The Next Frontier in Lung Transplantation: Protecting the Endothelium and Repairing Organs for Transplant Utilizing MG53
Lung transplantation is plagued by limited access to suitable donor organs. While organs traditionally come from brain dead donors (BDD), these organs from a standard donor do not currently meet the demand of those on the wait list.1 In recent years, extended criteria donors (ECD) (i.e., donors that were traditionally thought to be of poorer quality) have been utilized with increasing rates and success.2 However, limitations still exist on the immediate function and long-term implications of their use.3 ECD, due to their baseline quality, often suffer a disproportionate amount of warm ischemia during the agonal phase of the organ recovery process. Upon their implantation, the reperfusion injury afflicting these allografts triggers a litany of harmful processes (necroptosis, pyroptosis, etc.) that are the cause of immediate poor allograft function and possibly lead to long-term consequences. This process is known as ischemia reperfusion injury (IRI), and all transplanted organs suffer a degree of this injury. At the cellular level, IRI leads to degradation of the pulmonary vascular endothelium, which allows for an influx of immune cells into the alveoli leading to further damage and pulmonary edema.4 Clinically, the consequence of this inflammatory cascade results in primary graft dysfunction (PGD) within the first 72 h post-transplant, which has deleterious consequences in the immediate post-operative period5, 6 and can lead to long term rejection.5-7
PGD, like any form of acute lung injury (ALI) directly results in endothelial alteration.8 At the site of gas exchange, the alveolo-endothelial membrane consists of a thin layer of pulmonary vascular endothelial cells and alveolar epithelial cells with their basement membranes fused together.9 In addition to facilitating the exchange of oxygen, small amounts of fluid also cross this barrier, which is subsequently drained by lymphatics.10 Upon damage of the pulmonary endothelium (i.e. by IRI), the basement membrane is exposed thus initiating a phenotypic shift from an anti-thrombotic/anti-inflammatory state to a dysfunctional disposition resulting in un-inhibited inflammation leading to destruction of lung parenchyma and eventual pulmonary failure.11
Several pro-inflammatory pathways are initiated that destroy the endothelium, in addition to the recruitment of the innate immune system that causes additional damage. Molecularly, IRI (through the creation of damage-associated molecular patterns [DAMPs]) bind to toll-like receptors which leads to nuclear factor-kappa beta (NF-κB). Once NF-κB translocates into the nucleus, activation of nucleotide-binding oligomerization domain, Leucine rich Repeat and Pyrin domain containgin (NLRP) leads to the creation of reactive-oxygen species (ROS) and the NLRP-inflammasome, which all lead to the cleavage of pro-caspase-1 into its active form—caspase-1. From there, caspase-1 cleaves pro-interleukin-1-beta (IL-1β) to IL-1β, which leads to further inflammation and gasdermin-D (GSDMD) into its split product which initiates pyroptosis.12 Additionally, DAMPs can initiate release of tumor necrosis factor-alpha (TNF-α), which when bound to its receptors recruits cytosolic adaptor proteins to form complex I (which contains RIPK1) and complex II. This ultimately leads to the activation of mixed lineage kinase domain-like protein (MLKL) to promote its oligomerization and form a nonspecific membrane pore, which disrupts homeostasis cytosolic ions and the execution of necroptosis.13 Together, the activation of cell-programmed pathways of death leads to further destruction of the endothelial barrier and loss of its function. In terms of an innate immune response, neutrophil recruitment (and infiltration) are hallmarks of endothelial injury. Specific to lung transplantation, donor-derived non-classical monocytes (NCMs) are retained within the pulmonary vasculature which upon reperfusion into the recipient generate high levels of the neutrophil chemokine CXCL2, which recruits recipient neutrophils to the exposed basement membrane.4 These neutrophils subsequently migrate into the alveoli (to clear dead cells), however, due to their short half-life, death of neutrophils trigger secondary inflammation, which cause further damage and pulmonary edema and are the main leukocyte that is associated with injury in the acute phase.4
While there are many avenues to confer protection against IRI in the immediate post-operative period—direct preservation of pulmonary endothelium might be the most substantial in preserving allograft function and improving patient outcomes. Mitsugumin 53 (MG53) is a tripartite motif-containing (TRIM) family protein that is intimately involved in cell membrane repair. Once a membrane is injured, the cytosol is exposed to the oxidized extracellular environment which is sensed by MG53. MG53 is subsequently oligomerized through oxidation-dependent processes and formats a repair complex via tethering of phosphatidylserine on intracellular vesicles and the inner leaflet of the plasma membrane. Finally, local elevation of calcium ions allows of fusion of the aforementioned vesicles with the plasma membrane to form the repair patch (i.e., a “plug and patch” technique).14 While discovered initially in striated muscle, MG53 has been found to be also predominately expressed by alveolar epithelial cells.15 Modulation or administration of an exogenously produced human recombinant MG53 (rhMG53) and its related cell membrane repair is a potential novel therapeutic for the preservation of the pulmonary epithelium and endothelium for the treatment of IRI and prevention of PGD associated with lung transplantation.
