Cardiovascular disease mortality and air pollution in countries with different socioeconomic status
Abstract
Background
Cardiovascular diseases (CVDs) account for 17.9 million deaths annually. Behavioral risk factors increase the risk of dying from CVD. Air pollution is not included in this risk calculation since the appreciation of air pollution as a modifiable risk factor is still limited. The purpose of this study was to analyze CVD mortality attributed to air pollution in all World Health Organization WHO member states and demonstrate the association of CVD mortality with air pollution depending on countries' income level.
Methods
The CVD death rate was calculated by dividing the number of deaths by the total population. The proportion of the population with primary reliance on clean fuels and technologies for cooking was calculated as an indicator of household air pollution. The annual mean concentration of fine particulate matter ≤2.5 µg/m3 and ≤10.0 µg/m3 to which the population is exposed was used as an indicator of ambient air pollution.
Results
There is a gradual increase in CVD mortality attributed to air pollution from high-income countries (HICs) to low-income countries (LICs). Household air pollution is the major cause of CVD mortality in LICs. Ischemic heart disease mortality attributed to ambient air pollution in all countries is higher than stroke mortality attributed to ambient air pollution. In LIC, mortality from stroke is attributed to household air pollution of 39.27 ± 14.47, which is more than twice the stroke mortality attributed to ambient air pollution at 18.60 ± 5.64, t = 7.17, p < 0.01.
Conclusion
Air pollution control should be an essential component of the CVD preventive strategy, along with lifestyle modifications and effective disease management.
Highlights
-
There is a gradual increase in cardiovascular disease (CVD) mortality attributed to air pollution from high-income countries to low-income countries (LICs).
-
Ischemic heart disease mortality attributed to air pollution in all countries is higher than stroke mortality attributed to air pollution.
-
In LICs, mortality from stroke attributed to household air pollution is more than twice the stroke mortality attributed to ambient air pollution.
-
Air pollution control should be an essential component of the CVD preventive strategy, along with lifestyle modifications and effective disease management.
1 INTRODUCTION
In 2022, noncommunicable diseases (NCDs) killed 41 million people, equivalent to 74% of all deaths globally. Cardiovascular disease (CVD) accounts for most NCD deaths, or 17.9 million people die annually from CVD.1 Traditional risk factors such as smoking, physical inactivity, the harmful use of alcohol, and unhealthy diet all increase the risk of dying from a CVD.2, 3 Air pollution, both outdoor or ambient and household, is not included in this risk calculation despite air pollution being a major contributor to the global burden of disease, with an estimated 12% of all attributable deaths in 2019.3 Despite increasing awareness of the impact of air pollution on population health, appreciation of air pollution as a modifiable risk factor is still limited among the health professionals who are traditionally more focused on the classic risk factors. It is important to raise awareness about the harmful impact of air pollution on CVD mortality among the general population, health care providers, research community, and politicians.
World Health Organization (WHO) NCD Action Plan4-6 emphasizes the most effective ways for CVD mortality decline to successfully achieve the United Nations (UN) Sustainable Development Goal (SDG) 3.4 “by the year 2030, reduce by one-third premature mortality from NCDs through prevention and treatment … .”7
Air pollution control is not reflected in this plan while WHO estimates 6.7 million people die from air pollution and 99% of the world population live in places where air pollution exceeds WHO guideline limits.8, 9 These deaths are attributed to both indoor and outdoor pollution10, 11 and arise from man-made and natural sources of air pollution. Man-made or technogenic air pollution includes electricity production; the burning of solid fuels for cooking and heating in poor households; agriculture; industry; and road transport. The largest source of natural air pollution is airborne dust in the world's deserts. Other natural sources are fires, sea spray, pollen, and volcanoes. There are a number of pollutants that have negative health impacts.9 But there is one called particulate matter (PM) that all studies focus on. PM is everything in the air that is not a gas. These are very small particles made up of sulfate, nitrates, ammonia, sodium chloride, black carbon, mineral dust, and water that are suspended in the air that we breathe. Particles with a diameter of 10 μm (10 millionths of a meter) or less can enter deep inside a person's lungs. But the most health-damaging particles are even smaller. Those with a diameter of 2.5 μm or less—abbreviated as PM2.5—can penetrate the lung barrier and enter a person's blood system. These are extremely fine particles, about one-thirtieth of the diameter of a human hair.8, 9
