Vertebral artery injury following combination Jefferson fracture of C1 and Type II odontoid fracture: A case report
Yichen Meng, Chenglin Zhang, and Tengfei Song contributed equally to this work.
Key Clinical Message
Traumatic posterior atlantoaxial dislocation combined with Jefferson fracture and odontoid process fracture with vertebral artery injury is rare. The management of such injury raises controversial issues and is still open to debate. A 74-year-old Chinese male presented with sustained neck pain and stiffness after falling from height. The patient was neurologically intact. Preoperative radiographs demonstrated a Jefferson burst fracture with a posterior dislocation of the atlantoaxial joints and odontoid process Anderson and D'alonzo type II fracture. A computed tomography angiography (CTA) showed an occluded left vertebral artery. Coil embolization in the proximal portion of the occluded vertebral artery was performed to prevent further cerebral infarction due to distal embolization of the thrombus. Then a second stage occipito-cervical fusion was performed to reconstruct cervical spine stability. A systematic screening of blunt trauma vertebral artery injuries through CTA is required when dealing with upper cervical fracture. For cases with vertebral artery occlusion secondary to cervical spine injury, endovascular treatment preceding cervical spine surgery is a feasible and a safe treatment.
1 INTRODUCTION
Concomitant dislocation of the C1-2 fracture and odontoid fracture is a rare entity. A recent systematic review has reported that Anderson and D'alonzo type II odontoid fracture causes 78% of traumatic posterior atlantoaxial dislocation (TPAD), which can result in spinal cord injury and further increase the fatal nature of this injury.1, 2 Additionally, fractures involving the upper cervical spine put patients at significant risk of vertebral artery injuries (VAIs).3 Although most of these injuries are clinically silent as the opposing vertebral artery (VA) and the Willis circle provide adequate collateral blood supply, some authors report significantly higher rates of cerebral infarction after an injury.4 Therefore, the survival rate of these cases can only be increased through early diagnosis, meticulous VAI screening, and solid fixation of the fracture. In this report, we describe a patient with TPAD and VAI after falling from a height and discuss management options.
2 CASE HISTORY
Informed written consent was obtained from the patient for publication of this report and any accompanying images. A 74-year-old Chinese male presented with a blunt head trauma after falling from a ladder 10 days ago. He was still able to walk by himself during the immediate post-traumatic period and was brought to a local health care facility. The patient received treatment including immobilization and skull traction and was transferred to our medical center for further treatment. Upon arrival, he complained of sustained neck pain and stiffness, but denied subjective neurological signs such as weakness, numbness, or paresthesia. Physical examination revealed tenderness along the posterior aspect of the upper cervical spine. Neurological evaluation revealed no consciousness, motor or sensory abnormality.
