The epidemiological and clinical characteristics of COVID-19 patients admitted to a Fangcang shelter hospital in Beijing before the change in China's prevention and control policy
Xiaolong Xu, Hui Jiang, Maochen Li, and Jvjv Shang contributed equally.
Abstract
In November 2022, a large number of Omicron infections suddenly appeared in Beijing, but the epidemiological and clinical characteristics of the epidemic cases were unknown. We collected the data on COVID-19 cases in Fangcang Hospital in Beijing from November 20, 2022, to December 8, 2022, and analyzed the epidemiological and clinical characteristics. Of the enrolled study, 85.9% were asymptomatic and 14.1% were mild. Epidemiological data showed that the transmission speed of the Omicron variant was fast and the transmission range was wide, large-scale infections occurred in both rural and urban areas, and all age groups were susceptible to the Omicron variant. In addition, antipyretics and cough drugs were the two most used drugs, because 51.3% and 22.7% of patients had fever and cough, respectively, and 10.3% of patients took hypnotics. Furthermore, the proportion of patients with chronic diseases was low (13.9%), while the vaccination rate (71.2%) was relatively high. Based on the results, we found that most mild and asymptomatic cases did not need treatment, indicating that home isolation is correct and feasible. Although SARS-CoV-2 variants have characteristics such as high infectivity and immune-escape ability, the public should not be too afraid of COVID-19 infection; appropriate measures such as wearing masks and maintaining social distancing are sufficient to prevent reinfection.
1 INTRODUCTION
Since the outbreak of the COVID-19 epidemic at the end of 2019, the world has experienced several major outbreaks caused by different variants of concern (VOCs).1 Although COVID-19 vaccines were developed rapidly and the vaccination was actively advocated for, constant viral mutations affected the efficacy of approved vaccines.2 The infectivity and immune escape ability of SARS-CoV-2 variants constantly changed, which caused different disease characteristics in the epidemic dominated by the original strain to the Omicron variant, and the Omicron variant had higher infectivity and immune escape ability.3 In view of the high infectivity and pathogenicity of SARS-CoV-2, China still adhered strictly to epidemic prevention and control and took the safety and health of people as the priority before the launch of the “New Ten Rules” policy. The epidemic wave, in which the Omicron subvariant was dominant, in Shanghai and Guangzhou was successfully controlled and prevented through the “dynamic zeroing” strategy.4
Compared with the Delta variant, the severe cases and deaths caused by Omicron infections were about 0.4 times,5 only a few of patients with severe symptoms need treatment in hospital. In view of this, establishing shelter hospitals can provide adequate medical care and isolation conditions, to slow down the spread of the epidemic in society, and the medical sources were saved to alleviate the pressure of the medical system.6 In November 2022, a large number of Omicron infections suddenly appeared in Beijing, and the dominant variants in this wave were BA.5 and BF.7. Based on the data obtained from Fangcang shelter hospital in Shanghai and Jilin,7-9 most of the patients (~90%) had mild infections and recovered within 10 days after admission to the Fangcang shelter hospitals.6 Given the remarkable results achieved above, the government of Beijing established a series of Fangcang shelter hospitals in a short time to prevent and control the epidemic.
Before the release of the “New Ten Rules” policy (December 7, 2022), the Fangcang shelter hospital received about 20,000 COVID-19 patients, accounting for more than 70% of all confirmed cases. With the launch of the “New Ten Rules” policy, Fangcang shelter hospitals were closed on December 8, 2022, in Beijing, the mild and asymptomatic patients could have a home quarantine.
The “New Ten Rules” policy was launched by the government of China, aiming to prevent and control COVID-19 in a more accurate and scientific way, as well as reduce the adverse effect of COVID-19 on people's normal work and life (https://www.globaltimes.cn/page/202212/1281397.shtml). It was worth noting that the new policy allowed infected people to take a home quarantine rather than requiring hospital isolation and treatment.