All studies of the mortality impact of air pollution consider our exposure to PM. Some studies also consider the impact of ground-level ozone. The death toll from ozone is much lower than that of PM. In view of this, WHO did not analyze this pollutant-attributed mortality. Other air pollutants are rarely considered in global studies.9 Evidence for the impacts of PM on respiratory diseases, type 2 diabetes, musculoskeletal disorders, and pregnancy outcomes exists.12 However, we need more data concerning CVD, in particular, ischemic heart disease (IHD) and stroke, which are responsible for the vast majority of the global burden of disease. In 2014, an estimated 7.4 million CVD deaths were due to IHD, and 6.7 million were due to stroke.13 Scientific statements of the American Heart Association and European Society of Cardiology, along with the World Heart Federation and American College of Cardiology, put air pollution as the fourth highest-ranking risk factor for CVD mortality, with more attributable deaths than high low-density lipoprotein cholesterol, high body mass index, physical inactivity, or excessive use of alcohol.14 Population studies conducted in hundreds of urban areas globally indicate a consistent association between short-term variability in PM and CVD deaths,15 while large cohort studies from both high- and low-income settings demonstrate increased CVD incidence and mortality in association with PM levels.16 This could be caused by PM ambient air pollution linked with the progression of atherosclerosis.17
A clear relationship is evident between premature CVD mortality and country income levels. In 2016, in 49 selected countries, more premature deaths in adults aged 30–69 years occurred in low- (LICs) and middle-income countries (MICs) compared with higher income countries.18
In view of the above, we decided to analyze IHD and stroke mortality attributed to air pollution in all WHO member states implementing the WHO NCDs Global Action Plan and reporting the progress to provide health authorities and medical professionals with robust data on the association of CVD mortality with air pollution depending on countries' income levels. We expected that the practical implementation of our findings, along with lifestyle modification measures and proper disease management, would contribute to the enrichment and strengthening of global efforts to achieve SDG 3.4.
2 METHODS
Official WHO statistics and publications were used for the preparation of this manuscript. Based on the countrywide approach, 183 countries with a population of more than 90,000 provided unified data to WHO; the World Bank Classification of countries by income level was used to analyze air pollution-adjusted CVD mortality in countries with different levels of income19: 54 HICs, 53 upper-middle-income countries (UMICs), 47 low-middle-income countries (LMICs), and 29 LICs.
2.1 CVD mortality
IHD and stroke death rates were calculated by dividing the number of deaths by the total population. Age-standardized rates adjust for differences in population age distribution by applying the observed age-specific mortality rates for each population to a standard population. The age-standardized death rates can therefore be used to compare the rates of countries without being affected by differences in age distribution from country to country.
2.2 CVD-attributable mortality
CVD-attributable mortality corresponds to the proportion of CVD deaths that are attributable to an exposure. Attributable implies that the deaths would not have occurred had exposure been absent. CVD mortality is calculated by first combining information on the increased (or relative) risk of a disease resulting from exposure with information on how widespread the exposure is in the population (in case, for instance, ambient air pollution, the annual mean concentration of PM to which the population is exposed). This allows the calculation of the “population attributable fraction,” which is the fraction of disease seen in a given population that can be attributed to the exposure, in this case, the annual mean concentration of PM. Applying this fraction to the total CVD deaths gives the total number of deaths that result from ambient air pollution.8
2.3 Ambient air pollution
The annual mean concentration of fine PM (e.g., PM ≤ 2.5 and PM ≤ 10) to which the population is exposed was used as an indicator of ambient air pollution.
2.4 Household air pollution
Evidence from epidemiological studies has shown that exposure to smoke from incomplete combustion of solid fuels is linked with a range of diseases, including IHD and stroke in adults (25 years and over). Household (indoor) air pollution was considered as exposure to polluting fuels used for cooking, such as solid fuels (wood, coal, animal dung, charcoal, and crop wastes) and kerosene. The proportion of the population with primary reliance on clean fuels and technologies for cooking was calculated as an indicator of household air pollution.
All the WHO methodology is described in the WHO air pollution data portal8 (https://www.who.int/data/gho/data/themes/air-pollution).
2.5 Current tobacco smoking
Current tobacco smoking was defined as the percentage of the population aged ≥15 years who smoked any tobacco products.
2.6 Statistical analysis
All statistical analyses were conducted in SPSS version 22.0 (SPSS Inc.). Continuous data were expressed as mean ± standard deviation (SD) and analyzed by Student's t-test. A two-sided p < 0.05 was considered statistically significant.
