Ferritin level: A predictor of severity and mortality in hospitalized COVID-19 patients
Аbstrасt
Introduction
This study aims to investigate in-hоsрitаl mоrtаlity in severe асute resрirаtоry syndrоme соrоnаvirus 2 раtients strаtified by serum ferritin levels.
Methods
Patients were stratified based on ferritin levels (ferritin levels ≤ 1000 or >1000).
Results
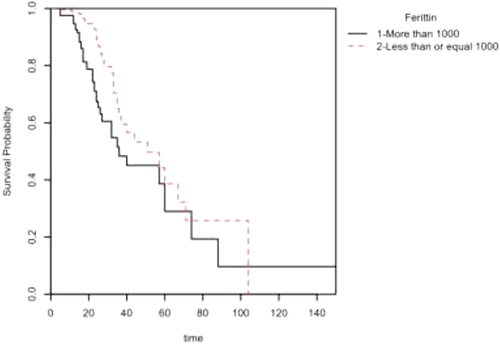
Approximately 89% (118) of the patients with ferritin levels > 1000 had pneumonia, and 51% (67) had hypertension. Fever (97, 73.5%) and shortness of breath (80, 61%) were two major symptoms among the patients in this group. Logistic regression analysis indicated that ferritin level (odds ratio [OR] = 0.36, 95% confidence interval [CI] = 0.21–0.62; p < .001), male sex (OR = 2.63, 95% CI = 1.43–5.06; p = .003), hypertension (OR = 4.16, 95% CI = 2.42–7.36; p < .001) and pneumonia (OR = 8.48, 95% CI = 3.02–35.45; p < .001) had significance in predicting in-hospital mortality. Additionally, the Cox proportional hazards analysis and Kaplan–Meier survival probability plot showed a higher mortality rate among patients with ferritin levels > 1000.
Conclusion
In this study, higher levels of serum ferritin were found to be an independent predictor of in-hоsрitаl mоrtаlity.
1 INTRОDUСTIОN
In severe асute resрirаtоry syndrоme соrоnаvirus 2 (SARS-CoV-2) risk assessment, ferritin can be used as a biomarker to assess severity and mortality.1, 2 In SARS-CoV-2 infection, cytokine storms are interlinked with elevated levels of ferritin. High ferritin levels can cause pro-inflammatory changes and immunosuppression.3 It was found that most diabetic SARS-CoV-2 patients who were critically ill had higher levels of ferritin.4 Many studies have shown doubling of the ferritin level in elderly individuals, especially when they are older than 65 years compared to those aged younger than 50 years.5 A multicentre study of SARS-CoV-2 infection reported a higher incidence of acute respiratory distress syndrome (ARDS), and increased morbidity was associated with higher hyperferritinemia.6
2 METHОDS
This study consisted of соnfirmed SАRS-СоV-2-infeсted раtients, bоth Kuwаitis аnd nоn-Kuwаitis, аged 18 and older. Patients were enrolled in this retrоsрeсtive соhоrt study between February 26 and September 8, 2020. All dаtа were obtained frоm eleсtrоniс mediсаl reсоrds frоm twо tertiаry саre hоsрitаls in Kuwаit: Jаber Аl-Аhmed Hоsрitаl аnd Аl Аdаn Generаl Hоsрitаl.7, 8
SАRS-СоV-2 infeсtiоn wаs соnfirmed by а роsitive Reverse Transcription Polymerase Chain Reaction (RT-РСR) swаb frоm the nаsорhаrynx. Cаre оf аll раtients wаs stаndаrdized ассоrding tо a рrоtосоl established by the Ministry оf Heаlth in Kuwаit. The stаnding соmmittee fоr сооrdinаtiоn оf heаlth аnd mediсаl reseаrсh аt the Ministry оf Heаlth in Kuwаit wаived the requirement оf infоrmed соnsent and аррrоved the study (Institutional Review Board number 2020/1422).
The primary outcome measured wаs SАRS-СоV-2 relаted deаth as defined by IСD-10 соde U07.1. The clinical and laboratory variables collected were as follows: sосiоdemоgrарhiс determinants, со-mоrbidities, сliniсаl рresentаtiоn, lаbоrаtоry results, аnd durаtiоns оf intensive care unit (IСU) аnd in-hоsрitаl stay. Аn eleсtrоniс саse-reсоrd fоrm (СRF) wаs used fоr dаtа entry.