In this study, we analyze and summarize the epidemiological, clinical characteristics, and laboratory results of COVID-19 cases admitted to Fangcang shelter hospitals at the initial stage of the epidemic in Beijing, supporting the home isolation of mild and asymptomatic patients. It is precisely because of the support of Fangcang shelter hospitals' clinical data that the most suitable epidemic prevention and control strategies can be formulated, which can not only protect the health of residents but also reduce the impact of COVID-19 on their lives. Although the WHO chief declared an end to COVID-19 as a global health emergency this May, many people have been reinfected recently, and how to prevent and control the reinfection once again became a spot of public attention. Our study not only summarizes the experience and past shortcomings but also provides suggestions for effective self-isolation in the future. In short, our study provides support and evidence for the country to formulate relevant policies.
2 RESULT
2.1 Patients with diabetes, as well as medical workers, were more susceptible
Between November 21 and December 8, 2022, 1307 patients involved in the survey were sent to the Fangcang shelter hospital for medical care and isolation. There were 1123 (85.9%) asymptomatic cases in the first group, followed by 184 (14.1%) mild cases in the second group. We got related data through the combination of the hospital database and call-back questionnaires (Figure 1). We analyzed the demographic characteristics, underlying medical conditions, and exposure history to determine the susceptible population. Of the patients, 738 (56.5%) were male, and the overall male-to-female ratio was 1.3:1, although this pattern was not uniform between the two groups. The median age was 38 (interquartile range [IQR]: 26–51), and the numbers of cases among those aged 25–49, 50–64, and 15–25 were 668 (51.1%), 260 (19.9%), and 197 (15.1%), respectively. The gender and age group distribution between the two groups was not statistically different (both p > 0.05, Table 1).

| Characteristics | All cases (N = 1307) | Asymptomatic cases (n = 1123, 85.9%) | Mild cases (n = 184, 14.1%) | p Value |
|---|---|---|---|---|
| Male | 738 (56.5) | 633 (56.4) | 105 (57.1) | 0.923 |
| Age, median years (IQR) | 38 (26–51) | 38 (26–51) | 37 (26–51) | 0.994 |
| Age group (year) | 0.325 | |||
| 0–4 | 17 (1.3) | 16 (1.4) | 1 (0.5) | |
| 5–14 | 72 (5.5) | 65 (5.8) | 7 (3.8) | |
| 15–25 | 197 (15.1) | 161 (14.3) | 36 (19.6) | |
| 25–49 | 668 (51.1) | 581 (51.7) | 87 (47.3) | |
| 50–64 | 260 (19.9) | 221 (19.7) | 39 (21.2) | |
| ≥65 | 93 (7.1) | 79 (7.0) | 14 (7.6) | |
| Underlying chronic medical conditionsa | ||||
| Any | 137/983 (13.9) | 110/839 (13.1) | 27/144 (18.8) | 0.094 |
| Hypertension | 89/983 (9.1) | 72/839 (8.6) | 17/144 (11.8) | 0.276 |
| Diabetes | 36/983 (3.7) | 25/839 (3.0) | 11/144 (7.6) | 0.012 |
| Asthma | 4/983 (0.4) | 3/839 (0.4) | 1/144 (0.7) | 1 |
| Chronic bronchitis | 6/983 (0.6) | 3/839 (0.4) | 3/144 (2.1) | 0.060 |
| COPD | 1/983 (0.1) | 1/839 (0.1) | 0/144 (0.0) | 1 |
| Chronic cardiac diseases | 11/983 (1.1) | 8/839 (1.0) | 3/144 (2.1) | 0.446 |
| Chronic liver diseases | 0/983 (0.0) | 0/839 (0.0) | 0/144 (0.0) | - |
| Chronic renal diseases | 3/983 (0.3) | 3/839 (0.4) | 0/144 (0.0) | 1 |
| Tumor | 4/983 (0.4) | 3/839 (0.4) | 1/144 (0.7) | 1 |
| Exposure historyb | ||||
| Yes | 636/750 (84.8) | 539/643 (83.8) | 97/107 (90.7) | 0.094 |
| Contacted with confirmed COVID-19 cases | 315/750 (42.0) | 266/643 (41.4) | 49/107 (45.8) | 0.451 |
| Cohabitation | 122/750 (16.3) | 102/643 (15.9) | 20/107 (18.7) | 0.553 |
| Space-time intersection | 175/750 (23.3) | 155/643 (24.1) | 20/107 (18.7) | 0.270 |
| Nosocomial infection | 24/750 (3.2) | 16/643 (2.5) | 8/107 (7.5) | 0.013 |
| No | 114/750 (15.2) | 104/643 (16.2) | 10/107 (9.3) | - |
- Note: Data are presented as n (%) of patients unless otherwise indicated.