First described by Jia et al., rhMG53 administration during rodent models of acute lung injury (ALI) resulted in preserved tissue architecture and pulmonic function. Additionally, serum marker of inflammation interleukin-6 (IL-6) and IL-1β were seen to be significantly decreased after administration as well. Rapid amplification of cDNA ends revealed that endogenous MG53 is produced by alveolar epithelial cells as well.15 While this study demonstrated the MG53 is protective against over-ventilation induced ALI, and is generated by alveolar epithelial cells as well, it was unclear if rhMG53 administration resulted in all membranes being repaired, or if individual cell populations were being targeted. In additional pre-clinical models of transplant relevant IRI, it was found that rhMG53 co-localized with CD31, which is a transmembrane protein that is almost exclusively expressed on endothelial cells.16 This observation indicates that the exogenously supplemented rhMG53 protein is locally bioavailable in the lung tissue and specifically associates with the damaged endothelium.12 While this finding is complementary to MG53's known membrane repair functions, other researchers have sought to determine if they're additional functions of MG53.
In studies examining MG53's role in protecting the liver against IRI, Han et al. found that MG53 was incorporated intracellularly in addition to its known membrane site of action, therefore indicating possible additional benefits of MG53.17 Wang et al. investigated a therapeutic role of MG53 to inhibit necroptosis during cardiac IRI. They found that MG53 could act as an E3-ligase by adding multiple ubiquitin chains to RIPK1, mediate its degradation and thus mitigate necroptosis within injured cells.13 While its necroptotic functions have been described, MG53's role in pyroptosis is being elucidated. Gouchoe et al. found that exogenous administration of rhMG53 lead to mitigated release of IL-1β and GSDMD, indicating a possible interaction of that pathway with MG53. While decreasing inflammatory pathways is important for the preservation of the endothelium, the innate immune system also plays a key role in destruction. Neutrophils are the main culprit of this injury early in the pathogenesis of IRI. Again, Gouchoe et al. found that the innate immune response is altered with the administration of rhMG53, leading to dampened neutrophilic response.12
Ultimately, the endothelium serves a multitude of functions; however an additional function is to regulate vascular tone through a variety of factors, most notably nitric oxide and endothelin-1 (ET-1).18 ET-1 is a vasoconstrictor and has been shown to mediate ALI as well.19 Particularly important to lung transplantation, high levels of ET-1 in the immediate post-operative period following lung transplantation has been associated with PGD20, 21 and long-term allograft dysfunction.22 At the cellular level, endothelial injury leads to ET-1 release and through endothelial-epithelial interaction decreases alveolar fluid reabsorption leading to edema formation within the alveolar space.23 Again, MG53 has shown the ability to decrease ET-1 release, and thus decrease formation of pulmonary edema.12 However, the exact mechanisms behind this release are yet to be elucidated and warrant further study.
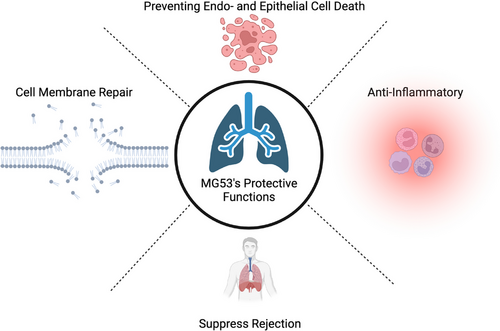
It is clear that MG53 is multi-functioning protein that not only is involved in direct membrane repair but is also mitigates the inflammatory response in common pathways associated with IRI and possibly has a role in innate immune modulation (Figure 1). The diverse set of functions makes MG53 an ideal therapeutic to combat IRI and further protect the most important barrier within the lung. As the lung transplantation waiting list is associated with a mortality that approaches 20% per year,1 it is important to transplant these patients as quickly as possible. The use of ECD allografts can lead to faster transplantation24; however it is not without its risks as these allografts are associated with decreased mid-term survival.3 MG53 offers the ability to repair the endothelium, preserve its function and by doing so maintains adequate oxygen exchange and parenchymal structure within lungs. By repairing ECD allografts, the donor pool for lung transplantation will be safely expanded, and thus further the potential for this life altering procedure.
CONFLICT OF INTEREST STATEMENT
All authors have no conflict of interest to declare.




