A rare coincidence of Turner syndrome and bronchiectasis: A case report
Abstract
Similar to bronchiectasis, Turner syndrome is possible to have more pathological manifestations or etiologies than what has already been documented. Slower recovery process is expected when treating a patient with several comorbidities like Turner syndrome. Turner syndrome patients are vulnerable and should be extensively monitored to lower late presentation rates.
1 INTRODUCTION
Turner syndrome (TS) is a condition seen in phenotypic females, which results when one of the X chromosomes (sex chromosomes) is missing or partially missing and has a prevalence of 1 in 2000 to 2500 live-born female children.1 Clinical presentation varies significantly in Girls with TS, especially those with lower degrees of mosaicism for monosomy X, who may not present with the classic phenotype.2 TS's clinical manifestations might include the following common signs and symptoms: short stature, pubertal delay/ovarian insufficiency, cardiac and renal abnormalities, sensorineural hearing loss, ophthalmologic problems, thyroid abnormalities, metabolic syndrome, inflammatory bowel disease, and neurocognitive issues.3 The diagnosis of TS can be established at a wide range of ages.4, 5 In the prenatal period, the ultrasound findings of increased nuchal translucency, cystic hygroma, and left-sided obstructive cardiac anomalies (especially coarctation of the aorta) in any fetus are highly suggestive of TS, and test to confirm the diagnosis prenatally by amniocentesis or chorionic villous sampling is necessary,6 Webbed neck, lymphedema, or coarctation of the aorta in infancy should prompt a peripheral blood karyotype to rule out TS.6 However, several girls have delayed diagnosis in late adolescence or early adulthood, with some estimates indicating that up to 38% of TS patients are diagnosed in adulthood.7 Diagnosis is made by sex chromatin [Barr body] detection, and chromosomal karyotyping is necessary to diagnose and identify the fraction of “Y” chromosome elements.
The associations of TS with congenital heart disease have been described widely in the literature. Up to one-third of the patients with karyotype 45, X may have coarctation of the aorta: In addition, patients with hypertrophic cardiomyopathy, septal defects, dextrocardia, and anomalous pulmonary venous drainage have been reported anecdotally.8
Bronchiectasis, a disease that presents clinically with repeated respiratory infections requiring antibiotics, disabling productive cough, shortness of breath, and hemoptysis, has rarely been reported to be associated with Turner syndrome in the medical literature.8 The disease primarily involves the bronchi and bronchioles, described as a vicious circle of transmural infection and inflammation with mediator release, and it is also related to retained inflammatory secretions and microbes in the small airways that would cause obstruction damaging the airway leading to recurrent infection.9 However, treatment in clinical practice is still based on antibiotics, pulmonary rehabilitation, and surgery in rare cases; many new treatments have been suggested over the last few years.9
We present a case of a unique coexistence between TS and bronchiectasis. Such case is the first describing this rare association. It is important to be addressed properly in case of similar future cases.
2 CASE PRESENTATION
A 32-year-old female patient presented to the emergency department with respiratory complaints. She reported repeated chest pain and mild dyspnea. Her medical history involves TS, Hypertension, and chronic kidney disease, which requires dialysis three times per week. Her stature is short, and her chest is broad, consistent with TS. On physical examination, orthopnea and fine bilateral crackles have been noticed. Room air oxygen saturation was low, and COVID-19 was excluded after doing a PCR test. She was admitted to the intensive care unit due to an unstable overall condition.
Initial blood works showed markedly elevated white blood cells (15.17109/L) with neutrophils dominance (77.6%), hemoglobin (9.6 g/dl), hematocrit (28.3%), CRP (93 mg/L), and LDH (809 U/L). Other tests have been done, including procalcitonin (11.5 ng/ml), IL-6 (62.3 ng/ml), and D-dimer (7.31 ng/ml). Urea, creatinine, and electrolytes are usually mildly elevated before dialysis. Gene-Xpert test has excluded tuberculosis.
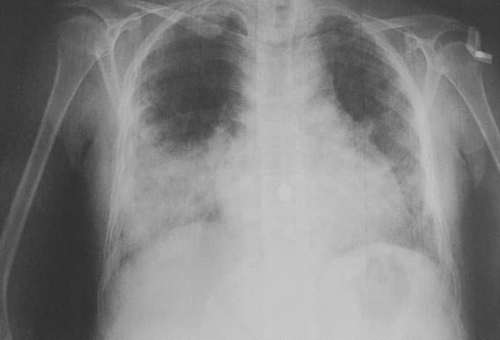
Chest X-ray revealed bilateral peripheral infiltrations and ground-glass opacities (Figure 1). Infective pneumonia with hypoxia was the initial diagnosis. Also, a high anion gap metabolic acidosis was complicating her case. Later, a CT scan was ordered and revealed clear signs of bilateral bronchiectasis (Figure 2). An echocardiogram showed slight left ventricular hypertrophy, insignificant right atrial enlargement, and no coarctation of the aorta.

During her stay in the intensive care unit, she has been treated with broad-spectrum antibiotics, as ceftriaxone and metronidazole, non-invasive oxygen therapy, and repeated dialysis. She had a slow recovery process. Despite that, she has finally shown signs of clinical improvement and was discharged without any need for oxygen supplementation or bronchodilators.
3 DISCUSSION
This case is a presentation of a rare association between TS and bronchiectasis. To our knowledge, this coexistence is rare and hardly ever reported in the literature. The patient came to the emergency department with long-term respiratory symptoms that started to limit her daily activities. She had the typical morphological and pathological features of TS. Bronchiectasis was only confirmed after ordering the CT.
Many etiologic factors have been described to cause bronchiectasis.10 Rarely enough, a case of ciliary aplasia was reported as a cause of bronchiectasis in TS.11 The etiology of our case's bronchiectasis has not been determined. Both cystic fibrosis and ciliary aplasia were excluded. Bronchiectasis etiology is possible to be congenital. However, as there is only a little data on this association, TS cannot be established yet as a primary cause for congenital bronchiectasis. Further research should be done to study this correlation.8
The 32-year-old patient is amenorrheic with underdeveloped female organs. She has never received hormone replacement therapy (HRT). It might be beneficial for future studies to consider following the absence of HRT when dealing with TS and bronchiectasis.
She has never reported similar respiratory symptoms before, and her medical history is remarkable in terms of repeated upper or lower airway infections. Infective pneumonia was treated by a regular protocol without particular consideration for TS. It is worth mentioning that her recovery process was noticeably slower than non-TS patients with similar presentations. Because of her overall vulnerability due to chronic diseases, her slow recovery cannot be restrictedly addressed to TS. After one year of discharge, no recurrence has been reported to the moment.
4 CONCLUSION
The coexistence of Turner syndrome with bronchiectasis is a rare combination that should increase the awareness of clinical doctors and pulmonologists. Following proper treatment and suitable diagnostic techniques are required when encountering a similar case in a clinic or hospital; we also emphasize the importance of carefully checking the medical history before administering any treatment. It is also vital for the treating doctor to be opened-up for possibilities of new pathologies to an already known syndrome.
AUTHOR CONTRIBUTIONS
All authors have contributed in writing and reviewing the artilce.
ACKNOWLEDGMENTS
Our sincere thanks to all the doctors and nurses who participated in the treatment of this case.
CONFLICT OF INTEREST
No conflict of interest exits in the submission of this manuscript.
ETHICAL APPROVAL
Ethical approval was given by the Aleppo University Hospital. Consent to participate was taken directly from the patient.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Open Research
DATA AVAILABILITY STATEMENT
All data generated or analyzed are included in this article.