- Abbreviation: IQR, inerquartile range.
- a Underlying chronic medical conditions: Due to the questionnaire filling status, 983 patients were included for the analysis of “Underlying chronic medical conditions.”
- b Exposure history: Due to the questionnaire filling status, 750 patients were included for the analysis of “Exposure history.”
Of the 983 cases, 13.9% had one or more underlying medical conditions. Hypertension (9.1%), diabetes (3.7%), and chronic cardiac diseases (1.1%) were the most common underlying medical conditions. In addition, 84.8% of patients had an exposure history, including contact with confirmed COVID-19 cases, cohabitation, space-time intersection, and nosocomial infection, accounting for 42.0%, 16.3%, 23.3%, and 3.2%, respectively. Moreover, there was no significant difference in underlying medical conditions and exposure history between different groups, except for diabetes and nosocomial infection, respectively (Table 1). And it meant that patients with diabetes, as well as medical workers, should take enough measures, like wearing masks, to avoid infection.
2.2 The infection rate was high in both rural and urban areas
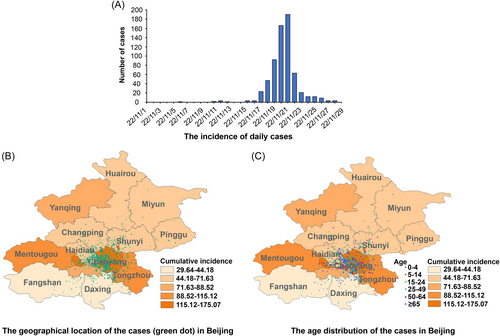
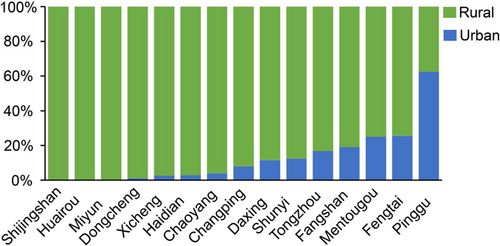
We collected the cases' sources to analyze the infection rate in different areas. It is shown that the occurrence time was concentrated between November 19 and 23 (≥40 cases per day, Figure 2A), and although the patients were distributed in the whole city, most cases were in urban areas (Figure 3). In terms of age distribution, there was no difference among different regions either (Figure 2B,C). In addition, the infection rate in some rural areas, such as those in Pinggu district can reach more than 60%, which was higher than in urban areas (Figure 3).
