Trend analysis of noncommunicable diseases and their risk factors in Afghanistan
Edited by Yi Cui
Abstract
Background
Afghanistan is suffering from 40-year chronic conflicts, displacement, and demolition of its infrastructure. Afghanistan mortality survey 2010 shows nearly 46% of all deaths in the country were attributed to noncommunicable diseases (NCDs). In this study, we aimed to understand the differences in mortality and premature death due to NCDs by sex and the trend for the next 8 years.
Methods
We applied trend analysis using the secondary data from the Institute for Health Metrics and Evaluation, Global Burden of Diseases 2019. The information on NCD mortality, NCD deaths attributed to its risk factors, NCD percent of total years lived with disability (YLDs) attribution to each risk factor extracted from this database from 2008 to 2019. We investigated the trend from 2008 to 2019 for the mentioned factors and then forecast their trends until 2030.
Results
Our study shows that Afghanistan has had an increasing death number due to NCDs from 2008 to 2019 (50% for both sexes) and this will reach nearly 54% by 2030. Currently, half of NCDs deaths are premature in Afghanistan. The mortality rate and prevalence of risk factors are higher among women. More than 70% of YLDs will be due to NCDs in Afghanistan till 2030. Five risk factors including high systolic blood pressure (28.3%), high body mass index (23.4%), high blood glucose (20.6%), high low-density lipoprotein cholesterol (16.3%), and smoking (12.3%) will have the highest contribution to NCDs death in 2030, respectively.
Conclusions
In general, our study indicates that without any specific intervention to address NCDs in Afghanistan, not only the Sustainable Development Goal target for NCDs will not be met, but an increase in almost all risk factors prevalence, as well as NCD mortality, will be seen in Afghanistan.
Highlights
-
The noncommunicable diseases (NCDs) mortality rate and its attribution to their common risk factors will increase till 2030 in Afghanistan and this increase will be more prevalent among women.
-
Specific and context-based policies and interventions should be designed to control and prevent high blood pressure, high body mass index, high blood glucose, high low-density lipoprotein cholesterol, and smoking among the population in Afghanistan.
-
Integrating NCDs prevention and control in the primary healthcare system is recommended.
1 INTRODUCTION
The four main noncommunicable diseases (NCDs) are cardiovascular diseases, cancer, chronic respiratory disease, and diabetes. NCDs and their common risk factors were the cause of 74.3% of deaths globally in 2019.1 These account for 82% of NCD deaths (32 million) occurring in low- and middle-income countries. In the countries of the WHO region for the Eastern Mediterranean, up to 50% of deaths due to NCDs occur before the age of 60 years compared with less than 10% in Western Europe.2 Afghanistan mortality survey 2010 shows that nearly 46% of all deaths in the country were attributed to NCDs including injuries.3 It means every two persons in Afghanistan dies due to NCDs.
Common, preventable risk factors underlie most NCDs. Globally, the leading risk factors are raised blood pressure, followed by tobacco use. Other major risk factors, accounting for a large fraction of the global mortality and morbidity from NCDs include alcohol use, unhealthy diet (such as low fruit and vegetable intake, or high salt intake), insufficient physical activity, overweight/obesity, raised blood glucose, and raised cholesterol.4
Afghanistan is suffering from 40-year chronic conflicts, displacement, and demolition of its infrastructure. Afghanistan is classified as a low-income country in which the health indicators have the worst situation after some African countries, such as Sierra Leone, Central African Republic, Chad, Guinea-Bissau, and Nigeria.5 This country was positioned 169 out of 188 in the low development category.6 Considerable progress has been made in improving health indicators; however, the collapse of government on August 15, 2021, and the pausing of donor's fund put at risk the gains made over two decades.7 Wide vulnerability including high poverty levels, food insecurity, limited access to drinking water and sanitation facilities, and natural disasters such as earthquakes and drought cause the health situation to worsen in the current situation, especially among women.8 These factors especially are prevalent among the most disadvantaged poor and least educated families living in rural settings.9 Besides, there is extreme inequality in terms of women's access to healthcare; Afghanistan is ranked 157 out of 162 countries in the 2019 Gender Inequality Index (GII value of 0.655).10
The increasing burden of NCDs also imposes severe economic consequences that range from the impoverishment of families to high health system costs and the weakening of country economies. The NCD epidemic is thwarting poverty reduction efforts and robbing societies of funds that could otherwise be devoted to social and economic development.11 NCDs-related health services' delivery is still limited in Afghanistan. The public sector lacks institutions with technical expertise for major NCDs. In this context, the private sector (none for profit and for-profit providers and contractors) is the prominent source of outpatient services. The for-profit sector provides mainly curative care. The national NCDs surveillance system, which is crucial for informed policy and strategy, has not been established yet. The mechanism for death registration and the qualification of the cause of death information does not exist. Almost no fund-raising activities have been carried out to support NCD-related activities in the country and the severe shortage of medical specialists is problematic for all NCDs as many qualified professionals left the country during the conflict years.12
To prevent the worsening of the current existing poverty within the country and mitigate the disaster effects on the Afghan population, there is a need to develop proper and context-based strategies to control and prevent NCDs. To set the strategies and determine which risk factors should focus more, a trend analysis is required. In this study, we aimed to understand (i) the difference in mortality and premature death due to NCDs by sex, (ii) the trend for the next 8 years, and (iii) the significance of each risk factor in terms of NCD mortality and years lived with disability (YLDs) attribution. The evidence provided in this paper on the trend of NCDs mortality and attribution of NCDs mortality and YLDs to the risk factors in Afghanistan will highlight the significance of each risk factor and will help policymakers to develop applicable and cost-effective strategies based on the significance of each risk factor. Obviously, data on the prevalence of NCDs risk factors and their trends are needed to commonly be used for public and policy communication.13 Finally based on this analysis, we propose a practical set of priority national targets in keeping with the globally agreed set of targets.