3 RESULTS
There is a gradual, statistically significant increase in CVD mortality from HICs to LICs attributed to air pollution (ambient + household) (Table 1 and Figure 1). LICs demonstrate the highest level of mortality both from IHD and stroke, which is significantly higher than mortality in countries with higher levels of income. Only for IHD, there is no difference in mortality between LMICs and LICs (t = 1.40, p > 0.05). In all socioeconomic groups of countries, mortality from IHD is greater than that from stroke (t = 3.23, p < 0.01 for LICs, t = 3.84, p < 0.01 for LMICs, t = 5.57, p < 0.001 for UMICs, and t = 5.44, p < 0.001 for HICs). This difference is more visible in countries with higher levels of income (UMICs and HICs) where mortality from IHD is almost twice higher than mortality from stroke.
| Diseases | HIC (n = 54) | UMIC (n = 54) | LMIC (n = 54) | LIC (n = 29) | ||
|---|---|---|---|---|---|---|
| Ambient and household air pollution | ||||||
| Ischemic heart disease | 16.06 ± 15.09 | 35.65 ± 18.44 | 61.01 ± 35.65 | 69.55 ± 25.81 | ||
HIC/UMIC: t = 6.60, p < 0.001 HIC/LMIC: t = 10.50, p < 0.001 HIC/LIC: t = 10.26, p < 0.01 |
UMIC/LMIC: t = 5.62, p < 0.001 UMIC/LIC: t = 5.42, p < 0.001 LMIC/LIC: t = 1.40, p > 0.05 |
|||||
| Stroke | 4.47 ± 4.29 | 18.20 ± 13.42 | 38.00 ± 20.51 | 51.71 ± 14.94 | ||
HIC/UMIC: t = 7.15, p < 0.001 HIC/LMIC: t = 10.99, p < 0.001 HIC/LIC: t = 16.69, p < 0.001 |
UMIC/LMIC: t = 5.64, p < 0.01 UMIC/LIC: t = 10.06, p < 0.001 LMIC/LIC: t = 3.36, p < 0.01 |
|||||
| Household air pollution | ||||||
| Ischemic heart disease | 0.35 ± 1.69 | 12.78 ± 13.51 | 35.93 ± 23.94 | 46.50 ± 15.00 | ||
HIC/UMIC: t = 6.47, p < 0.001 HIC/LMIC: t = 10.16, p < 0.001 HIC/LIC: t = 16.5, p < 0.01 |
UMIC/LMIC: t = 5.8, p < 0.001 UMIC/LIC: t = 10.00, p < 0.05 LMIC/LIC: t = 2.37, p < 0.05 |
|||||
| Stroke | 0.20 ± 0.98 | 9.16 ± 11.04 | 26.82 ± 18.71 | 39.27 ± 14.47 | ||
HIC/UMIC: t = 5.89, p < 0.01 HIC/LMIC: t = 9.54, p < 0.001 HIC/LIC: t = 14.5, p < 0.001 |
UMIC/LMIC: t = 5.62, p < 0.001 UMIC/LIC: t = 8.66, p < 0.001 LMIC/LIC: t = 3.25, p < 0.01 |
|||||
| Ambient air pollution | ||||||
| Ischemic heart disease | 15.78 ± 14.92 | 25.78 ± 15.06 | 32.40 ± 15.70 | 33.91 ± 21.06 | ||
HIC/UMIC: t = 3.46, p < 0.01 HIC/LMIC: t = 5.43, p < 0.001 HIC/LIC: t = 4.11, p < 0.01 |
UMIC/LMIC: t = 2.14, p < 0.05 UMIC/LIC: t = 1.84, p > 0.05 LMIC/LIC: t = 0.33, p > 0.05 |
|||||
| Stroke | 4.29 ± 4.0 | 10.31 ± 6.25 | 14.80 ± 6.60 | 18.60 ± 5.64 | ||
HIC/UMIC: t = 5.92, p < 0.01 HIC/LMIC: t = 9.05, p < 0.001 HIC/LIC: t = 12.1, p < 0.001 |
UMIC/LMIC: t = 3.48, p < 0.01 UMIC/LIC: t = 6.12, p < 0.001 LMIC/LIC: t = 2.67, p < 0.01 |
|||||
- Note: Data are presented as mean ± standard deviation.
- Abbreviations: HIC, high-income countries; LIC, low-income countries; UMIC, upper-middle-income countries.
