Spectrum of thyroid disease in a single patient: A case of papillary thyroid carcinoma in a patient with Graves' disease and Hashimoto's thyroiditis
Abstract
A 65-year-old man with a history of Hashimoto's thyroiditi on Levothyroxine developed Graves' disease with ocular symptoms and was treated with teprotumumab without improvement. Total thyroidectomy was performed to control hyperthyroidism. Surgical pathology revealed multifocal papillary thyroid carcinoma. Rarely, a spectrum of thyroid disorders is seen in a single patient.
1 INTRODUCTION
Hashimoto's thyroiditis and Graves' disease are the most common autoimmune thyroid disorders. Hashimoto's thyroiditis is the most common type of primary hypothyroidism and Graves' disease is the most common type of primary hyperthyroidism. The conversion of hyperthyroidism to hypothyroidism has been reported, but the conversion of hypothyroidism to hyperthyroidism has been considered a rare phenomenon.1 In addition, studies have associated Hashimoto's thyroiditis with an increased risk of developing papillary thyroid carcinoma.2 In this case report, we present at 65-year-old man who was incidentally discovered to have papillary thyroid carcinoma following conversion of Hashimoto's thyroiditis to Graves' disease. This case highlights a rare instance of a single patient presenting with the full spectrum of thyroid disease: Hashimoto's thyroiditis, Graves' disease, and papillary thyroid carcinoma.
2 CASE PRESENTATION
A 65-year-old Caucasian male with past medical history of Hashimoto's thyroiditis and GERD presented to the endocrinology office for evaluation of hyperthyroidism. The patient presented with symptoms of binocular diplopia (L > R), proptosis, ocular dryness, and erythema. The patient's main concern was regarding difficulty driving due to his ocular symptoms. On physical examination, the patient had a normal-sized thyroid, without palpable nodules and no evidence of bruit or thrill. Eye examination revealed bilateral proptosis (left greater that right), conjunctival erythema, limitation of lateral gaze bilaterally, and lower lid retraction bilaterally. He reported that the diagnosis of Hashimoto's thyroiditis was made 1 year prior, and he was started on thyroid hormone replacement with levothyroxine 150 mcg at that time. He became hyperthyroid while on levothyroxine and the dose was gradually decreased over a period of 7 months and eventually discontinued prior to his initial presentation. The patient denied any family history of thyroid disorders and any prior tobacco use. He admitted to rare alcohol consumption.
The patient was found to have biochemical evidence of hyperthyroidism including thyroid stimulating hormone (TSH) suppression with a value of 0.01 mIU/L (normal range: 0.5–5 mIU/L) and free thyroid hormone (FT4) value of 2.2 ng/dL (normal range: 0.7–1.9 ng/dL), thyroid stimulating immunoglobulin (TSI) of 343% (normal range: <130% baseline). Thyroid US revealed a 0.7 cm mixed nodule in the right upper lobe, 0.7 cm mixed hyperechoic nodule in the right middle lobe, and 0.5 cm hyperechoic nodule in the left middle lobe. Based on the presence of ocular symptoms, other physical examination findings, biochemical hyperthyroidism and elevated TSI levels, the diagnosis of Graves' disease was made. The patient was started on methimazole 10 mg daily. The dose of methimazole was decreased over the next few months to 2.5 mg daily to achieve and maintain biochemical euthyroidism.