2 METHODS
In this study, we analyzed the trend of NCD deaths attributed to seven risk factors including smoking, physical activity, body mass index, alcohol use, blood pressure, blood glucose, blood cholesterol, and YLD attributed to the same risk factors mentioned above, by gender from the year 2008 to 2019. The data for these indicators are shown in Table 1.
| Investigated factors | Factors/years | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NCD deaths | Total NCD deaths (%) | Male—Afghanistan | 45.00 | 45.62 | 45.81 | 46.11 | 45.87 | 46.28 | 45.17 | 44.21 | 43.78 | 46.33 | 46.88 | 48.14 |
| Females—Afghanistan | 52.00 | 52.48 | 53.18 | 53.89 | 54.39 | 55.40 | 55.31 | 55.25 | 55.53 | 57.74 | 54.99 | 56.70 | ||
| Male—World | 64.62 | 65.67 | 66.14 | 67.13 | 67.84 | 68.56 | 69.17 | 69.96 | 70.75 | 71.46 | 72.26 | 73.01 | ||
| Female—World | 67.22 | 68.25 | 68.76 | 69.75 | 70.61 | 71.36 | 72.10 | 72.89 | 73.73 | 74.47 | 75.25 | 75.98 | ||
| NCD deaths under age 70 (%) | Male—Afghanistan | 36.00 | 36.63 | 36.82 | 37.12 | 36.95 | 37.48 | 36.44 | 35.49 | 35.17 | 37.72 | 39.34 | 45.00 | |
| Females—Afghanistan | 43.00 | 44.18 | 44.81 | 45.47 | 45.94 | 47.00 | 46.83 | 46.72 | 47.05 | 49.39 | 47.70 | 55.00 | ||
| Male—World | 51.20 | 52.27 | 52.70 | 53.91 | 54.73 | 55.47 | 56.19 | 57.28 | 58.29 | 59.06 | 59.99 | 60.79 | ||
| Female—World | 47.84 | 48.96 | 49.51 | 50.86 | 52.04 | 53.17 | 54.36 | 55.70 | 57.01 | 58.13 | 59.26 | 60.25 | ||
| Smoking | NCD deaths attributable to smoking (%) | Male | 12.18 | 12.74 | 13.27 | 13.84 | 14.44 | 15.03 | 15.59 | 16.08 | 16.46 | 16.76 | 16.98 | 17.06 |
| Female | 2.17 | 2.24 | 2.30 | 2.38 | 2.47 | 2.56 | 2.66 | 2.75 | 2.82 | 2.87 | 2.88 | 2.87 | ||
| Both sex | 6.31 | 6.64 | 6.94 | 7.27 | 7.63 | 7.95 | 8.26 | 8.55 | 8.75 | 8.90 | 9.00 | 9.04 | ||
| NCD % of total YLDs (15–49 ages) attributable to smoking | Male | 1.83 | 1.91 | 1.99 | 2.07 | 2.16 | 2.24 | 2.33 | 2.40 | 2.45 | 2.48 | 2.50 | 2.52 | |
| Female | 0.20 | 0.23 | 0.24 | 0.25 | 0.26 | 0.27 | 0.28 | 0.29 | 0.29 | 0.29 | 0.29 | 0.29 | ||
| Both sex | 0.86 | 0.91 | 0.94 | 0.98 | 1.03 | 1.07 | 1.11 | 1.14 | 1.16 | 1.17 | 1.18 | 1.19 | ||
| Physical activity | NCD deaths attributable to low physical activity (%) | Male | 2.84 | 2.87 | 2.88 | 2.89 | 2.91 | 2.90 | 2.91 | 2.95 | 2.95 | 2.98 | 3.01 | 3.03 |
| Female | 2.81 | 2.89 | 2.91 | 2.95 | 2.98 | 3.00 | 3.02 | 3.00 | 3.40 | 3.15 | 3.19 | 3.21 | ||
| Both sex | 2.83 | 2.88 | 2.89 | 2.92 | 2.95 | 2.95 | 2.98 | 3.02 | 3.04 | 3.07 | 3.11 | 3.13 | ||
| NCD % of total YLDs attributable to low physical activity | Male | 0.50 | 0.50 | 0.51 | 0.51 | 0.52 | 0.52 | 0.54 | 0.55 | 0.56 | 0.57 | 0.58 | 0.59 | |
| Female | 0.48 | 0.49 | 0.50 | 0.51 | 0.51 | 0.52 | 0.53 | 0.54 | 0.55 | 0.56 | 0.57 | 0.58 | ||
| Both sex | 0.49 | 0.50 | 0.50 | 0.51 | 0.51 | 0.52 | 0.53 | 0.54 | 0.55 | 0.56 | 0.57 | 0.58 | ||
| High body mass index | NCD deaths attributable to high body mass index (%) | Male | 7.34 | 8.12 | 8.70 | 9.27 | 9.86 | 10.36 | 10.90 | 11.44 | 11.89 | 12.32 | 12.77 | 13.13 |
| Female | 13.27 | 14.12 | 14.80 | 15.52 | 16.25 | 16.68 | 17.51 | 18.14 | 18.67 | 19.12 | 19.54 | 19.82 | ||