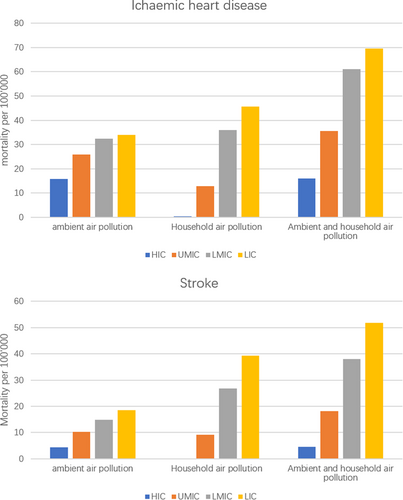
Household air pollution is the major cause of CVD mortality in lower income countries, while only three HICs have signs of household air pollution (Mauritius, Panama, and Romania). CVD mortality attributable to household air pollution, statistically significantly increase from HICs to LICs. There is no difference between IHD and stroke-related mortality when we consider household air pollution in HICs for IHD (0.35 ± 1.69) and for stroke (0.20 ± 0.98) (t = 0.56, p > 0.05) and UMICs for IHD (12.78 ± 13.51) and for stroke (9.16 ± 11.04) (t = 1.5, p > 0.05). However, this difference becomes statistically significant in LMICs for IHD (35.93 ± 23.94) and for stroke (26.82 ± 18.71) (t = 2.06, p < 0.05) and in LICs for IHD (46.50 ± 15.00) and for stroke (39.27 ± 14.47) (t = 1.87, 0.1 ≥ p > 0.05) at 10% probability level.
CVD mortality attributed to ambient air pollution also increases from HICs to LICs, the highest level of which is observed in LICs. From Table 1, we can see that IHD mortality in LICs is more than twice higher than in HICs (t = 4.11, p < 0.001). IHD mortality in HICs is lower compared with UMICs and LMICs (t = 3.46, p < 0.001 and t = 5.43, p < 0.001). However, mortality between UMICs and LICs and LMICs and LICs is not significant (t = 1.84, p > 0.05 and t = 0.33, p > 0.05).
IHD mortality associated with ambient air pollution is almost two to three times higher than mortality from stroke in HICs, UMICs, LMICs, and LICs (t = 5.47, p < 0.001 for HICs, t = 6.91, p < 0.001 for UMICs, t = 7.08, p < 0.001 for LMICs, t = 3.78, p < 0.001 for LICs). The difference in stroke mortality associated with ambient air pollution between HICs and LICs is significant. The highest level of mortality is seen in LICs.
We compared CVD mortality attributed to household air pollution and ambient air pollution (Table 1). IHD mortality attributed to household air pollution in LICs 46.5 ± 15.00 is significantly higher than IHD mortality attributed to ambient air pollution 33.91 ± 21.06, t = 2.2, p < 0.05. In LIC, mortality from stroke, attributable to household air pollution is more than twice the stroke mortality associated with ambient air pollution, 39.27 ± 14.47 versus 18.60 ± 5.64, t = 7.17, p < 0.001. In LMIC difference for IHD attributable mortality between household and ambient air pollution disappears at 35.93 ± 23.94 and 32.40 ± 15.70, t = 0.83, p > 0.05, while for stroke, it remains statistically significant at 26.82 ± 18.71 and 14.8 ± 6.60, t = 4.16, p < 0.001.
We see a reverse picture concerning HICs where IHD mortality attributable to ambient air pollution 15.78 ± 14.92 is much higher than IHD mortality associated with household air pollution 0.35 ± 1.69, t = 7.56, p < 0.001, for HICs and 25.78 ± 15.06 versus 12.78 ± 13.51 for UMICs (t = 4.67, p < 0.001). In HIC, stroke mortality attributable to household air pollution 0.20 ± 0.98 is much lower than ambient air pollution 4.29 ± 4.00, t = 7.13, p < 0.001.
Due to the high heterogeneity of the studied countries from different WHO regions, even with similar income levels, we decided to analyze air pollution impact on CVD mortality in one region with a more homogenic population. WHO Region for Africa (AFRO) includes 47 countries: 21 LICs, 17 LMICs, 7 UMICs, and 2 HICs. AFRO is characterized by a high proportion of countries with primary reliance on polluting fuels and technologies. In our analysis, we combined UMIC and HIC in one group due to the small number of HICs in the region. Only Mauritius and Seychelles belong to HIC, according to the World Bank classification.19 Finally, only Mauritius was included in the analysis since no data from the Seychelles were available.
