |
| ≥3 years | 139 (0.7) |
| Ischemic stroke (n [%]) | |
| <1 year | 135 (0.7) |
| ≥1 < 2 years | 83 (0.4) |
| ≥2 years | 475 (2.5) |
| Hemorrhagic stroke (n [%]) | |
| <1 year | 25 (0.1) |
| ≥1 year | 106 (0.5) |
| Peripheral vascular disease (n [%]) | |
| <1 year | 44 (0.2) |
| ≥1 year | 108 (0.6) |
| Lower extremity amputation (n [%]) | |
| Any year | 94 (0.5) |
| Elixhauser comorbidity score (van Walraven 2009) (n [%]) | |
| < 0 | 550 (2.8) |
| 0 | 13 202 (67.9) |
| >0 < 5 | 1482 (7.6) |
| ≥5 < 15 | 3376 (17.4) |
| ≥15 < 25 | 768 (4.0) |
| ≥25 | 63 (0.3) |
| Biochemistry | |
| Fasting plasma glucose (mmol/L)) (n [%]) | 7.7 (2.6) |
| <5.7 | 3253 (16.8) |
| ≥5.7 < 7.0 | 5480 (28.4) |
| ≥7.0 | 10 502 (54.4) |
| Missing | 87 (0.5) |
| Hemoglobin A1C (%) (n [%]) | 7.5 (1.5) |
| <5.7 | 617 (3.2) |
| ≥5.7 < 7.0 | 7516 (38.9) |
| ≥7.0 | 11 153 (57.7) |
| Missing | 36 (0.2) |
| HDL-cholesterol (mmol/L) (n [%]) | 1.3 (0.4) |
| <1.3 | 9483 (49.1) |
| ≥1.3 < 1.55 | 5502 (28.5) |
| ≥1.55 | 4228 (21.9) |
| Missing | 109 (0.6) |
| LDL-cholesterol (mmol/L) (n [%]) | 2.4 (0.8) |
| <2.6 | 11 483 (59.4) |
| ≥2.6 < 3.35 | 5100 (26.4) |
| ≥3.35 | 2334 (12.1) |
| Missing | 405 (2.1) |
| Estimated glomerular filtration rate (mL/min/1.73m2) (n [%]) | 78.9 (24.6) |
| <30 | 956 (4.9) |
| ≥30 < 60 | 3064 (15.9) |
| ≥60 < 90 | 7633 (39.5) |
| ≥90 | 7648 (39.6) |
| Missing | 21 (0.1) |
| Alanine transaminase levels (IU/L) (n [%]) | 28.3 (22.5) |
| <10 | 473 (2.4) |
| ≥10 < 40 | 15 638 (80.9) |
| ≥40 | 3109 (16.1) |
| Missing | 102 (0.5) |
| Plasma albumin (g/L) (n [%]) | 43.5 (3.43) |
| <35 | 317 (1.6) |
| ≥35 < 50 | 18 586 (96.2) |
| ≥50 | 334 (1.7) |
| Missing | 85 (0.4) |
| Hemoglobin (g/dL) (n [%]) | 13.4 (1.6) |
| <10 | 519 (2.7) |
| ≥10 | 18 650 (96.5) |
| Missing | 153 (0.8) |
| Treatments (Ref: none) | |
| Glucose lowering drugs (n [%]) | |
| True | 16 563 (85.7) |
| Insulin (n [%]) | |
| True | 5054 (26.2) |
| Statins (n [%]) | |
| True | 10 233 (52.9) |
| Missing | 258 (1.3) |
| Angiotensin-converting enzyme (ACE) inhibitor (n [%]) | |
| True | 6911 (35.8) |
| Missing | 190 (1.0) |
| Angiotensin receptor blocker (ARB) (n [%]) | |
| True | 2961 (15.3) |
| Missing | 190 (1.0) |
| Blood pressure lowering drugs (excluding RAS inhibitors—ACE/ARB) (n [%]) | |
| True | 3853 (19.9) |
| Missing | 191 (1.0) |
- Abbreviations: CKD, chronic kidney disease; EQ-5D-3L, EuroQol five-dimensional three-level questionnaire; HDL, high-density lipoprotein; LDL, low-density lipoprotein; RAS, renin-angiotensin system; T2D, type 2 diabetes.