| Both sex | 10.46 | 11.25 | 11.90 | 12.55 | 13.23 | 13.80 | 14.41 | 15.01 | 15.51 | 15.95 | 16.40 | 16.72 | ||
| NCD % of total YLDs attributable to high body mass index | Male | 2.01 | 2.19 | 2.35 | 2.51 | 2.68 | 2.86 | 3.05 | 3.23 | 3.37 | 3.51 | 3.65 | 3.79 | |
| Female | 3.30 | 3.52 | 3.71 | 3.89 | 4.08 | 4.26 | 4.45 | 4.60 | 4.70 | 4.79 | 4.90 | 5.01 | ||
| Both sex | 2.75 | 2.96 | 3.13 | 3.30 | 3.49 | 3.67 | 3.86 | 4.02 | 4.14 | 4.25 | 4.37 | 4.50 | ||
| Alcohol use | NCD deaths attributable to alcohol use % | Male | 0.42 | 0.43 | 0.43 | 0.44 | 0.45 | 0.45 | 0.46 | 0.46 | 0.48 | 0.49 | 0.50 | 0.51 |
| Female | 0.27 | 0.26 | 0.26 | 0.25 | 0.25 | 0.25 | 0.24 | 0.24 | 0.24 | 0.25 | 0.25 | 0.25 | ||
| Both sex | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | 0.30 | ||
| NCD % of total YLDs attributable to alcohol use | Male | 0.84 | 0.84 | 0.85 | 0.85 | 0.86 | 0.86 | 0.86 | 0.86 | 0.86 | 0.86 | 0.86 | 0.86 | |
| Female | 0.27 | 0.27 | 0.27 | 0.27 | 0.28 | 0.27 | 0.27 | 0.27 | 0.28 | 0.28 | 0.28 | 0.29 | ||
| Both sex | 0.51 | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 | 0.53 | 0.53 | ||
| High systolic blood pressure | NCD deaths attributable to high systolic blood pressure % | Male | 25 | 25 | 25 | 25 | 25 | 25 | 26 | 26 | 26 | 26 | 26 | 26 |
| Female | 27 | 27 | 27 | 27 | 27 | 27 | 27 | 27 | 28 | 28 | 28 | 28 | ||
| Both sex | 26 | 26 | 26 | 26 | 26 | 26 | 26 | 27 | 27 | 27 | 27 | 27 | ||
| NCD % of total YLDs attributable to high systolic blood pressure | Male | 1.63 | 1.62 | 1.61 | 1.62 | 1.63 | 1.64 | 1.66 | 1.69 | 1.70 | 1.71 | 1.73 | 1.75 | |
| Female | 1.60 | 1.58 | 1.57 | 1.57 | 1.58 | 1.59 | 1.61 | 1.62 | 1.60 | 1.59 | 1.59 | 1.59 | ||
| Both sex | 1.61 | 1.60 | 1.59 | 1.59 | 1.60 | 1.61 | 1.83 | 1.65 | 1.64 | 1.64 | 1.65 | 1.66 | ||
| High blood glucose | NCD deaths attributable to high blood glucose % | Male | 14.85 | 15.14 | 15.21 | 15.32 | 15.42 | 15.40 | 15.49 | 15.63 | 15.74 | 15.89 | 16.13 | 16.31 |
| Female | 17.98 | 18.19 | 18.23 | 18.42 | 19.00 | 19.00 | 19.00 | 19.00 | 20.00 | 20.00 | 20.00 | 21.00 | ||
| Both sex | 16.47 | 16.72 | 16.78 | 16.94 | 17.11 | 17.18 | 17.37 | 17.61 | 17.83 | 18.04 | 18.34 | 18.86 | ||
| NCD % of total YLDs attributable to high blood glucose | Male | 4.53 | 4.58 | 4.60 | 4.65 | 4.70 | 4.77 | 4.86 | 4.97 | 5.06 | 5.17 | 5.29 | 5.42 | |
| Female | 4.69 | 4.75 | 4.79 | 4.85 | 4.92 | 4.99 | 5.08 | 5.16 | 5.21 | 5.26 | 5.35 | 5.45 | ||
| Both sex | 4.62 | 4.68 | 4.71 | 4.76 | 4.83 | 4.90 | 4.99 | 5.08 | 5.15 | 5.22 | 5.32 | 5.44 | ||
| High LDL cholesterol | NCD deaths attributable to high LDL cholesterol % | Male | 13.85 | 14.01 | 14.07 | 14.22 | 14.41 | 14.45 | 14.61 | 14.93 | 15.10 | 15.39 | 15.74 | 15.99 |
| Female | 13.11 | 13.19 | 13.20 | 13.28 | 13.36 | 13.32 | 13.37 | 13.56 | 13.65 | 13.83 | 14.01 | 14.12 | ||
| Both sex | 13.45 | 13.57 | 13.60 | 13.72 | 13.85 | 13.85 | 13.94 | 14.19 | 14.32 | 14.55 | 14.81 | 14.98 | ||
| NCD % of total YLDs attributable to high LDL cholesterol | Male | 0.58 | 0.58 | 0.58 | 0.58 | 0.59 | 0.59 | 0.60 | 0.61 | 0.62 | 0.62 | 0.63 | 0.64 | |