Figure 2 demonstrates an increase in CVD-attributed mortality associated with household air pollution from HICs to LICs. Concerning CVD mortality associated with ambient air pollution, only stroke mortality demonstrates a gradual increase from HICs to LICs. There is no statistically significant difference between IHD and stroke mortality associated with household air pollution. On the other hand, there is a statistically significant difference between IHD and stroke mortality associated with ambient air pollution. IHD mortality is higher than stroke mortality in LICs (t = 4.04, p < 0.001), LMICs (t = 5.19, p < 0.001), and HICs + UMICs (t = 6.56, p < 0.001).
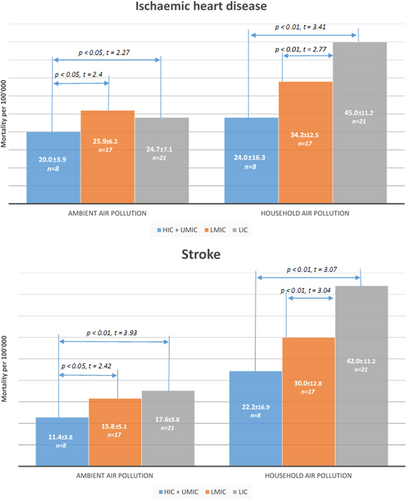
We analyzed the prevalence of smoking in HICs + UMICs and in LMICs and LICs to consider the impact of smoking on air pollution in this group of African countries. It was 18.28% ± 3.68%, n = 7, for HICs + UMICs, 12.33% ± 7.53%, n = 12, for LMICs and 11.23% ± 5.00%, n = 13, for LICs. The difference between HICs + UMICs and LMICs and LICs was statistically significant, t = 2.3, p < 0.05 and t = 3.60, p < 0.01 accordingly.
4 DISCUSSION
Exposure to air pollution is harmful to many NCDs besides CVD.12, 20, 21 As far as CVD is concerned air pollution may increase blood pressure, exacerbate myocardial ischemia, and trigger myocardial infarction.22, 23 A scientific statement from the American Heart Association and multiple clinical studies provided a detailed description of the pathophysiologic mechanisms through which PM triggers cardiovascular events increasing mainly the risk of atherothrombosis.24-26 The European Society of Cardiology expert position paper27 updated the observational and mechanistic evidence and identified air pollution as one of several major modifiable risk factors relevant to the prevention and management of CVD. Recent research also indicates that air pollution impacts cardiovascular health even at very low levels below current WHO guidelines and most national standards.9, 28 Socioeconomic factors play a crucial role in this association. An international prospective cohort study in 21 countries with high- and low-income settings (PURE) demonstrates increased CVD incidence and mortality in low-income settings correlated with PM levels.16
Our previous study in 49 HICs and MICs found significantly higher levels of air pollution, both ambient and household, in MICs than in HICs.18
The current study, including practically all WHO Member States, has clearly demonstrated the association of air pollution with CVD mortality, which strongly depends on the level of socioeconomic development. LICs are most prone to high CVD mortality, where IHD is a major health problem. LICs are most suffering from household air pollution, associated with high CVD mortality. A total of 183 countries included in our analysis is one of the strengths of our study. However, the high heterogeneity of the world population, even divided by income level, incited us to make a similar analysis in more homogenic regions. Our findings confirmed general tendency and specified some of the findings. For instance, the association of IHD mortality with ambient air pollution in AFRO, where there is a statistically significant increase of IHD mortality from higher income countries to lower income countries. However, this increase is not gradual like that for household air pollution, which has become one of the major public health problems in LIC, where IHD and stroke death rates are much higher than the same death rate caused by ambient air pollution.
Around 2.4 billion people worldwide still cook using solid fuels (such as wood, crop waste, charcoal, coal, and dung) and kerosene in open fires and inefficient stoves.1 Most of these people are poor and live in LICs and MICs. Without strong policy action, these people are estimated to still lack access to clean fuels and technologies in 2030.1 There is a particularly critical need for action in sub-Saharan Africa, where population growth has outpaced access to clean cooking, and 923 million people lacked access in 2020. Strategies to increase the adoption of clean household energy include policies that provide financial support to purchase cleaner technologies and fuels, improved ventilation or housing design, and communication campaigns to encourage clean energy use. For instance, programs such as India's Pradhan Mantri Ujjwala Yojana have made clean cooking fuels accessible to millions of households, helping to reduce indoor air pollution.29
In light of the widespread use of polluting fuels and stoves for cooking, WHO issued a set of normative guidance, the guidelines for indoor air quality: household fuel combustion,28 which offer practical evidence-based guidance on what fuels and technologies used in the home can be considered clean, including recommendations discouraging the use of kerosene and recommending against the use of unprocessed coal. The guidelines also specify the performance of fuels and technologies (in the form of emission rate targets) needed to protect health and emphasize the importance of addressing all household energy uses, particularly cooking, space heating, and lighting, to ensure benefits for health and the environment. Preventive measures will also be beneficial for the whole population since household air pollution is also a major contributor to ambient (outdoor) air pollution.