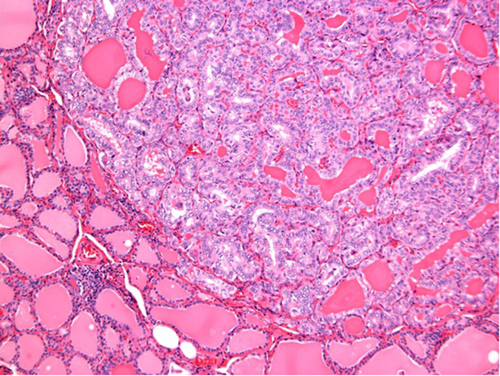
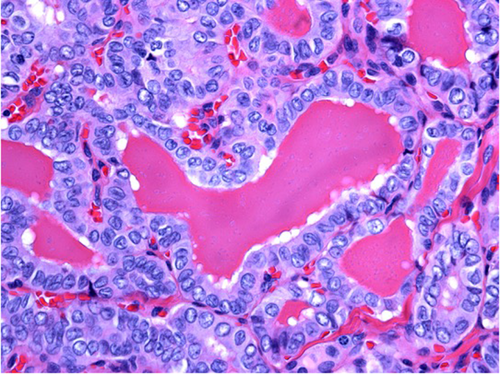
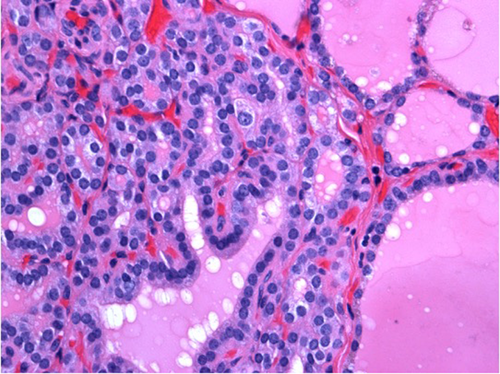
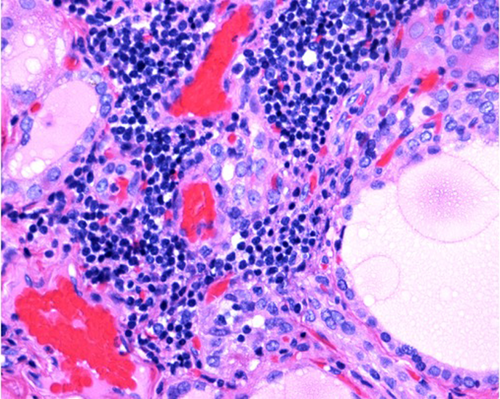
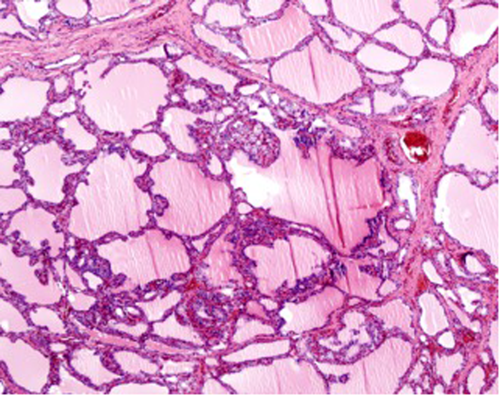
Due to significant diplopia and proptosis, the patient was deemed to be a good candidate for teprotumumab. However, despite completing seven out of eight cycles of therapy, he reported no resolution of his visual symptoms. He was not felt to be a candidate for radioactive iodine therapy given his active eye disease. Total thyroidectomy was advised as a permanent treatment option to control hyperthyroidism with the expectation that decreasing TSI would lead to improvement of his visual symptoms in the future or allow him to undergo surgical correction of his orbitopathy. Final surgical pathology following thyroidectomy revealed papillary thyroid carcinoma, follicular variant, with 3 foci ranging in size 0.1–0.5 cm, unencapsulated, involving both lobes of the thyroid and isthmus (Figures 1 and 2), thyroid follicular hyperplasia, papillary hyperplasia and lymphocytic infiltrates (Figures 3, 4, and 5).The patient was started on levothyroxine following thyroidectomy and remained euthyroid since then.
3 DISCUSSION
Hashimoto's thyroiditis is the most common type of autoimmune thyroid disease and type of primary hypothyroidism. Hashimoto's thyroiditis is diagnosed with clinical and biochemical evidence of a hypothyroid state. Diagnosis includes elevated TSH, low FT4, positive autoimmune antibodies including anti-thyroperoxidase and anti-thyroglobulin antibodies. In Hashimoto's thyroiditis, there is lymphocytic infiltration of thyroid follicular cells, often resulting in fibrosis of the thyroid.3 Females are disproportionately more affected than males.4 There are certain genetic and environmental factors that increase one's risk of developing Hashimoto's thyroiditis. There is an increased association among gene loci and Hashimoto's including HLA-DR3, HLA-DR4, and HLA-DQ.5 In addition, excessive iodine intake has been associated with increased risk of Hashimoto's thyroiditis.6 Patients with Hashimoto's thyroiditis typically present with a constellation of symptoms including fatigue, dry skin, constipation, cold intolerance, weight gain, goiter, and neck pain.7 Patients are typically treated with levothyroxine to establish a euthyroid state.7 In our case, the patient was diagnosed with Hashimoto's thyroiditis and treated with a full weight-based dose of levothyroxine 150 mcg for 1 year. He developed clinical and biochemical evidence of hyperthyroidism and presented to the endocrinology office for further care.