| Female | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 | 0.53 | 0.53 | 0.53 | 0.53 | 0.54 | 0.54 | 0.54 | ||
| Both sex | 0.54 | 0.55 | 0.55 | 0.55 | 0.55 | 0.55 | 0.56 | 0.57 | 0.57 | 0.57 | 0.58 | 0.59 | ||
- Abbreviations: GBD, Global Burden of Diseases; LDL, low-density lipoprotein; NCDs, noncommunicable diseases; YLDs, years lived with disability.
- Source: Institute for Health Metrics and Evaluation, GBD 2019.
As shown in the table, measurements for the study factors repeated over time and annually. In addition to descriptive analyses to show the trend of death rates and its NCD causes over time in Afghanistan, we also tried to predict how the trend will be continued over the years by 2030.
Due to the lack of death registration and NCDs surveillance system in Afghanistan, we used the secondary data collected by visiting the Global Burden of Diseases (GBD) website, which is owned by the Institute for Health Metrics and Evaluation (IHME), and the independent global health research center at the University of Washington. The GBD data, which was our data source in this study, are publicly available for noncommercial use (GBD; Available at: www.healthdata.org/gbd. Accessed date: 11/10/2020). Despite the availability of the required data for this study in a number of databases other than the GBD, including the WHO, this database was selected intentionally as it provides the most up-to-date data by country and age groups, gender, and some other characteristics. The GBD 2019 collaborators identify multiple relevant data sources for each disease, injury, and risk factors, including censuses, civil registration and vital statistics, household surveys, disease registries, air pollution monitors, health service use, disease notification, and other sources. Then, they produce unified, comparable data for different countries using special modeling and data processing methods.14, 15 Also, the report of NCDs death by the type of NCDs in the GBD website is based on the ICD-10 format, which makes the comparability of the results with other countries and the world most possible.
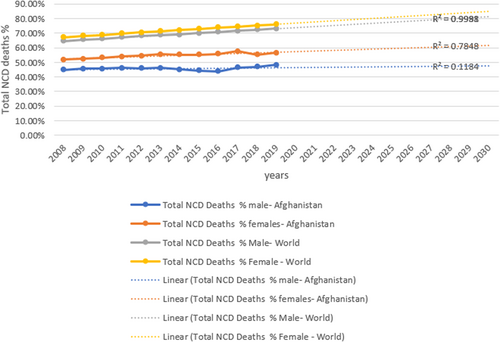
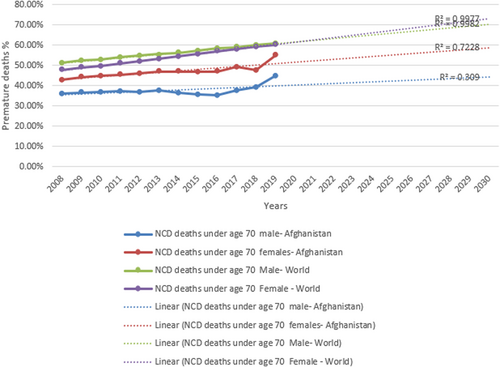
Given the necessity of considering the time factors in all analyses, linear regression analysis was used to describe or explain the trends in causes of death based on time. In fact, this analysis was used to measure the slope of changes in mortality rates and the YLDs, where “time” is the independent variable and “percentage of causes of death” and “number of years lived with disability” are the dependent variables. Excel software was used to investigate the trend from 2008 to 2019 for the mentioned factors and then forecast their trends until 2030. The prediction helps us to set up realistic goals and objectives for the Afghanistan national NCDs management policy. The graphs show the trend while we compared the mortality trend for males and females in Afghanistan and the world (Figures 1 and 2). We also showed the trend for NCDs and YLDs attributions to risk factors (Supporting Information file).