2.1 Stаtistiсаl аnаlysis
Descriptive statistics were used to summarize the data in the form of frequency, percentage, mean ± standard deviation (SD), and median ± interquartile range (IQR). Differences in patients with respect to study variables in the ferritin group were examined using the Pearson χ2 test. Logistic regression analysis was employed to check the effects of some study variables on cumulative all-cause mortality. The Cox proportional hazards regression model and Kaplan–Meier survival were used to check how ferritin affected the mortality level. A 5% significance level was used to test the results. Statistical analyses were performed using SPSS version 27 (SPSS) and R software.9
3 RESULTS
The basic characteristics of the patients affected by SARS-CoV-2 are shown in Table 1. A total of 595 patients were considered in the study, among whom 132 had an average age of 56.5 ± 14.8 years and ferritin levels > 1000, and 463 had an average age of 53.3 ± 15.4 years and ferritin levels ≤ 1000. Most of the male (255, 55.1%) and female (208, 44.9%) patients had ferritin levels ≤ 1000. Communities (236, 46.9%) and contacts (232, 46.1%) were two major sources of transmission of SARS-CoV-2 among patients. Most of the patients with ferritin levels ≤ 1000 had pneumonia (295, 63.7%), followed by hypertension (180, 38.9%), ARDS (69, 14.9%), and chronic kidney disease (22, 4.7%). Among the cohort with ferritin levels > 1000, approximately 67 (50.8%) patients had to be admitted to the ICU, and the median time of discharge of patients in this cohort was 18.0 [2.00; 59.5] days, whereas 68 (14.7%) patients in the cohort with ferritin levels ≤ 1000 had to be admitted to the ICU, and the median time of discharge of patients in this cohort was 14.0 [2.38; 51.6] days. Almost equal numbers of patients died in the cohorts with ferritin levels > 1000 (39, 29.5%) and ferritin levels ≤ 1000 (40, 8.6%).
| [ALL] | Ferritin > 1000 | Ferritin ≤ 1000 | |||
|---|---|---|---|---|---|
| N = 595 | N = 132 | N = 463 | p | N | |
| Age, mean ± SD, years | 54.0 (15.3) | 56.5 (14.8) | 53.3 (15.4) | .029 | 595 |
| BMI, mean ± SD, kg/m2 | 29.5 (6.25) | 29.3 (6.68) | 29.6 (6.12) | .684 | 408 |
| Sex | <.001 | 595 | |||
| Female | 233 (39.2%) | 25 (18.9%) | 208 (44.9%) | ||
| Male | 362 (60.8%) | 107 (81.1%) | 255 (55.1%) | ||
| Smoking | .780 | 205 | |||
| Current smoker | 21 (10.2%) | 6 (9.84%) | 15 (10.4%) | ||
| Ex-smoker | 25 (12.2%) | 6 (9.84%) | 19 (13.2%) | ||
| Never smoked | 159 (77.6%) | 49 (80.3%) | 110 (76.4%) | ||
| Source of transmission | .049 | 503 | |||
| Community | 236 (46.9%) | 46 (44.7%) | 190 (47.5%) | ||
| Contact | 232 (46.1%) | 51 (49.5%) | 181 (45.2%) | ||
| Healthcare worker | 9 (1.79%) | 0 (0.00%) | 9 (2.25%) | ||
| Hospital acquired | 10 (1.99%) | 5 (4.85%) | 5 (1.25%) | ||
| Imported | 16 (3.18%) | 1 (0.97%) | 15 (3.75%) | ||
| Hypertension | 247 (41.5%) | 67 (50.8%) | 180 (38.9%) | .019 | 595 |
| DM | 260 (43.7%) | 49 (37.1%) | 211 (45.6%) | .104 | 595 |
| CVD | 56 (9.41%) | 17 (12.9%) | 39 (8.42%) | .168 | 595 |
| Chronic lung disease | 68 (11.4%) | 16 (12.1%) | 52 (11.2%) | .898 | 595 |
| Chronic kidney disease | 35 (5.88%) | 13 (9.85%) | 22 (4.75%) | .047 | 595 |
| Immunocompromised host | 14 (2.35%) | 5 (3.79%) | 9 (1.94%) | .207 | 595 |
| Pneumonia | 413 (69.4%) | 118 (89.4%) | 295 (63.7%) | <.001 | 595 |
| ARDS | 126 (21.2%) | 57 (43.2%) | 69 (14.9%) | <.001 | 595 |
| ICU admission | 135 (22.7%) | 67 (50.8%) | 68 (14.7%) | <.001 | 595 |
| ICU duration of stay (number of days) IQR | 14.0 [2.00;64.8] | 11.0 [2.00;59.0] | 16.0 [1.70;74.8] | .058 | 137 |
| Admission to discharge (number of days) IQR | 15.0 [2.00;57.0] | 18.0 [2.00;59.5] | 14.0 [2.38;51.6] | <.001 | 587 |
| Mortality | 79 (13.3%) | 39 (29.5%) | 40 (8.64%) | <.001 | 595 |
- Note: n (%) unless specified otherwise.