Among the EQ-5D domains, 29.9% of patients reported some or severe problems in pain/discomfort, 18.9% for anxiety/depression, 9.5% for mobility, 6.7% for usual activity, and 3.2% for self-care (Table 2). The mean EQ-5D utility score was 0.860 (SD: 0.163) and 11 450 (59.3%) reported full health. The mean EQ-5D utility of patients who did not experience any complications was 0.869 (SD: 0.149) and decreased to 0.792 (SD: 0.227) in those who experienced one complication and 0.724 (SD: 0.290) in those who experienced two or more complications.
| Mobility (n [%]) | Self-care (n [%]) | Usual activities (n [%]) | Pain/discomfort (n [%]) | Anxiety/depression (n [%]) | |
|---|---|---|---|---|---|
| 1 No problem | 17 485 (90.5) | 18 713 (96.8) | 18 038 (93.4) | 13 547 (70.1) | 15 658 (81.0) |
| 2 Some problems | 1786 (9.2) | 495 (2.6) | 1118 (5.8) | 5366 (27.8) | 3485 (18.0) |
| 3 Severe problems | 51 (0.3) | 114 (0.6) | 166 (0.9) | 409 (2.1) | 179 (0.9) |
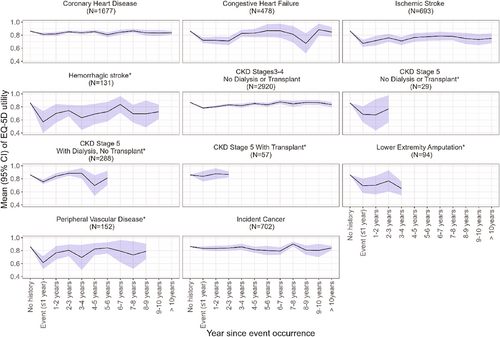
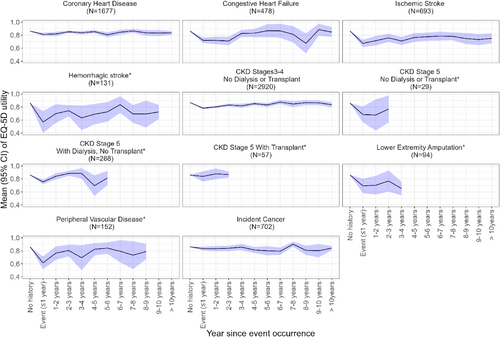
Unadjusted mean HRQoL utility trends by time of occurrence for each complication are summarized in Figure 1. Large decrements in HRQoL utility were observed in year of occurrence of hemorrhagic stroke, ischemic stroke, PVD, LEA, and chronic kidney disease (CKD) G5 without renal replacement therapy (RRT). Although EQ-5D utilities gradually improved over time, it rarely recovered to the utility levels before the occurrence of event.
3.1 EQ-5D decrements associated with diabetes-related complications
Figure 2 shows the temporal associations of EQ-5D utility decrements with diabetes-related complications. For cardiovascular events, the largest EQ-5D utility decrements were observed in year of occurrence of a hemorrhagic stroke (−0.230 [95% confidence interval (CI): −0.289 to −0.170]), followed by ischemic stroke (−0.165, [95% CI: −0.191 to −0.139]), PVD (−0.117 [95% CI: −0.165 to −0.070]), LEA in any year after occurrence (−0.093 [95% CI: −0.126 to −0.059]), and CHF (−0.061 [95% CI: −0.085 to −0.037]).