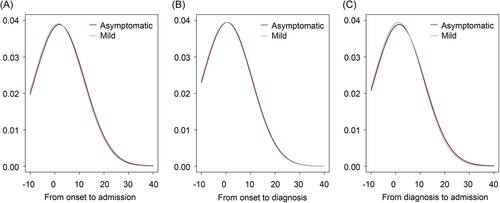
2.3 The time to event of mild and asymptomatic patients was similar
We compared the time to event of mild and asymptomatic patients to analyze the progress of infection and the correlation between the clinical classification and hospital admission. There was no significant difference between the median time from symptom onset to hospital admission, symptom onset to diagnosis, and diagnosis to hospital admission in the two groups (p > 0.05). Specifically, the median time from symptom onset to diagnosis and from symptom onset to hospital admission in the mild group were 0 days (p = 0.145) and 2 days (p = 0.133), respectively. The median time from diagnosis to hospital admission was both 1 day in two groups (p = 0.021, Figure 4). The above results showed that there was no significant difference in the symptom progress, and the appeared symptom was not correlated with delayed treatment.
2.4 A few patients received drug treatment
We collected a series of clinical indexes, including symptoms and treatment measures, to further study the disease characteristics. Fever (498/970, 51.3%), cough (220/970, 22.7%), and sore throat (209/970, 21.5%) were the most common symptoms and signs. Other symptoms included runny nose, nasal congestion, and muscular pain. Among the patients with mild symptoms, only 11.1% (145/1307) received the drug treatment, the drugs for common use included such categories: hypnotics, antiallergic drugs, gastrointestinal drugs, cough drugs, antiviral drugs, antipyretics, and antibiotics. Specifically, cough drugs (4.5%) were the most used, followed by antipyretics (2.9%) and gastroenteric drugs (1.9%). In addition, among the patients with drug treatment, 10.3% (15/145) took hypnotics, and only one took antiviral drugs (Table 2). The result meant the patients may be under high psychological pressure, which was caused by the discrimination of surrounding people and the public since the overall infection rate in Beijing was low before this epidemic wave.
| Characteristics | All cases (N = 1307) | Asymptomatic cases (n = 1123, 85.9%) | Mild cases (n = 184, 14.1%) | p Value |
|---|---|---|---|---|
| Symptoms and signsa | ||||
| Fever | 498/970 (51.3) | 402/832 (48.3) | 96/138 (69.6) | <0.001 |
| Cough | 220/970 (22.7) | 169/832 (20.3) | 51/138 (37.0) | <0.001 |
| Sore throat | 209/970 (21.5) | 169/832 (20.3) | 40/138 (29.0) | 0.029 |
| Runny nose | 40/970 (4.1) | 33/832 (4.0) | 7/138 (5.1) | 0.708 |
| Nasal congestion | 31/970 (3.2) | 26/832 (3.1) | 5/138 (3.6) | 0.963 |
| Muscular pain | 90/970 (9.3) | 75/832 (9.0) | 15/138 (10.9) | 0.591 |
| Fatigue | 49/970 (5.1) | 38/832 (4.6) | 11/138 (8.0) | 0.139 |
| Diarrhea | 18/970 (1.9) | 14/832 (1.7) | 4/138 (2.9) | 0.522 |
| Vomit | 8/970 (0.8) | 6/832 (0.7) | 2/138 (1.4) | 0.713 |
| Anosmia | 11/970 (1.1) | 8/832 (1.0) | 3/138 (2.2) | 0.417 |
| Ageustia | 20/970 (2.1) | 15/832 (1.8) | 5/138 (3.6) | 0.285 |
| Treatmentb | 0.041 | |||
| No | 1162 (88.9) | 1007 (89.7) | 155 (84.2) | - |
| Yes | 145 (11.1) | 116 (10.3) | 29 (15.8) | - |
| Hypnotics | 15 (1.1) | 13 (1.2) | 2 (1.1) | 1 |
| Antiallergic drug | 6 (0.5) | 5 (0.4) | 1 (0.5) | 1 |
| Gastroenteric drugs | 25 (1.9) | 21 (1.9) | 4 (2.2) | 1 |
| Cough drugs | 59 (4.5) | 43 (3.8) | 16 (8.7) | 0.006 |
| Antiviral drugs | 1 (0.1) | 1 (0.1) | 0 (0.0) | 1 |
| Antipyretics | 38 (2.9) | 34 (3.0) | 4 (2.2) | 0.688 |
| Antibiotics | 13 (1.0) | 9 (0.8) | 4 (2.2) | 0.181 |
- Note: Data are presented as n (%) of patients unless otherwise indicated.