3 RESULT
3.1 NCD mortality and premature death trend in Afghanistan and the world
As Figure 1 shows, Afghanistan has had an increasing death number due to NCDs from 2008 till 2019 (more than 55% for females and more than 45% for males in 2019). This means that one out of every two Afghans dies due to NCDs in Afghanistan. Although the graph shows a decline in the number of deaths for men in 2016 and for females in 2018, as predicted, these numbers will have an increment trend and will go beyond 60.0% for females and to 47.6% for males by 2030. However, Afghanistan's rate is lower compared with the World rate (more than 70% for both sexes in 2019, and more than 80% in 2030). The mortality rate is higher among women than men in Afghanistan.
Figure 2 also shows an increasing trend in premature NCD deaths in Afghanistan for males and females. However, this trend is lower for Afghanistan compared with the world's NCD premature deaths. In addition, the NCD deaths under age 70 are more prevalent among females compared with men in this country. On the basis of the data, currently, half of NCDs' death are premature in Afghanistan. The graph also shows that nearly 60% of NCD deaths in women and more than 40% of NCD deaths in males will be premature in 2030.
3.2 Trend of attribution of NCD deaths and YLD to risk factors
As Figure S3 shows more than 70% of YLDs will be due to NCDs in Afghanistan until 2030. The graph illustrates an increasing trend for NCDs deaths attributed to smoking as well as for attribution of YLD to smoking in Afghanistan. Our prediction shows that 12.29% of NCDs deaths and 1.58% of YLDs will be attributed to smoking in Afghanistan. Although the attribution of NCDs death and YLDs to low physical activity does not have considerable change from 2008 to 2030, it will attribute to 3.41% NCDs death and 0.67% of YLDs in 2030 (Figure S4). The NCDs percentage of total YLDs will have an increasing trend toward 2030, with a similar trend for total YLDs' attribution to high body mass index (from 2.75% in 2008 to 6.34% in 2030). The figure also shows an increasing attribution of total NCDs deaths to high body mass index (from 10.46% in 2008 to 23.41% in 2030), more than twofold in Afghanistan (Figure S5). NCDs deaths and YLDs have a consistent attribution to alcohol use in Afghanistan from 2008 to 2030 with no significant change (Figure S6)
Although our finding shows a low growth rate for attribution of NCD deaths and YLDs to high systolic blood pressure from 2019 until 2030 (to near 30% for NCD deaths and 1.75% for YLDs), still the data shows that one in every three persons die/will die due to high systolic blood pressure during this time (Figure S7). Our finding also shows an increasing trend in the attribution of NCD deaths to high blood glucose (from 16.47% in 2008 to 20.66% in 2030) and YLDs (from 4.62% in 2008 to 6.19% in 2030). It means that one in every five persons dies/will die due to having high blood glucose in Afghanistan (Figure S8).
The trend of NCD deaths and YLDs attribution to high low-density lipoprotein (LDL) cholesterol also is additive from 2008 to 2030 (from 13.45% in 2008 to 16.30% in 2030 for NCD deaths); however, this increment is very low for YLDs attribution to high LDL cholesterol (to less than 1% in 2030) (Figure S9).
As Table 2 shows NCDs death will have the highest attribution to the five risk factors, including high systolic blood pressure, high body mass index, high blood glucose, high LDL cholesterol, and smoking in 2030, respectively.
| Risk factor | High systolic blood pressure (%) | High body mass index (%) | High blood glucose (%) | High LDL cholesterol (%) | Smoking (%) | Low physical activity (%) | Alcohol use (%) |
|---|---|---|---|---|---|---|---|
| Attribution to NCDs death | 28.34 | 23.41 | 20.66 | 16.30 | 12.29 | 3.41 | 0.30 |
| Attribution to YLDs | 1.75 | 6.34 | 6.19 | 0.63 | 1.58 | 0.67 | 0.54 |
- Abbreviations: LDL, low-density lipoprotein; NCDs, noncommunicable diseases; YLDs, years lived with disability.
4 DISCUSSION
In this study, we aimed to map the trend of NCDs mortality and the attribution to the risk factors from 2008 to 2019 and forecast their trend into 2030.
People suffering from NCDs mostly develop impairments, which may lead to restriction and activity limitations in the absence of supportive personal and environmental factors. An 80% of YLDs rate is attributed to NCDs.16 It means NCDs can often lead to disabilities. Data from the Global Burden of Disease Study show that 9 out of the top 10 causes of YLD were NCDs.17
NCD countdown 2030 collaborators in 2018 investigated the worldwide trends in NCD mortality and progress toward Sustainable Development Goals (SDGs) target 3.4. They found that mortality from the four NCDs included in SDG target 3.4 become inert or increased since 2010 in 15 countries among women and middle-income countries than in high-income countries.18 Our finding shows that the NCD mortality rate is increasing from 2008 toward 2030 and it is higher among women rather than men in Afghanistan. This means there is inequality in terms of access to healthy food and healthcare for women.