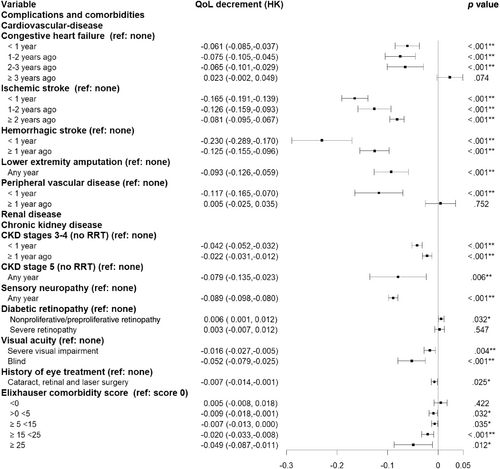
For kidney events, occurrence of CKD G5 without RRT in any year after event occurrence was associated with greater HRQoL decrement (−0.079, [95% CI: −0.135 to −0.023]) compared to occurrence of CKD G3–G4 without RRT (−0.042 [95% CI: −0.052 to −0.032]). We examined the changes in eGFR and urinary albumin creatinine ratio (ACR) values 3 years before and 3 years after their first event of hospitalization with chronic kidney disease as the primary diagnosis. Patients showed significant improvements in mean eGFR and ACR after transplantation as compared to progressive decline in eGFR and increase in ACR in patients at G3–G4 or G5 without receiving renal replacement therapy (Supplementary Figure S1).
Detection of sensory neuropathy during assessment was associated with worse HRQoL decrement than those with visual problems. For the latter, blindness was associated with the worst HRQoL decrement, followed by severe visual impairment and history of eye treatment. Because EQ-5D utility was not impaired in patients with diabetes who had CHD, cancer, and CKD G5 with RRT, these complications were not included in our final model.
In most patients, cardiovascular event had significant residual impacts on HRQoL that seldom returned to preevent health-state. Ischemic stroke or CHF had significant detrimental impacts on HRQoL that persisted for 2 years and remained static. HRQoL decrements were also observed 1 year after occurrence of CKD G3–G4 without RRT. Patients with increasing number of comorbidities (higher ECI scores) had worse HRQoL (Figure 2).
3.2 EQ-5D utility decrements associated with demographics, risk factors, and behaviors
Independent of occurrence of these complications, female sex, age of diabetes diagnosis ≥60 years, ≥15 years of diabetes, BMI ≥30 kg/m2, and being ex-alcohol drinkers were associated with lower HRQoL (Supplementary Table S3). Frequent self-reported hypoglycemia episodes were associated with greater HRQoL decrements whereas frequent physical activity levels were associated with better HRQoL. Patients with lower education level (primary, illiterate, or others: ≤6 years) had worse HRQoL than those with higher level (middle or high school: >6 and ≤13 years).
Users of GLDs and ACE inhibitors had better HRQoL than nonusers. Insulin use was not associated with significant HRQoL decrement (Supplementary Table S3). For risk factors, low-density lipoprotein (LDL)-cholesterol ≥2.6 mmol, HbA1C ≥5.7%, FPG ≥5.7 mmol/L, and eGFR 30–60 mL/min/1.73m2 were associated with higher HRQoL and high-density lipoprotein (HDL)-cholesterol <1.3 mmol/L and diastolic BP ≥75 mm Hg were associated with reduced HRQoL utilities. Patients with serum albumin<35 g/L, alanine transaminase<10 IU/L, and hemoglobin <10 g/dL were associated with reduced HRQoL.
4 DISCUSSION
This is the first report on the temporal associations of a comprehensive array of subtypes of diabetes-related cardiovascular-renal complications on HRQoL using the prospective data from the JADE Register. During a 12-year period, 19 322 Chinese patients with T2D from Hong Kong enrolled in the register and completed the EQ-5D survey. Cardiovascular-renal complications had detrimental and long-lasting impacts on HRQoL. The largest HRQoL decrement expressed as EQ-5D utility score was observed in year of occurrence of a hemorrhagic stroke (−0.230), followed by ischemic stroke (−0.165), PVD (−0.117), LEA (−0.093), sensory neuropathy (−0.089), CKD G5 without RRT (−0.079), CHF (−0.061), and CKD G3–G4 without RRT (−0.042). Residual impacts on HRQoL persisted after index event of CHF, ischemic stroke, hemorrhagic stroke, or CKD G3–G4 without RRT. However, CHD, cancer, and CKD G5 with RRT were not associated with impaired HRQoL.