- a Symptoms and signs: Due to the questionnaire filling status, 970 patients were included for the analysis of “Symptoms and signs.”
- b Treatment: All treatments were recorded, thus all patients were included in the analysis.
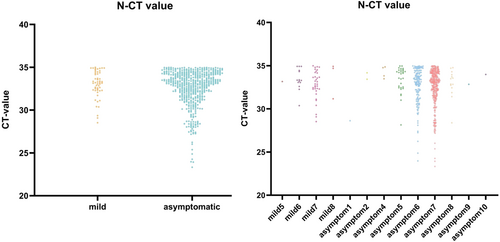
2.5 Most mild and asymptomatic patients received COVID-19 vaccines
We investigated the vaccination situation to ensure whether lighter symptoms were related to a higher inoculation rate. Of those, 71.2% of patients (930/1307) received at least one dose of the COVID-19 vaccine. Among the patients who received three doses of inactivated vaccines, 86.1% (618/718) and 13.9% (100/718) were asymptomatic and mild, respectively. In the 3-dose vaccinees, the proportion of those who received adenovirus vector vaccine, recombinant protein vaccine, and messenger RNA vaccine was 0.1% (1/738), 1.5% (11/738), and 0.5% (4/738), respectively. Although the government previously advocated the sequential immunization strategy (i.e., vaccination with different types of vaccines, such as inactivated vaccine + adenovirus vector vaccine or inactivated vaccine + recombinant protein vaccine2), only 0.4% of patients have received heterologous inoculation (Table 3). In addition, from the laboratory result, there was no significant difference between the Ct values of mild and asymptomatic patients, as well as the patients with different discharge times (Figure 5). The result meant that at least 1-dose inoculation can effectively attenuate the symptom classification.
| Yes (n = 930, 71.2%)a | No (n = 67, 5.1%)a | Refused (n = 310, 23.7%)a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Full course vaccination (n = 738, 79.4%) | Nonfull course (n = 180, 19.4%) | ||||||||||
| Inactivated vaccine (n = 718, 97.3%) | Adenovirus vaccine (n = 1, 0.1%) | protein vaccine (n = 11, 1.5%) | RNA vaccine (n = 4, 0.5%) | Sequential inoculation (n = 3, 0.4%) | Inactivated vaccine (n = 177, 98.3%) | Adenovirus vaccine (n = 2, 1.1%) | protein vaccine (n = 1, 0.6%) | RNA vaccine (n = 0, 0%) | |||
| Asymptomatic cases | 618 (86.1) | 1 (100.0) | 9 (81.8) | 4 (100.0) | 3 (100.0) | 147 (83.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 57 (85.1) | 273 (88.1) |
| Mild cases | 100 (13.9) | 0 (0.0) | 2 (18.2) | 0 (0.0) | 0 (0.0) | 30 (16.9) | 2 (100.0) | 1 (100.0) | 0 (0.0) | 10 (14.9) | 37 (11.9) |
- Note: Data are presented as n (%) of patients unless otherwise indicated.
- a Among all participants, 930 patients declared a certain inoculation (at least one dose), 67 declared no inoculation and 310 did not fill the “Vaccination” part in the questionnaire.
3 DISCUSSION
In the past epidemic wave in Beijing, although the Omicron variant spread rapidly, and caused many infections in a short time, Beijing strictly abided by “dynamic zeroing” prevention and control measures. To ensure COVID-19 patients can be treated and isolated in a timely manner, 23 Fangcang shelter hospitals were established in a very short time.