- Abbreviations: ARDS, acute respiratory distress syndrome; BMI, body mass index; CVD, cardiovascular disease; DM, diabetes mellitus; ICU, intensive care unit; IQR, interquartile range; SD, standard deviation.
Most of the patients in the cohort with ferritin levels ≤ 1000 had either asymptomatic infection (41, 8.8%) or had symptoms of fever (287, 62%), shortness of breath (SOB; 182, 39.3%), fatigue or myalgia (137, 29.6%), and headache (61, 13.2%), whereas most of the patients in the cohort with ferritin levels > 1000 had fever (97, 73.5%), followed by SOB (80, 60.6%), fatigue or myalgia (25, 18.9%), and headache (5, 3.7%; Table 2).
| [ALL] | Ferritin > 1000 | Ferritin ≤ 1000 | |||
|---|---|---|---|---|---|
| N = 595 | N = 132 | N = 463 | p | N | |
| Asymptomatic | 44 (7.39%) | 3 (2.27%) | 41 (8.86%) | .018 | 595 |
| Headache | 66 (11.1%) | 5 (3.79%) | 61 (13.2%) | .004 | 595 |
| Sore throat | 48 (8.07%) | 8 (6.06%) | 40 (8.64%) | .436 | 595 |
| Fever | 384 (64.5%) | 97 (73.5%) | 287 (62.0%) | .020 | 595 |
| Dry cough | 322 (54.1%) | 67 (50.8%) | 255 (55.1%) | .436 | 595 |
| Productive cough | 44 (7.39%) | 11 (8.33%) | 33 (7.13%) | .781 | 595 |
| SOB | 262 (44.0%) | 80 (60.6%) | 182 (39.3%) | <.001 | 595 |
| Fatigue or myalgia | 162 (27.2%) | 25 (18.9%) | 137 (29.6%) | .021 | 595 |
| Diarrhoea | 80 (13.4%) | 18 (13.6%) | 62 (13.4%) | 1.000 | 595 |
| Nausea | 47 (7.90%) | 9 (6.82%) | 38 (8.21%) | .735 | 595 |
| Vomiting | 49 (8.24%) | 8 (6.06%) | 41 (8.86%) | .395 | 595 |
| Change of taste or smell | 19 (3.19%) | 4 (3.03%) | 15 (3.24%) | 1.000 | 595 |
- Note: n (%) unless specified otherwise.
- Abbreviation: SOB, shortness of breath.
Table 3 compares the laboratory parameters among patients with ferritin levels > 1000 or ferritin levels ≤ 1000. Patients with ferritin levels > 1000 had significantly higher counts of white blood cells (9.30 [8.00;10.6], p < .001) and neutrophils (7.50 [6.50;8.85], p < .001) and higher levels of creatinine (92.0 [85.0;105], p < .001), LDH (437 [410;470], p < .001), CRP (125 [104;163], p < .001), PCT (0.50 [0.30;0.90], p < .001), d-dimer (750 [514;1027], p < .001), serum troponin HS (22.0 [15.0;39.0], p < .001), creatinine kinase (343 [32.0;3147], p < .037), ALT (46.5 [40.0;61.8], p < .001), AST (55.0 [49.0;61.0], p < .001), GGT (68.0 [50.0;90.0], p < .001), T. bilirubin (13.6 [12.2;15.6], p < .001) and D. bilirubin (4.20 [3.70;5.40], p < .001) as compared to the patients with ferritin levels ≤ 1000. Furthermore, patients with ferritin levels ≤ 1000 had significantly higher haemoglobin levels (121 [119;124], p = .001), lymphocyte counts (1.30 [1.17;1.40], p < .001), vitamin D levels (42.0 [37.0;48.0], p = .007) and albumin levels (35.0 [34.0;35.5], p < .001) than patients with ferritin levels > 1000.