In alignment with other studies, 20%–30% of JADE participants reported some problems with pain/discomfort and anxiety/depression.16 The mean EQ5D utility of 0.860 from our cohort was comparable to that reported in Asian patients with diabetes (0.84–0.91).16-20 In general, these scores were higher in Asian than their European counterparts (0.72–0.80) possibly due to differences in values, culture, and traditions.16, 21, 22 Although HRQoL decrements related to diabetes complications had been reported in Asians, its temporal relationship with time of occurrence of event has not been previously estimated.20, 23-25 Our study is the first to evaluate residual HRQoL decrements related to diabetes complications in subsequent years after occurrence of the event. These prospective data will allow more precise estimation of health benefits of new diabetes interventions and their long-term cost-effectiveness.
Previous studies in Asia that explored HRQoL decrements with diabetes complications had considerably less granularity than our report.18, 24, 26-28 For example, this is the first Asian study to report HRQoL decrements for ischemic and hemorrhagic stroke subtypes. In a meta-analysis, sodium-glucose-transporter 2 inhibitors reduced hemorrhagic stroke but not ischemic stroke or all-stroke.29 By contrast, glucagon-like-peptide receptor agonist reduced ischemic stroke but not hemorrhagic stroke.30 Given subtle differences in etiologies and risk factors for stroke subtypes as well as drug mechanisms, differences in drug effects are plausible. These HRQoL estimates enable us to identify patient subgroups who will benefit most from a drug using cost-effectiveness models simulated using individual patient data.
Although the overall HRQoL of Asian patients with T2D was higher than that of their European counterparts,31-33 Asian patients were more prone to develop stroke than CHD.34 In this study, ischemic (−0.165) and hemorrhagic stroke (−0.230) decrements were higher than that reported in studies with mainly Europeans (ASCEND [A Study of Cardiovascular Events iN Diabetes] trial ischemic stroke: −0.062,7 LEADER [Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results] trial stroke: −0.046,32 ADVANCE [Action in Diabetes and Vascular Disease-PreterAx and DiamicroN Controlled Evaluation] trial stroke: −0.099,5 and MEPS [Medical Expenditure Panel Survey] database stroke: −0.060).35 Our findings corroborate results from the Acarbose Cardiovascular Evaluation trial conducted in Chinese patients with impaired glucose tolerance (IGT) (overall stroke: −0.107)36 and a hospital-based study in Chinese patients with T2D (overall stroke: −0.101).18 In this trial, which enrolled patients with prior cardiovascular disease and IGT, HRQoL decrements associated with stroke were higher than those in European patients with T2D. To this end, high prevalence of stroke in Asians might be due to high salt intake and high prevalence of hypertension, further aggravated by increasing obesity and diabetes, related to rapid socioeconomical and lifestyle transition.37 These regional, ecological, and cultural differences call for more effective stroke prevention strategies to reduce the immediate and residual impacts of stroke on HRQoL in Asians with T2D.38, 39
In our study, patients who experienced CHF had persistent HRQoL decrements in subsequent years. This contrasts the improvements in QoL decrements in subsequent years reported in the ACCORD trial (<1 year: −0.089, >1 year ago: −0.041).4 HRQoL decrements related to PVD (−0.117) were comparable to Japanese (−0.070)28 and European (−0.061)40 patients with diabetes. In our cohort, LEA HRQoL decrements (−0.093) were smaller than in other populations (Japan: −0.178,28 United Kingdom: −0.272,40 ASCEND trial: −0.2067), which may be due to the majority of our patients having minor toe amputations only.