The NCD countdown collaborators also indicated that SDG target 3.4 will be achieved in 35 countries for women and 30 for men if these countries maintain or surpass their 2010–2016 rate of decline in NCD mortality. Most of these are high-income countries with already—low NCD mortality, and countries in Central and Eastern Europe. An additional 50 countries for women and 35 for men are projected to achieve such a reduction in the subsequent decade, and thus, with the slight acceleration of decline, could meet the 2030 target.18 Our data showed that a one-third reduction, relative to 2015 levels of premature NCDs mortality (from 35.49% in 2015 to 23.40% in 2030 for males and from 46.72% in 2015 to 31.40% in 2030 for females) will not be achieved until 2030 having any specific strategies in Afghanistan. Although the 30–70-year mortality rate is lower in Afghanistan compared with the world, this rate is higher among females rather than males in Afghanistan.
NCD-associated risk factors such as tobacco smoking, harmful use of alcohol, unhealthy diet, and physical inactivity substantially affect NCD mortality. Available data shows that 31% of the world's population is not meeting the minimum recommendations for physical activity.19 In Afghanistan, physical inactivity is responsible for 3.13% of NCD deaths and the trend until 2030 will remain the same.
A study estimated trends between 1980 and 2008 in overweight and obesity prevalence and their uncertainty for adults 20 years of age and older in 199 countries and territories. The finding of this study shows that the prevalence of obesity and overweight increased during the 28-year period. They found that, although the magnitude of the rise in obesity varies by region, country, and gender, stability in obesity prevalence was rare. Moreover, the rise in obesity has accelerated in the last decade (2000–2008). This study also mentioned an estimated decline in the prevalence of obesity for men in seven countries, including Afghanistan.13 Our finding also shows that the increase in BMI is more prevalent among women than in men. In addition, the attribution of the total NCD deaths to the BMI is increasing over the period of 2008–2030 in Afghanistan.
The study in Africa shows that the age-standardized prevalence of diabetes increased from 3.4% to 8.5% in men and from 4.1% to 8.9% in women (NCD Risk Factor Collaboration.20 Our result indicates an increase in the attribution of NCD deaths and YLDs to the high blood glucose in Afghanistan from 2008 to 2030 and it is more prevalent among women rather than men.
Our result shows that high systolic blood pressure contributes to NCD deaths and YLDs will increase slightly from 2019 to 2030, but as the study conducted by NCD Risk Factor Collection in 2017 supports our finding, Afghanistan is one of the countries with a high prevalence of mean blood pressure, and one of every three adults dies/will die from high systolic blood pressure in this country.
Another study in Pakistan shows that the tobacco use is more prevalent among men (35.6%) compared with women (8.7%). This study has also found that a high percentage of females in Pakistan have a low level of physical activity (58.6%) compared with men (28.2%) and obesity is more prevalent among women (17.1%) than men (12.1%).21 This study in Pakistan does not show any increase in the investigated NCD risk factors, but its result is like our findings regarding the prevalence of tobacco use (higher in men), physical inactivity, and obesity (more prevalent among women). Our study also shows that NCD deaths and YLDs' attribution to smoking will have an increasing trend over 2019–2030.
Harmful use of alcohol has been estimated to be responsible for 3.3 million deaths globally every year, which represents 5.9% of all deaths.22 The highest alcohol consumption levels are found in the developed world, particularly in the WHO European Region and the Region of the Americas. Our findings indicate no significant changes in the attribution of alcohol use to NCD deaths and YLDs during 2008–2030. There is a legal and social restriction on alcohol use in Afghanistan, so less information is available on the use of alcohol in this country.
A study conducted in 2010 also reports 2.2% raised cholesterol levels in the Indian population residing in Punjab.23 Our study also shows a 3.0% increase in the trend of high LDL cholesterol among both sexes. Our findings indicate that one in every four people will have high LDL cholesterol in Afghanistan by 2030.
Limited data on NCDs in Afghanistan has prevented an accurate assessment of the NCD burden and has created challenges in the development of effective interventions. Afghanistan lacks standardized surveillance systems for NCDs, with a few exceptions. The study which addressed the blood pressure trends worldwide from 1975 to 2015 also emphasized the importance of national NCD-oriented surveillance and the inclusion of older people in health surveys.24 In addition, the health system needs to have surveillance of NCDs and related risk factors, health sector activities such as screening, diagnosis, and management are also important. Healthcare systems in many developing countries are not well prepared to deal with the high burden of NCDs, and there is increased recognition of the need to strengthen primary care services in Afghanistan. One strategy that can be used within a primary care setting in the prevention of NCDs is to assess patients for common risk factors and to provide counseling on behavior modification.25 WHO released the results of STEPwise surveys in Afghanistan in 2015 and 2018;26, 27 however, there are no practical interventions in health policies and strategies of the Ministry of Public Health to address the mortality and morbidity related to NCDs and their common risk factors.