In this study, we conducted a series of analyses on the COVID-19 cases in the Fangcang shelter hospitals and observed that large-scale infections occurred in both rural and urban areas, and all age groups were susceptible to the Omicron variant. Most cases were mild and asymptomatic and could be cured by taking conventional drugs, indicating that it is feasible and reliable to change the previous centralized isolation strategy to home isolation, which can save medical resources as well as reduce the social burden and public panic.
Early detection, diagnosis, and treatment are the basis for controlling and eliminating infectious diseases. In this epidemic wave, the average time of onset-admission, onset-diagnosis, and diagnosis-admission of asymptomatic and mild patients was only 2, 0, and 1 day, respectively, indicating that the infected people were effectively controlled in a short time, further blocking the social transmission of the epidemic. Such a fast response speed is inseparable from the “dynamic zeroing” prevention and control measures. With the release of the “New Ten Rules” policy, mild and asymptomatic cases can take home quarantines, increasing the risk of virus transmission in society. Under this situation, how to effectively prevent and control the epidemic once again became the focus. Vaccination is the most effective method to prevent and control infectious diseases, 74% of the COVID-19 patients were full-vaccinated in the study, of which 97% received the inactivated vaccine. The COVID-19 vaccination can cause extensive cellular immunity or memory cell reaction, which is one of the reasons for the small number of severe cases in Beijing. Considering that other types of vaccines, such as adenovirus vector vaccines or recombinant protein vaccines, can induce extensive helper T cell responses and germinal center B cell responses, thus providing longer-time protection,2, 10-12 it is recommended that the sequential immunization should be taken to effectively prevent the reinfection of Omicron subvariant for both convalescent and uninfected population.
In this wave of the Omicron epidemic, more than half of the patients suffered from fever, but only a few cases used antibiotics, which was very different from the wide use of antibiotics in the early treatment of COVID-19 cases.13 After a 3-year fighting with COVID-19, the understanding of COVID-19 in clinical practice was deeper and the treatment was more scientific. Except for secondary lung bacterial infection, COVID-19 cases no longer relied on antibiotics for treatment. To our surprise, in addition to common antipyretics and cough drugs, 10.3% of patients (15/145) took hypnotics, reflecting that they had great mental pressures. Since the overall infection rate in Beijing was low before this wave of the epidemic, COVID-19 patients were lacking a general understanding of Omicron infection and may be discriminated against by the surrounding people and the public, thus had psychological pressure to bring burden and inconvenience to other people. The release of the “New Ten Rules” not only enabled people to understand the infection more scientifically and eliminate the discrimination of COVID-19 patients but also provided a more comfortable and reassuring environment for mild and asymptotic cases by home isolation, which is conducive to recovery. Moreover, it should not be ignored that although drug interventions such as antipyretics and cough drugs can alleviate the symptom in a short time, they cannot effectively inhibit viral infection and shorten the disease course,14 severe cases still need antiviral treatment. At present, the possible adverse effects of approved antiviral drugs (such as Molnupiravir, a SARS-CoV-2 RdRp inhibitor,15 Paxlovid, a 3CL protein inhibitor,16 and Azvudine, a nucleoside analog that inhibits RdRp) cannot be ignored; therefore, antiviral treatment should be carried out under the guidance of doctors for patients with excessive viral load and serious clinical complications, and reduce the risk of hospital critical illness or death.