Graves' Disease is the most common type of hyperthyroidism, commonly affecting individuals 30–50 years of age. Similarly to Hashimoto's thyroiditis, females are disproportionately more affected by Graves' disease than males.8 Graves' disease is diagnosed with clinical and biochemical evidence of a hyperthyroid state, such as low to suppressed TSH, high FT4 and autoimmune antibodies including thyroid stimulating immunoglobulins (TSIs). There has been a proposed association between low iodine intake and Graves' disease.6 In Graves' disease, the immune system produces thyroid stimulating immunoglobulins that cause the thyroid to produce excessive thyroid hormone. The clinical manifestations of Graves' disease vary from person to person and depend on the severity of the disease. Common symptoms include weight loss, palpitations, dyspnea, tremor, fatigue, heat intolerance, and hair loss. Graves' disease can also manifest with ocular symptoms including lid lag, lid retraction, diplopia, periorbital edema, and scleral injection.8 Graves' disease can be complicated by severe ophthalmopathy including corneal breakdown and optic neuropathy.9 In our case, the patient presented with symptoms of severe ophthalmopathy including bilateral proptosis (L > R), diplopia, erythema, and dryness. Graves' disease can be managed with anti-thyroid drugs, surgical resection, or radioactive iodine therapy. Anti-thyroid medications include methimazole, carbimazole, and propylthiouracil, which inhibit thyroid hormone production. Radioactive iodine has also been widely utilized to treat patients with Graves' disease but has the adverse side effect profile of worsening Graves' ophthalmopathy.10 In this case, the patient was diagnosed with Graves' disease due to presence of orbitopathy, suppressed TSH and positive TSIs. The patient achieved biochemical control of his hyperthyroidism with methimazole 2.5 mg. Afterwards, total thyroidectomy was performed to alleviate his ocular symptoms and to enable permanent control of his hyperthyroidism. Radioactive iodine treatment was not recommended to prevent worsening ophthalmopathy.
There have been reported cases of conversion of hyperthyroidism to hypothyroidism, which seem to be more exceedingly common than the converse as seen in our patient.11 The conversion of hypothyroidism to hyperthyroidism has been considered a rare phenomenon, but there are an increasing number of cases reported.11-13 The exact mechanism of conversion of hypothyroidism to hyperthyroidism is still under investigation, but there are a few theories that have been postulated. One theory suggests that an imbalance of thyroid stimulating and blocking antibodies may contribute to the thyroid state and subsequent conversion.12 Another theory suggests that in genetically susceptible individuals, an environmental trigger may play a role in conversion from hypothyroidism to hyperthyroidism.13 In this case, it is unclear what triggered the conversion of Hashimoto's thyroiditis to Graves' disease. An imbalance of autoimmune thyroid antibodies may have contributed to the conversion and corresponding ocular thyrotoxicosis symptoms. Our patient's conversion from hypothyroidism to hyperthyroidism within 1 year is the shortest time interval of conversion reported in current literature.14
In patients with Hashimoto's thyroiditis, there is a rare cause of a transient hyperthyroid state, called Hashitoxicosis. Hashitoxicosis precedes the signs and symptoms of the hypothyroid state associated with Hashimoto's thyroiditis and lasts a few weeks to months. It occurs as a result of the biochemical release of preformed thyroid hormone due to autoimmune destruction of the thyroid. Patients may present with biochemical laboratory results and clinical symptoms consistent with a hyperthyroid state that mimics Grave's disease.15 While this unique phenomenon is a cause of hyperthyroidism, it is an unlikely cause of the hyperthyroid state in our patient. The patient presented with biochemical and clinical evidence of hyperthyroidism following his hypothyroid state. Additionally, the patient's hyperthyroid state lasted greater than 1 year, longer than the typical transient hyperthyroid phase of Hashitoxicosis. While Hashitoxicosis was on the differential diagnosis for our patient, it was ultimately ruled out due to time frame of the patient's hyperthyroid state.