Our reported HRQoL decrements for ESKD (G5 without RRT) (−0.079) were similar to other reports (ADVANCE trial: −0.049,5 Japanese cohort: −0.05028). In our analysis, patients undergoing RRT exhibited significant improvements in albuminuria and eGFR, in contrast to those who did not receive RRT, who experienced a progressive decline in kidney function. Compared to patients at G3–G4 without RRT, patients at CKD G5 with RRT had no significant HRQoL decrements. Other researchers had reported considerable improvement in HRQoL in patients with ESKD after RRT, especially with transplantation, the latter being considered a cost-effective treatment in many countries.41, 42
Decrements in HRQoL associated with sensory neuropathy (−0.089) in this cohort were comparable to similar reports (Europe: −0.084,40 China: −0.057,25 Japan: −0.06628). For proliferative retinopathy and visual acuity, the HRQoL decrements were similar to those in Japanese (blindness in one eye: −0.032, blindness in both eyes: −0.108)28 and Chinese (sight-threatening retinopathy: −0.043)24, 25 cohorts. These data highlighted that, although these microvascular complications might not be immediately life threatening, their negative impacts on HRQoL should not be underestimated and call for better prevention efforts.43 In agreement with other studies, multimorbidity indicated by increased ECI scores was associated with worse HRQoL (score ≥25: −0.049). Although other local researcher had reported greater decrements with increasing number of diabetes comorbidities (three: −0.060, ≥four: −0.173), they had not adjusted for the impacts of diabetes-related complications.20
Concurring with other reports,7, 24, 26, 44 we did not observe significant HRQoL decrements with CHD, which might be attributed to advancements in cardiology-related technology. The lack of significant HRQoL decrements with incident cancers and CKD G5 with RRT might be due to referral or survival bias. Patients in the JADE Register were assessed in an ambulatory care setting, which might have limited the representation of patients with severe diseases. Because patients on RRT or those with cancer were followed up frequently at dialysis and cancer centers respectively, they were less likely to be referred to the diabetes center for assessment and education with possible referral bias.
The associations of female gender,7, 20, 23, 28 old age,5, 7, 23 low education level,27 obesity,7, 23 and alcohol use25 with low HRQoL were also observed in our cohort whereas patients with exercise ≥ three times weekly had higher HRQoL. In the Look AHEAD (Action for Health in Diabetes) trial, 175 min exercise weekly with ≥7% weight loss improved not only HRQoL but also control of blood glucose, BP, and blood lipids accompanied by reduced incidence of CKD, retinopathy, and depression.45 Physical exercise is known to increase secretion of neurotransmitters such as endocannabinoids46 and brain-derived neurotrophic factor,47 which might reduce depression and anxiety.
In our analysis, LDL-cholesterol ≥2.6 mmol, HbA1C ≥5.7%, or eGFR 30–60 mL/min/1.73 m2 were associated with better HRQoL. We speculate that high fat and sugary diets might upregulate the reward pathway and alter neurochemical transmitters (dopamine, serotonin) with increased sense of well-being and pleasure.48 These associations of LDL-cholesterol and HbA1C levels with HRQoL were independent of complications. Although patients on high fat and sugar diets might feel fit, over time, suboptimal risk factor control will be translated to complications with HRQoL reductions. Patients with HDL-cholesterol <1.3 mmol/L and diastolic BP ≥75 mm Hg (markers of obesity) had suboptimal HRQoL. Parameters of liver dysfunction (low albumin), often associated with chronic poor-health,49 was also associated with decreased HRQoL.