From the laboratory result, there was no significant difference between the Ct values of mild and asymptomatic patients, as well as the patients with different discharge times, indicating that it may be unreasonable to uniformly carry out nucleic acid tests after 5-day isolation, and a considerable number of patients may have a converted negative PCR result before the test. Therefore, it is necessary to infer the time of PCR results turning negative according to the patient's admission indicators, such as Ct value and symptoms, and conduct timely detection to reduce the waste of medical resources and relieve the pressure on the medical system. In addition, continuous nucleic acid detection has consumed a lot of human and financial resources,17 which has seriously affected the normal life of people. The release of the “New Ten Rules” ended the long-term high pressure in epidemic prevention and control, facilitating people's lives, but also increasing the risk of social virus transmission. Therefore, hospitals should not only make full preparations to deal with the possible shortage of resources but also use antiviral drugs appropriately for cases with chronic diseases to reduce the severity of the disease or mortality.18 In addition, the World Health Organization has announced that COVID-19 was no longer a global health emergency, but the risk of new variants emerging should not be ignored. According to the data collected by the Chinese Center for Disease Control and Prevention, the SARS-CoV-2 reinfection rate has an increasing trend recently (https://en.chinacdc.cn/), so it is also necessary to take measures including wearing masks and maintaining social distancing. Although the public is no longer afraid of COVID-19 infection, it is still necessary to store some antipyretics and antiviral drugs appropriately. In addition, once infected with the SARS-CoV-2 virus, the public needs to closely monitor their own health status, and immediately go to the hospital when the severe symptom appears.
This study had some limitations. First, we only collected data on mild and asymptomatic cases, and severe and death cases were not included in the study; thus, a comprehensive comparison of COVID-19 cases was not possible. Second, we only collected information on COVID-19 cases in Beijing, which limited our ability to describe the differences in cases in different regions. Third, not all COVID-19 cases information on Fangcang shelter hospitals has been collected, which may cause bias. However, the most important factors have been collected.
In conclusion, our study reflected the epidemiological and clinical characteristics of COVID-19 cases during the early Omicron epidemic wave in Fangcang shelter hospital in Beijing, and we found that no severe cases of death happened in the Fangcang shelter hospital and most cases did not need treatment, which indicates that the “New Ten Rules” policy is correct and feasible. However, the transmission speed of the Omicron variant is fast and the transmission range is wide, and all age groups are susceptible; reinfection is prone to occur, thus the awareness of prevention and control should not be relaxed. It is necessary to wear masks and maintain social distancing. In addition, in the case of respiratory symptoms such as cough and fever, the public should be alert to whether it is COVID-19 reinfection. Once confirmed, it is necessary to take suitable measures, such as self-isolation and medication. Moreover, never put immense psychological stress on COVID-19 infection and never refuse the necessary medical assistance. Only in the above manner, can we better respond to possible outbreak risks in the future.
4 MATERIALS AND METHODS
4.1 Study design and participants
This is a retrospective study including a total of 1307 mild and asymptomatic cases of Omicron infection in Beijing between November 20, 2022, to December 8, 2022. All cases were diagnosed based on the diagnosis and treatment protocol of the National Health Commission of the People's Republic of China (9th edition). All enrolled cases were tested positive for SARS-CoV-2 by reverse transcription polymerase chain reaction (RT-PCR; Ct value < 35) or antigen test, and were admitted to the Fangcang shelter hospital within 2–5 days after the positive antigen or PCR result. After a 5-day isolation, nucleic acid test was performed, and the patients could be discharged after two consecutive negative PCR results (Ct value > 35, Figure 1). No deaths or severe cases occurred during the study.
4.2 Case definition
Asymptomatic case: (1) positive for SARS-CoV-2 by RT-PCR Or positive for immunoglobulin G (IgG) and immunoglobulin M (IgM) antibody in nonvaccinated cases; (2) no clinical symptoms or mild clinical symptoms with short duration, and no symptoms at the time of admission to the Fangcang shelter hospital.
Mild case: (1) positive for SARS-CoV-2 by RT-PCR Or positive for IgG and IgM antibody in non-vaccinated cases; (2) mild clinical symptoms and still exist at the time of admission to Fangcang shelter hospital.
4.3 Data collection
We collected the demographic, epidemiological, clinical, and laboratory data of 1307 cases using standardized forms. We also collected symptom onset time, diagnosis time, and hospital admission time, and detailed information regarding the questionnaire will be available after the request. Based on the symptoms, we divided the total cases into two groups, namely the symptomatic group and the asymptomatic group.