4.1 Setting target for reduction of NCD mortality and its shared risk factors' prevalence for Afghanistan
As indicated, our findings on the trend of NCDs death and risk factors prevalence are aligned with the world's trend. Afghanistan should develop its own NCD targets in line with its international obligations. The global mortality target of a 25% relative reduction in premature mortality from NCDs was based on the achievement of the best-performing countries. The establishment of a national, multisectoral action plan and strategy will provide the context for the achievement of Afghanistan NCDs targets. Table 3 shows the global target for the reduction of NCDs mortality and its shared risk factors and the health system targets for the world. It works as a reference to adjust the targets for Afghanistan. Table 4 also proposes the criteria by which we select the targets for the Afghanistan context.
| Premature mortality reduction from NCDs | 25% relative reduction |
| Harmful use of alcohol | 10% relative reduction |
| Physical inactivity | 10% relative reduction |
| Salt/sodium intake | 30% relative reduction |
| Tobacco use | 30% relative reduction |
| Raised blood pressure | 25% reduction |
| Diabetes and obesity | 0% increase |
| Drug therapy and counseling | 50% coverage |
| Essential medicine and technologies | 80% coverage |
- Abbreviation: NCDs, noncommunicable diseases.
| Importance of risk factor—its contribution to the overall NCD mortality and YLDs |
| Impact of achieving the target on ethnic inequalities in NCD mortality |
| Availability of cost-effective and affordable interventions |
| Successful national and international experiences |
| Ability to measure progress in a timely manner |
| Political feasibility of the target |
| Programmatic feasibility of the target |
- Abbreviations: NCDs, noncommunicable diseases; YLD, years lived with disability.
Political feasibility is challenging in Afghanistan because while this can change quite rapidly—the most important actions such as taxation and regulating market/ing—currently need high political stability and the will of the de facto authorities. Programmatic feasibility hinges not only on high-level political support, sufficient to make available the required financial resources but also people and organizational capacity and capability to implement interventions, wider societal support, effective partnerships with a range of sectors, ongoing monitoring of performance indicators, together with strategic oversight and technical guidance. Currently, due to unstable and unpredictable situations, and unauthorized government by international society, the prerequisite of programmatic feasibility is hardly available within Afghanistan.
We did not use the WHO target for setting the target for Afghanistan, because we considered it unrealistic that it will not be met, given the absence of strong governance, lack of financial resources in the country, and the lack of international donors after changing the regime. In addition to setting the targets for Afghanistan, we also extend the time for achieving the target from 2025 to 2030 for this country. It gives more time to involve stakeholders to achieve the targets in a timely manner (Table 5).
| Factor | AFG target by 2030 | WHO target by 2025 | Justification | Action |
|---|---|---|---|---|
| Raised blood pressure | A 25% relative reduction in the prevalence of raised blood pressure | A 25% relative reduction in the prevalence of raised blood pressure by 2025 | The essential health services to control and monitor high blood pressure are included in the Basic Package of Health Services (BPHS) which is implemented by NGOs in 34 provinces of Afghanistan, so by implementing this package properly, this target is achievable in Afghanistan | Proper financing, implementation, and M&E of interventions related to screening, controlling, and treatment of blood pressure in BPHS |
| Obesity | A 0% increase | A 0% increase | High body mass index is the second factor with a high contribution to NCDs death and YLDs in Afghanistan | Improved physical activity levels in children and adults are important but will make only a small contribution to achieving the obesity target. The focus must be primarily on food and nutrition |
| Saturated fat intake | A 25% relative reduction in energy intake from saturated fat for adults | Not included as a WHO target | There is no national assessment to determine the current situation of saturated fat intake in Afghanistan. So, primarily, we recommend conducting a baseline assessment and then set the actions for a relative 25% reduction in Afghanistan | Developing a strategic approach to saturated fat reduction, including a public educational campaign to inform the public about the low-fat diets |
| Salt/sodium intake | A 30% relative reduction in mean population intake of salt/sodium | A 30% relative reduction in mean population intake of salt/sodium | The level of salt intake is 12.1 g/day for both sexes,28 which is more than twofold of the recommended intake of salt by WHO. A 30% reduction will mean that the salt consumed per person per day in Afghanistan would fall from 12.1 to 8.5 g; however, it is still higher than WHO recommendations (5 g/day/person). Achieving this target will have a major impact on population blood pressure levels, heart disease, and stroke rates | Development of a national salt reduction strategic plan, including initiating a consumer awareness campaign and undertaking independent monitoring of progress at 3–5-year intervals |
| Tobacco use | A 25% relative reduction in tobacco use prevalence in 2021 which is 44.2%29 | A 30% relative reduction in the prevalence of current tobacco use in persons aged 15+ years | Afghan people use different tobacco products, including cigarette smoking (21.9%), tobacco chewing (17.7%), tobacco dipping/snuff (14.2%). “Business as usual” will not achieve the smoke-free 2025 goal. A 30% reduction in the current tobacco use will require halving the uptake of smoking and doubling the current quit rate29 | Develop the strategic plan for reaching the target, including start tobacco taxation, increasing funding for sustained, research-based mass media campaigns, implementing the smoke-free public places legislation |
| Physical inactivity | A 10% relative reduction in physical inactivity | A 10% relative reduction in the prevalence of insufficient physical activity by 2025 | Physical inactivity is not a big share (3.41%) of NCDs mortality in Afghanistan. However, considering the population structure in Afghanistan, this amount also can be decreased to achieve the target | Develop a set of priority actions consistent with WHO recommendations, including promoting physical activity in schools and universities and increasing public awareness through campaigns to improve the acceptability and safety of walking and cycling |
| Health systems | Increased uptake of evidence-based medications and behavioral interventions following an NCD event or diagnosis | At least 50% of eligible people receive drug therapy and counseling (including glycemic control) to prevent heart attacks and strokes | Medicines for the treatment of NCDs are not included in the BPHS and Essential Package of Essential Services. In addition, the current recruited counselors working in the health system are not working toward the prevention and control of NCDs | Develop strategic approach including equipping health professionals with relevant skills, regulating and empowering private sectors to lead the tertiary care of NCDs in the health system |
- Abbreviations: AFG, Afghanistan; M&E, Monitoring and Evaluation; NCDs, noncommunicable diseases; NGO, nongovernmental organization; WHO, World Health Organization; YLDs, years lived with disability.