Despite potential side effects, use of oral GLDs and ACE inhibitors was associated with better HRQoL than nonuse. In line with previous reports,50 HRQoL decrements were associated with increasing frequency of self-reported hypoglycemia episodes. Similar to the Dutch SPIRIT study,51 there was no difference in HRQoL between insulin and noninsulin users. In our study, patients treated with ARB also had better HRQoL than nonusers. Apart from proven organ-protective effects, ARB had neutral side effects compared to other BP-lowering drugs, which could limit their effectiveness due to poor adherence.52
Our study is not without limitations. Patients with lower baseline HRQoL might experience further decrements with occurrence of events although we did not have previous HRQoL measures for comparison. Over 80% of patients were attending hospital-based clinics and our results might not be representative of patients receiving primary care. Survival bias was possible as participants who died or those who were too ill would not undergo these assessments. That said, our results were largely in agreement with similar studies, with temporal associations as a novel feature.
Our study has multiple strengths. This is the first large-scale, prospective study in Asian patients with T2D spanning for 12 years. A real-world cohort has considerably less volunteer bias compared to participants of randomized controlled trials (RCTs). In this real-world register, we have accrued large number of events that could not have been captured in expensive RCTs with short follow-up duration. This analysis was based on patients enrolled from a single region. This had reduced regional variations in HRQoL rating as reported in multinational RCTs5, 44 or meta-analysis.53
5 CONCLUSIONS
In conclusion, our study provides temporal associations of HRQoL decrement with a comprehensive array of subtypes of cardiovascular-renal events in Chinese patients with T2D. By incorporating these temporal HRQoL estimates indicating the residual impacts of an index event in a simulation model, we can provide accurate estimation of the long-term cost-effectiveness of innovative interventions on an individual patient level in an Asian setting.
AUTHOR CONTRIBUTIONS
Juliana Lui, Juliana Chan, and Elaine Chow contributed to the study design. Juliana Lui conducted the analysis and drafted the manuscript. Juliana Chanis the principal investigator of the JADE Register and provided important clinical insights and results interpretation throughout the study. Eric Lau is the data manager of JADE and contributed to data curation and data cleaning. All authors contributed to data collection, interpretation of results, and revision of the manuscript and approved the final version for submission.
ACKNOWLEDGEMENTS
We express our gratitude to all participants of the JADE Register, collaborating doctors, nurses, and healthcare assistants for their contribution in establishing this 12-year cohort.
CONFLICT OF INTEREST STATEMENT
Juliana Chan reported receiving grants and/or honoraria for consultancy or giving lectures from Applied Therapeutics, AstraZeneca, Bayer, Boehringer Ingelheim, Celltrion, Eli Lilly, Hua Medicine, Powder Pharmaceuticals, Merck, MSD, Pfizer, Sanofi, Servier, Viatris, and Zuelig Pharma. She is the chief executive officer (pro bono) of the Asia Diabetes Foundation that developed the web-based JADE platform for implementation of data-driven diabetes care. She holds patents for using biomarkers to predict diabetes and its complications. She is the cofounder of GemVCare, a biotech company, with partial support from the Hong Kong Government, which uses biogenetic markers and information technology to implement precision diabetes care and prevention through partnerships. Juliana Chan is a member of the editorial board of the Journal of Diabetes and a coauthor of this article. To minimize bias, she was excluded from all editorial decision-making related to the acceptance of this article for publication. Alice Kong has received honorarium for consultancy or giving lectures from Abbott, Astra Zeneca, Bayer, Boehringer Ingelheim, Eli-Lilly, Kyowa Kirin, Merck Serono, Nestle, Novo-Nordisk, Pfizer, and Sanofi. Andrea Luk has received research grants and/or honorarium and/or served as a member of advisory panel for Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Lee's Pharmaceutical, MSD, Novo Nordisk, Roche, Sanofi, Sugardown Ltd, and Takeda, outside the submitted work. Ronald Ma has received research grants and/or honoraria for consultancy or giving lectures from AstraZeneca, Boehringer Ingelheim, Bayer, Kyowa Kirin, Merck, Novo Nordisk, Pfizer, Roche Diagnostics, and Tricida Inc. The proceeds have been donated to the Chinese University of Hong Kong, American Diabetes Association, and other charitable organizations to support diabetes research and education. The other authors declare no conflict of interest.
CONSENT FOR PUBLICATION
All authors have given consent for publication.