Regretfully, most sources of outdoor air pollution are well beyond the control of individuals and this demands concerted action by local, national, and regional level policy-makers working in sectors such as energy, transport, waste management, urban planning, and agriculture.
There are many examples of successful policies that reduce air pollution.12 Despite these challenges, given its near-ubiquitous exposure, air pollution reduction offers a powerful opportunity to equitably reduce CVD. Experience also indicates a clear path forward. In the United States, reductions in PM concentrations resulting from a diverse array of regulatory actions and technologies were responsible for up to 15% of the increase in US life expectancy observed over the past several decades.30, 31
From the CVD prevention side for many individuals, these changes will not, however, be sufficient, and medical interventions along with lifestyle modification measures will, therefore, also be required.
Patients need long-term access to affordable, quality-assured medicines for disease management that will achieve the desired clinical outcome and improve quality of life. The importance of access to safe, effective, quality, and affordable medicines is reflected in SDG 3.8.32
From this viewpoint, the WHO Package of Essential NCD (PEN) interventions is based around a core set of evidence-based, cost-effective interventions for the prevention and treatment of key NCDs, including CVD in primary care, which are feasible in low-resource settings. PEN protocols may be adapted to different national settings.33
Recently, WHO and the US Centers for Disease Control and Prevention launched the Global Hearts Initiative to scale up prevention and control of CVD, particularly in resource-limited settings. Along with lifestyle modifications, the Initiative is focused on simplified treatment protocols for primary and secondary prevention, appropriate referral using a core set of medicines and basic technologies, and improved service delivery through task-sharing supported by robust clinical monitoring. The Global Hearts Initiative technical package is fully aligned with and complementary to the clinical guidance and core medicines recommended in the WHO-PEN and other best-practice guidelines.2 Tobacco smoking is a major behavioral risk factor for CVD and may contribute to air pollution. Global efforts against tobacco and, in particular, the WHO Framework Convention on Tobacco Control34 , adopted 20 years ago, raised awareness about the harmful effects of tobacco and being successfully implemented globally. Their success is, no doubt, reflected in the smoking prevalence, quality of air, and subsequent health benefits globally, and, in particular, in LICs. Our data35 demonstrate that smoking prevalence in lower income (LMICs and LICs) African countries is still not very high, 12.33% and 11.23%, to have a dramatic impact on the air quality in these countries. CVD mortality attributable to air pollution is higher in LMICs and LICs than in HICs + UMICs, despite the lower prevalence of smoking in LMICs and LICs comparatively with HICs + UMICs 18.28%. It means that other than tobacco components of air pollution, especially indoor air pollution, play at the moment crucial role in CVD-attributable to air pollution mortality, especially in lower income countries.
5 CONCLUSION
Air pollution, especially PM, has been linked to increased CVD mortality and morbidity, and the effect on the cardiovascular system can occur both after short- or long-term exposure.26 Air pollution control should be an essential component of the preventive strategy along with lifestyle modifications and effective disease management.
Air pollution has a close association with CVD mortality and country income level. In LIC, indoor air pollution caused by people living in energy poverty is one of the largest contributors to IHD mortality.
Air pollution control and improving health care quality as a result is an essential element of health system strengthening. Finally, air pollution-attributed deaths are avoidable if air pollution is reduced to levels that would not increase the risk of developing CVD through better housing, less time outdoors during periods of high concentration of pollutants, and filters in the household. These measures, along with the current WHO CVD/NCD preventive strategy as a part of the multistakeholder event, will improve our global efforts in reducing mortality from CVD and timely achieving SDG 3.4.
AUTHOR CONTRIBUTIONS
Nikolai Khaltaev collected data, performed the statistical analysis, and prepared the manuscript. Svetlana Axelrod collected the data and provided intellectual contributions as well as critical revision.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
None.
Open Research
DATA AVAILABILITY STATEMENT
Data supporting the results can be obtained from the corresponding author.