To attain these targets, it will be vital to have collaboration among all interested parties: government, government ministries and agencies; local authorities; civil society; academia; and in some cases, the private sector (excluding the tobacco and alcohol industries and those associated with them, and other “unhealthy commodity” industries, who, evidence suggests, should have no role in formulating national or international NCD policy).30 Agencies involved in working toward targets must keep focused on a limited set of priorities and gradually expand their ambitions as experience accumulates and progress is made. It is important to keep in mind the political realities but also be able to build on opportunities that might arise.
We have outlined a sector-initiated set of national targets that can be used for further developing actions that align with global targets and actions but are specific to Afghanistan. Government leadership and collaboration between the government and all other sectors, together with clear monitoring and accountability arrangements, will be vital to success.
4.2 Study limitations
We explored many data sources for NCDs in Afghanistan, but many of them had on-the-spot or cross-sectional data with different indicator types that could not be used in trend analysis. Since these diseases were not the priority of government and donors in the past 20 years, very few studies were conducted systematically and over the years. So, we had to use the data from GBD, from which the metric proportion of NCD deaths relative to total deaths as an outcome measure was selected. This metric has limitations when it is used in trend analysis. The proportion of cause-specific deaths informs about the relative weight of deaths from that specific cause relative to all-cause deaths, but it does not consider the effect of changes in the population size and changes in the age distribution of the population. However, exploring many different sources, there is no data on age-standardized death rate (ASDR) due to NCDs over the years to be used for trend analysis. So, we recommend Afghanistan government and donors to invest in integrating the NCDs surveillance system into the current Health Management Information System/Digital Health Information System 2 to produce timely and accurate data for this country.
The second limitation of our study is the limited use of secondary data, which was collected from the GBD website so it results in small R2 values for linear regressions and impacted the power of our prediction. The third limitation was the radical changes in the regime in Afghanistan in 2021. This change will affect our prediction since there is no updated data after 2021 to be included in the study and improve the precision of our prediction. Meanwhile, we recommend designing and implementing further research on the calculation of ASDRs data and the calculation of the probability of dying between the exact ages of 30–70 years from any of the four major NCDs.
5 CONCLUSION
In general, our study indicates that without any specific policy and intervention to address NCDs in Afghanistan, not only the SDG's target for NCDs will not meet (25% decline in NCD mortality and morbidity by 2025), but an increase in almost all risk factors prevalence, as well as NCD mortality, will be seen in Afghanistan. As mentioned earlier, most of the risk factors are more prevalent among women. So, there is an urgent need for locally relevant knowledge, supportive policies, adequately equipped health services, and optimal social and physical citizen-friendly environment to address NCDs among citizens, especially women. Finally, controlling and preventing NCDs needs strong leadership and governance, effective coordination, and resource mobilization through the multiple stakeholders in Afghanistan. In addition, these resources should be allocated to train the health workforce on the prevention and management of NCDs and their risk factors, the establishment of a good NCDs surveillance system, and procurement of NCDs required medicine and medical technology in health facilities.
AUTHOR CONTRIBUTIONS
Narges Neyazi, Ali Mohammad Mosadeghrad, and Maryam Tajvar designed the research; Narges Neyazi extracted the data; Narges Neyazi and Ali Mohammad Mosadeghrad wrote the paper. Najibullah Safi and Maryam Tajvar reviewed the article and provided technical input to enrich the paper, and Najibullah Safi also edited the language of the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was approved by the Ethics Committee of Tehran University of Medical Sciences with the core of ethics IR.TUMS.SPH.REC.1397.083.
Open Research
DATA AVAILABILITY STATEMENT
All data sets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.