3 INVESTIGATION AND TREATMENT
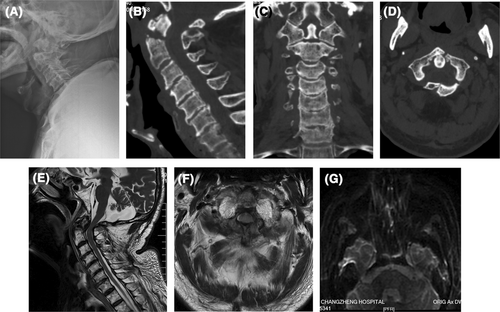
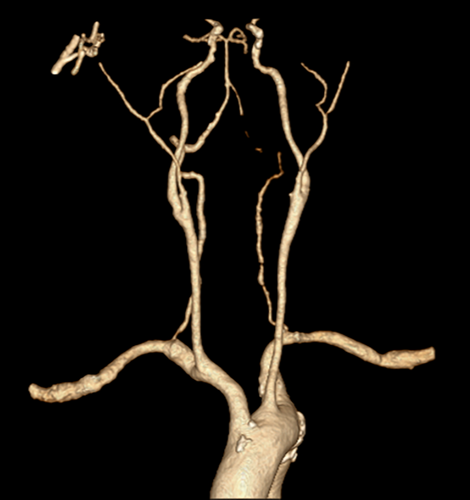
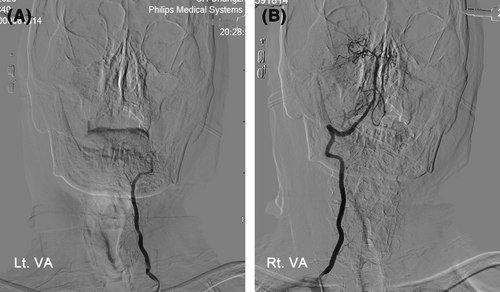
Cervical spine x-rays (Figure 1A) and computed tomography (CT) scans (Figure 1B–D) demonstrated a Jefferson burst fracture with a posterior dislocation of the atlantoaxial joints and odontoid process type II fracture (Anderson and D'alonzo classification). Magnetic resonance imaging (MRI) revealed reduced space available for the spinal cord caused by the fragmented odontoid process but no change in spinal cord signal (Figure 1E,F). As CT scans revealed a fracture through the posterior arch in the region of the vertebral artery sulcus, a computed tomography angiography (CTA) was performed and showed a left VA flow void involving the segments V3 and V4 (Figure 2). But diffusion-weighted MRI of the head showed no acute cerebral infarction (Figure 1G). The patient was then subjected to digital subtraction angiography (DSA), which confirmed the left VA occlusion and determined it to be Grade IV on the Denver Grading Scale (Figure 3A). The right VA angiography showed good visualization of the main intracranial artery (Figure 3B). A diagnosis of VAI and TPAD with Jefferson fracture and odontoid process fracture was made and cervical spine reduction surgery was needed. However, VA hemodynamics were potentially altered during the spine surgery and there was a risk of cerebral infarction due to distal embolization of thrombus. In addition, it has been 15 days since the trauma and there were no neurologic deficits attributable to VAI, indicating the right VA provides adequate collateral blood supply. Therefore, we decided to sacrifice the injured vessel and perform artery occlusion of the left VA.
4 CONCLUSION AND RESULTS
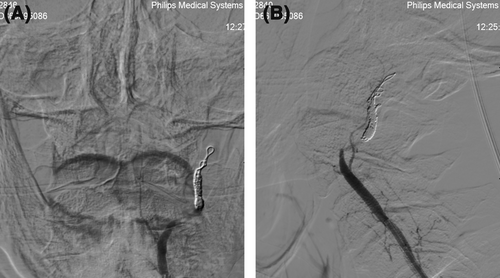
The patient underwent coil embolization in the proximal portion of the occluded VA. Under general anesthesia, a 6-Fr Fubuki dilator kit was inserted through the left femoral artery, guided into the left vertebral artery. A 3.2/3.4-Fr Guidepost and Phenom17 (Medtronic) were guided from the 6-Fr Fubuki dilator kit and coil embolization was performed from the level of the left vertebral artery V3 segment, to the left vertebral artery V4 segment. Left VA angiography confirmed the absence of antegrade blood flow in the left VA (Figure 4). Then on the following days, posterior spinal instrumentation with occipito-cervical fusion to the level of C3 was performed (Figure 5). The procedure was done in a prone position under general anesthesia. C2 fixation with pedicle screw, and C3 with lateral mass screw under C-arm guidance. The occipital plate was fixed with five screws after identifying following landmarks external occipital protuberance superior nuchal line, foramen magnum, and ensuring that the plate is flush with the skull. An iliac bone graft was implanted over the posterior arch of C1 and the C2 lamina. The patient was discharged without any complication after surgery. No new neurological abnormalities were found. The left VA was completely occluded on follow-up angiography (Figure 6).