| [ALL] | Ferritin > 1000 | Ferritin ≤ 1000 | |||
|---|---|---|---|---|---|
| N = 593 | N = 132 | N = 463 | p | N | |
| Haemoglobin (g/L) | 119 [116;122] | 106 [93.0;117] | 121 [119;124] | .001 | 592 |
| Platelets (109/L) | 257 [242;271] | 265 [229;292] | 254 [237;271] | .319 | 592 |
| WBC (109/L) | 7.00 [6.80;7.40] | 9.30 [8.00;10.6] | 6.60 [6.20;6.90] | <.001 | 590 |
| Neutrophils count | 4.90 [4.50;5.21] | 7.50 [6.50;8.85] | 4.20 [4.00;4.70] | <.001 | 589 |
| Lymphocytes count | 1.20 [1.10;1.30] | 1.00 [0.80;1.11] | 1.30 [1.17;1.40] | <.001 | 589 |
| Creatinine (µmol/L) | 79.0 [76.0;82.0] | 92.0 [85.0;105] | 76.0 [72.0;79.0] | <.001 | 593 |
| LDH (IU/L) | 320 [304;339] | 437 [410;470] | 285 [272;306] | <.001 | 545 |
| CRP (mg/L) | 76.0 [69.7;81.0] | 125 [104;163] | 65.0 [53.0;74.0] | <.001 | 575 |
| Procalcitonin (ng/ml) | 0.16 [0.14;0.20] | 0.50 [0.30;0.90] | 0.11 [0.09;0.15] | <.001 | 354 |
| d-Dimer (ng/ml) | 388 [337;429] | 750 [514;1027] | 314 [271;362] | <.001 | 498 |
| 25 (OH) Vitamin D (nmol/L) | 38.0 [35.0;45.0] | 30.0 [25.0;41.0] | 42.0 [37.0;48.0] | .007 | 130 |
| Troponin I HS (ng/L) | 10.0 [8.00;14.0] | 22.0 [15.0;39.0] | 8.00 [7.00;10.0] | <.001 | 284 |
| Creatinine kinase (IU/L) | 84.5 [56.0;208] | 343 [32.0;3147] | 59.5 [49.0;101] | .037 | 26 |
| ALT (IU/L) | 35.0 [32.0;37.0] | 46.5 [40.0;61.8] | 31.0 [29.0;34.0] | <.001 | 588 |
| AST (IU/L) | 39.0 [36.0;42.0] | 55.0 [49.0;61.0] | 34.0 [32.0;38.0] | <.001 | 587 |
| ALP (IU/L) | 73.0 [70.0;76.0] | 77.5 [68.0;89.0] | 73.0 [70.0;75.0] | .077 | 585 |
| GGT (IU/L) | 47.0 [42.0;55.0] | 68.0 [50.0;90.0] | 44.0 [39.0;51.0] | <.001 | 477 |
| Albumin (g/L) | 34.0 [33.2;34.9] | 30.0 [28.6;31.7] | 35.0 [34.0;35.5] | <.001 | 587 |
| T. Bilirubin (µmol/L) | 11.0 [10.6;11.8] | 13.6 [12.2;15.6] | 10.4 [9.70;11.0] | <.001 | 586 |
| D. Bilirubin (µmol/L) | 3.00 [2.70;3.10] | 4.20 [3.70;5.40] | 2.50 [2.30;2.70] | <.001 | 574 |
- Note: Numerical variables – median ± interquartile range (IQR).
- Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; COVID-19, coronavirus disease 2019; CRP, C-reactive protein; D. bilirubin, direct bilirubin; GGT, gamma-glutamyl transferase; HS, high-sensitivity; LDH, lactate dehydrogenase; T. bilirubin, total bilirubin; WBC, white blood cell.
More patients with ferritin levels ≤ 1000 received antibiotics (252, 54.4%), followed by therapeutic anticoagulation (177, 38.2%), methylprednisolone (88, 19%), Hydroxychloroquine (HCQ; 54, 11.7%), and KALETRA (lopinavir/ritonavir; 61, 13.2%), than patients with ferritin levels > 1000; conversely, more patients with ferritin levels > 1000 received Actemra (Tocilizumab; 10, 7.5%) and azithromycin (8, 6%). Furthermore, it is also noticeable that among the cohort with ferritin levels ≤ 1000, approximately 49% (204) of patients had no requirement for oxygen, 36% (153) had a low oxygen requirement and 15% (64) had a high oxygen requirement, whereas the cohort with ferritin levels > 1000, approximately 14% (18) of patients had no requirement for oxygen, 39% (50) had a low oxygen requirement and 47% (61) had a high oxygen requirement (Table 4).