Papillary thyroid carcinoma is the most common type of thyroid malignancy, representing 70%–80% of all diagnosed thyroid cancers.16 There is some controversy whether there is a relationship between Hashimoto's thyroiditis and development of papillary thyroid carcinoma. Prior research studies suggest that Hashimoto's thyroiditis is associated with an increased risk of developing papillary thyroid carcinoma.2, 17 A meta-analysis that evaluated histopathologically proven papillary thyroid carcinoma provides evidence to suggest that there is a strong association between Hashimoto's thyroiditis and papillary thyroid carcinoma compared to other benign thyroid conditions and thyroid cancers.18 Other studies found no evidence to support the relationship between Hashimoto's thyroiditis and papillary thyroid carcinoma.19 There are a few different hypotheses regarding the pathogenesis from Hashimoto's thyroiditis to papillary thyroid carcinoma. One hypothesis suggests that in Hashimoto's thyroiditis, the chronic inflammatory state and lymphocytic infiltration results in damage, promoting pathogenesis of papillary thyroid carcinoma.20 Another hypothesis suggests that in Hashimoto's, the elevated TSH levels stimulate follicular epithelial cell proliferation and increase the likelihood of malignant transformation to papillary thyroid carcinoma.21 A study investigating biopsy proven co-existing papillary thyroid carcinoma and Hashimoto's thyroiditis demonstrated associations including a higher female predominance, multifocal involvement of the thyroid, no involvement of extrathyroidal structures, and no lymph node metastasis.18 In this case, surgical pathology following total thyroidectomy revealed papillary thyroid carcinoma with multifocal involvement of the thyroid gland involving both thyroid lobes and isthmus. The patient underwent total thyroidectomy for permanent control of hyperthyroidism and the finding of thyroid malignancy was incidental. Hashimoto's thyroiditis may have contributed to an increased risk of developing papillary thyroid carcinoma. In addition, the patient demonstrated multifocal involvement of the cancer, no extrathyroidal cancer involvement, and no lymph node metastasis, consistent with prior research studies regarding the association of Hashimoto's thyroiditis and papillary thyroid carcinoma. Furthermore, Graves' disease with thyroid nodular lesions has also been associated with an increased risk of developing papillary thyroid carcinoma. In this case, thyroid US demonstrated nodular lesions in the right upper and middle lobes and left middle lobe of the thyroid. The combination of nodular thyroid lesions and Graves' disease may have also increased the patient's risk of subsequent development of papillary thyroid carcinoma.
This case report highlights the need for a high index of suspicion for Graves' disease if a patient with a known diagnosis of Hashimoto's thyroiditis is presenting with thyrotoxic symptoms, regardless of the time interval elapsed from initial diagnosis. This patient presented with symptoms of ocular thyrotoxicosis only 1 year following treatment with levothyroxine. This represents the shortest reported time interval in current literature regarding transformation from hypothyroidism to hyperthyroidism. In addition, this patient was incidentally diagnosed with papillary thyroid carcinoma following thyroidectomy, which provides further evidence to suggest papillary thyroid carcinoma may be associated with Hashimoto's thyroiditis and Graves' disease.17, 21-23 This case depicts the unique spectrum of thyroid disease in a single patient: conversion of hypothyroidism to hyperthyroidism and presence of papillary thyroid carcinoma, all in the same gland. Future studies investigating this distinct conversion can provide further insight into the association between autoimmune thyroid disease and thyroid malignancy
AUTHOR CONTRIBUTIONS
PP drafted and prepared the original manuscript. JM and JP obtained patient data and revised manuscript for important intellectual content from an endocrinology perspective. ZB provided insight from a histopathological perspective and revised the manuscript for important intellectual content from a pathology perspective. PP, JM, and JP contributed equally to literature review and revising manuscript drafts. All authors approved of the final submission and have made significant contributions to the manuscript.
ACKNOWLEDGMENTS
We would like to acknowledge Lisa, M. Price, MSLIS, for editorial consulting.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest to be reported.
ETHICAL APPROVAL
This study did not include any experiments on animals or human subjects.
CONSENT
Written informed consent was obtained from the patient to publish this case report.
PERMISSION TO REPRODUCE MATERIAL FROM OTHER SOURCES
N/A
CLINICAL TRIAL REGISTRATION
N/A
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