5 DISCUSSION
Cases involving both Jefferson fracture and odontoid process fracture are rare. A large retrospective epidemiological study conducted in 2000 for a period of 14 years revealed that only 2 of 784 cases were a combination of these injuries.5 The odontoid process acts as a pivoting anchor in the C1–C2 configuration, which makes the trans-odontoid luxation fracture a highly unstable traumatic lesion of the atlantoaxial complex. Posterior instability occurs when the integrity of the bony support, either the odontoid process or the anterior arch of C1 is compromised by major trauma, leading to posterior displacement of C1 in relation to C2.2 Regarding the treatment of atlantoaxial dislocation, there is a consensus that reduction has to be performed as soon as possible in all cases, to prevent residual instability and development of permanent deformity. Several authors reported that the reduction of the dislocation was achieved using traction but all cases were atlantoaxial dislocation with an isolated odontoid process fracture (without C1 fracture).6-8 Our case is unique; TPAD due to both C1 burst fracture and odontoid process fracture. At first, we attempted to perform a closed reduction using skull traction, but there was no evidence of atlantoaxial joint reduction. Therefore, open reduction and fixation were performed.
VAI is a relatively common sequelae of cervical spine injuries, especially those with subluxations or involving the upper cervical spine.7 The literature suggests a 71% prevalence of VAI in patients with cervical spine injury and 18% in those with C2 fractures.9 A recent study reported combined C0-C3 fractures were associated with an increased risk of VAI.10 Therefore, early diagnosis and prophylactic treatment are essential for traumatic VAI. VAI commonly occurs in V3 segments in adults due to the proximity of the atlantoaxial articulation with the transition from V2 to V3 segments.7, 11 In our case, the foramen transversarium of C1, the border between V2 and V3, is the VAI site. CTA is an accurate and reliable tool for diagnosing VAI in patients with sustained blunt trauma.12, 13 In our case, VAI was diagnosed by three-dimensional CTA. And DSA was also performed as endovascular therapy was considered. The management of VAI is very controversial as there is very little high-quality data available to assist decision-making. As VAI of any injury grade has the potential to cause distal posterior circulation ischemia or stroke, anticoagulation or antiplatelet therapy is recommended following known VAI.12 However, up to 14% of patients anticoagulated with IV heparin for VAI will experience significant complications.7 There is an increased risk of serious cerebral infarction due to thrombus scattering after VA recanalization. Kinosada et al. reported a patient with VA occlusion who experienced cerebral infarction after spontaneous VA recanalization by administration of heparin and aspirin.14 Lauerman et al. reported the incidence of cerebral infarction in patients diagnosed with traumatic vertebral artery occlusion when recanalization occurred was 22.2%.15 Additionally, in many cases of cervical spine injury, the vertebral artery is mechanically occluded, and when the occlusion is released by repair, recanalization occurs, resulting in cerebral infarction.15 On the other hand, coil embolization was recently documented to prevent secondary stroke, with a low risk of ischemia due to “embolization of the occluded vessel.”16, 17
VAI and TPAD combined with Jefferson fracture and odontoid process fracture are even more rare. To the best of our knowledge, only one case has been reported before.3 In that case, VAI was asymptomatic and was left untreated. Unfortunately, the patient experienced brainstem and cerebellar infarction 3 months after VAI. Based on these considerations, we prophylactically embolized the proximal portion of the left vertebral artery with coils prior to cervical spine surgery. Consequently, this could prevent the dispersal of the thrombus from the vertebral artery following the surgery.
From this rare case of TPAD combined with Jefferson fracture and odontoid process fracture with VAI, we recommend a CTA as a screening tool for vascular injury. Solid fusion with internal fixation is necessary to reconstruct the joint stability. Endovascular treatment with coil embolization preceding cervical spine surgery is a feasible and a safe treatment for traumatic vertebral artery occlusion.
AUTHOR CONTRIBUTIONS
Yichen Meng: Investigation; writing – original draft. Chenglin Zhang: Data curation; methodology. Tengfei Song: Methodology; writing – original draft. Rui Gao: Conceptualization; supervision; visualization; writing – review and editing. Xuhui Zhou: Conceptualization; writing – review and editing.
ACKNOWLEDGMENTS
The authors have nothing to report.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
ETHICS STATEMENT
The study was conducted in accordance with the Declaration of Helsinki. The patient provided written informed consent to participate in the study.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.