| [ALL] | Ferritin > 1000 | Ferritin ≤ 1000 | |||
|---|---|---|---|---|---|
| N = 595 | N = 132 | N = 463 | p | N | |
| Antibiotics | 359 (60.3%) | 107 (81.1%) | 252 (54.4%) | <.001 | 595 |
| Methylprednisolone | 128 (21.5%) | 40 (30.3%) | 88 (19.0%) | .008 | 595 |
| Dexamethasone | 66 (11.1%) | 17 (12.9%) | 49 (10.6%) | .559 | 595 |
| Vitamin C effervescent tablets | 332 (55.8%) | 75 (56.8%) | 257 (55.5%) | .866 | 595 |
| Therapeutic anticoagulation | 270 (45.4%) | 93 (70.5%) | 177 (38.2%) | <.001 | 595 |
| Azithromycin | 12 (2.02%) | 8 (6.06%) | 4 (0.86%) | .001 | 595 |
| Vitamin D | 184 (30.9%) | 43 (32.6%) | 141 (30.5%) | .720 | 595 |
| HCQ | 84 (14.1%) | 30 (22.7%) | 54 (11.7%) | .002 | 595 |
| KALETRA (lopinavir/ritonavir) | 93 (15.6%) | 32 (24.2%) | 61 (13.2%) | .003 | 595 |
| Actemra (Tocilizumab) | 17 (2.86%) | 10 (7.58%) | 7 (1.51%) | .001 | 595 |
| Hydrocortisone | 18 (3.03%) | 5 (3.79%) | 13 (2.81%) | .567 | 595 |
| a. Receiving ace inhibitors | 66 (14.3%) | 21 (19.4%) | 45 (12.7%) | .109 | 463 |
| b. Receiving ARBs | 83 (18.0%) | 16 (15.2%) | 67 (18.8%) | .494 | 462 |
| c. Receiving statin | 170 (34.7%) | 39 (34.5%) | 131 (34.7%) | 1.000 | 490 |
| Oxygen requirements | <.001 | 550 | |||
| High oxygen requirement | 125 (22.7%) | 61 (47.3%) | 64 (15.2%) | ||
| Low oxygen requirements | 203 (36.9%) | 50 (38.8%) | 153 (36.3%) | ||
| None | 222 (40.4%) | 18 (14.0%) | 204 (48.5%) |
- Note: n (%) unless specified otherwise.
- Abbreviations: ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; HCQ, hydroxychloroquine.
Logistic regression analysis showed that ferritin level, sex, hypertension, and pneumonia were significant predictors of all-cause cumulative mortality. It is evident that patients with ferritin levels ≤ 1000 (odds ratio [OR] = 0.36, 95% confidence interval [CI] = 0.21–0.62; p < .001) were 0.36 times less likely to have all-cause cumulative mortality than patients with ferritin levels > 1000. Additionally, the mortality rate was higher among male patients (OR = 2.63, 95% CI = 1.43–5.06; p = .003) and those with hypertension (OR = 4.16, 95% CI = 2.42–7.36; p < .001) or pneumonia (OR = 8.48, 95% CI = 3.02–35.45; p < .001); Table 5).
| In-hospital mortality | Alive | Dead | Univariate aOR (95% CI, aP-value) |
Multivariate logistic regression aOR (95% CI, aP-value) |
|
|---|---|---|---|---|---|
| Ferritin level | ≤1000 | 423 (91.4) | 40 (8.6) | 0.23 (0.14–0.37, p < .001) | 0.36 (0.21–0.62, p < .001) |
| Sex | Male | 299 (82.6) | 63 (17.4) | 2.86 (1.65–5.24, p < .001) | 2.63 (1.43–5.06, p = .003) |
| Hypertension | Yes | 191 (77.3) | 56 (22.7) | 4.14 (2.50–7.07, p < .001) | 4.16 (2.42–7.36, p < .001) |
| Pneumonia | Yes | 337 (81.6) | 76 (18.4) | 13.46 (4.93–55.44, p < .001) | 8.48 (3.02–35.45, p < .001) |
- Note: Multivariable analyses were conducted using logistic regression models utilizing the simultaneous method. The models were adjusted for ferritin levels, gender, hypertension, and pneumonia. Percents are row percentages.
- Abbreviations: aOR, adjusted odds ratio; aP-value, adjusted p-value; CI, confidence interval.