All participants provided oral informed consent, and the patients who were invited can accept or reject the questionnaire freely. For participants under 18 years old or lacking the capacity to approve verbal consent, consent was provided by parents or legal guardians on behalf of patients. Since it is a retrospective study, the information was collected through the call-back, if the patient agrees to provide relevant information for research, then we will use the data collected in hospital databases or through the call-back. Most patients were admitted to the Fangcang hospital from November to December 2022, and some experienced the release of “New Ten Rules,” in which time the medical resource was short, and related patients' data were not collected in time. Therefore, we conducted this retrospective research and did the collection by combining hospital data and call-back results with the verbal consent of patients.
The authors designed the study, collected and analyzed the data, and vouch for the completeness and accuracy of the data and the fidelity of the study.
4.4 Statistical analysis
Descriptive statistical methods were adopted to analyze the continuous variables and categorical variables for mild and asymptomatic cases, respectively. The differences between the two groups were compared by χ2 test. We fitted the parametric distribution (Weibull, Gamma, and Logistic-normal) and nonparametric (kernel density) distributions to the time from symptom onset to diagnosis, symptom onset to admission, diagnosis to admission, and selected the best model to the time from symptom onset to diagnosis. Model fitness was visually examined by comparing fitted density curves to the observed frequencies, and parametric distributions followed were compared using the Akaike information criteria if necessary. We used ArcGIS (Arc Map, version 10·2; ESRI Inc.) to explore the distribution patterns of COVID-19 cases in different areas. The ordinarily one-way analysis of variance was used to analyze the difference in Ct value between asymptomatic and mild patients. In addition, according to the zoning code and urban-rural zoning code for statistics in 2012 from the National Bureau of Statistics of China, we divided the patient's addresses into two parts: urban areas and rural areas.
SAS (version 9.4) and R project (version 3.63.0) were used for data extraction, sorting, cleaning, and the rest of further data management and analysis. All statistical tests were two-sided with a significance level of p < 0.05.
AUTHOR CONTRIBUTIONS
Bo Li, Huahao Fan, and Qingquan Liu contributed to the study concept and design; Xiaolong Xu, Yifan Shi, Yumeng Yan, Chunxia Zhao, and Chongpei Cen led the acquisition of clinical data; Hui Jiang, and Maochen Li led the statistical analysis and interpretation of data; Jvjv Shang, Xintong Li, Shuang Song, and Chunxia Zhao participated in the case-discussion and gave suggestion in the analysis; Xiaolong Xu, Hui Jiang, and Maochen Li drafted the manuscript and Xiaolong Xu, Hui Jiang, Maochen Li, Jvjv Shang, and Huahao Fan revised the manuscript. All authors have read and approved the final manuscript.
ACKNOWLEDGMENTS
We thank the participants in this study for their help in data collection, we also thank all medical workers for their contribution to the study. Qingquan Liu declares grants from the National Multidisciplinary Innovation Team Project of Traditional Chinese Medicine (No. ZYYCXTD-D-202201), National Natural Science Foundation of China (No. 82141202). Huahao Fan declares grants from the National Key Research and Development Program of China (grant no. 20SWAQK22, 2020YFA0712102), National Natural Science Foundation of China (grant no. 82151224), Fundamental Research Funds for Central Universities (grant no. BUCTZY2022), and H&H Global Research and Technology Center (grant no. H2021028).
CONFLICT OF INTERESTS STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
The Ethics Review Committee of the Beijing hospital of Traditional Chinese Medicine, Capital Medical University provided approval for this study (No: 2022BL02-044-02). Additionally, patients' personal identifying information was anonymized to ensure privacy and all participants provided oral informed consent. The study obtained approval from the Ethics Review Committee for the use of verbal consent.
Open Research
DATA AVAILABILITY STATEMENT
The original data of the study are available upon request.