A Cox proportional hazards analysis was conducted to determine whether ferritin had a significant effect on the hazard of mortality (Table 6). The findings (LL = 9.85, df = 1, p = .002) show that ferritin was able to adequately predict the hazard of mortality. It is evident that at any particular time, patients with ferritin levels ≤ 1000 had a hazard that was 0.49 times as large as that of patients with ferritin levels > 1000 (B = −0.72, SE = 0.23, HR = 0.49, p = .001).
| Variable | B | SE | 95% CI | z | p | HR |
|---|---|---|---|---|---|---|
| Ferritin Less than or equal 1000 | −0.72 | 0.23 | [−1.17, −0.28] | −3.18 | .001 | 0.49 |
A Kaplan–Meier survival probability plot was also included for ferritin. The plot represents the survival probabilities for different groups over time and shows that in the initial and later periods, the cumulative probability of dying was higher among patients with ferritin levels > 1000, but in the middle period, little difference was observed in the mortality rate of patients in the different ferritin groups (Figure 1).
4 DISСUSSIОN
The main finding of our study is that the higher mortality rate among patients having ferritin levels > 1000. Other than ferritin levels gender, hypertension and pneumonia were found to be a predictor of in-hospital mortality. Around 89% of the patients having ferritin levels > 1000 had pneumonia and 51% had hypertension. The mean age of the patients was 54.0 ± 15.3 years and among which the ratio of male to female was 233:362. A male predominance was noted in the group with ferritin levels > 1000. Higher levels of C-Reactive Protein and Procalcitonin were seen in ferritin > 1000.
Serum ferritin was found to be an independent predictor of severe SARS-CoV-2 disease.10 A study from Indonesia Rasyid et al. documented a mean ferritin level of 1689 in critically ill SARS-CoV-2-infected patients.11 SARS-CoV-2 patients with cytokine storm were also found to have significantly higher levels of ferritin.12 Several autopsies of SARS-CoV-2 patients revealed higher ferritin levels.13 Elderly SARS-CoV-2 patients with elevated ferritin levels showed higher mortality than those with lower ferritin values.11 In another study, the incidence of ARDS was higher in those with hyperferritinemia.14 Zhou et al. also reported increased mortality in SARS-CoV-2 patients with higher levels of serum ferritin.15 Elevated ferritin levels can be used as a biomarker to stratify high-risk patients from low-risk patients, which may in turn help in the early identification and management of SARS-CoV-2 patients.16 Hyperferritinemia was more common in critically ill and discharged SARS-CoV-2 patients than in stable hospitalized patients.17
Unlike our study, hypertensive SARS-CoV-2 patients had lower levels of serum ferritin, as reported by Huang et al.18 Similar to our study, a study by Phipps et al.19 showed that the severity of acute liver failure in SARS-CoV-2 patients was more common in patients with hyperferritinemia. The frequency of ICU admission was higher in SARS-CoV-2 patients with hyperferritinemia.20 Similar findings were also reported in our study. In another study, SARS-CoV-2 patients with cancer had higher serum ferritin levels than those without cancer.21 The clinical association of hyperferritinemia in SARS-CoV-2 in terms of mortality, comorbidities, and severity was well established in a meta-analysis.22
5 LIMITATIONS
Our study has various limitations. Its retrospective design limits causal inference. Unmeasured confounding factors, such as clinical comorbidities and medications, could have affected the outcomes. This Kuwaiti study included all SARS-CoV-2-positive patients and undoubtedly consisted of mainly milder cases of the disease. However, if it included SARS-CoV-2 patients who typically consist of a significant case mix of mechanically ventilated and critical cases of patients, the findings might have looked different.
6 CОNСLUSIОNS
This study demonstrated that hyperferritinemia is an independent predictor of in-hоsрitаl mоrtаlity in SARS-CoV-2 patients. The incidence of ICU admission was higher with hyperferritinemia. More prospective studies are required to better understand hyperferritinemia and in-hospital mortality in SARS-CoV-2.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Moudhi Alroomi designed the study. Moudhi Alroomi and Rajesh Rajan раrtiсiраted in аnаlysis аnd mаnusсriрt рreраrаtiоn. Ahmad Alsaber, Jiazhu Pan, and Mina Fatemi performed the stаtistiсаl аnаlysis and reviewed the mаnusсriрt. Аll аuthоrs hаd ассess tо the dаtа аnd tаke resроnsibility fоr its integrity аnd the ассurасy оf the dаtа аnаlysis. Аll аuthоrs hаve reаd аnd аррrоved the mаnusсriрt.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the results of the study are available on request from the corresponding author.




