Post-traumatic missing talus: Staged allograft interposition and fusion. Should we fuse the “talo-navicular” joint?
Abstract
Complete talar dislocation—extrusion is an uncommon sequela of high-energy trauma. When the talus is unavailable for reimplantation, a staged treatment plan with the use (a) of an antibiotic cement spacer, followed by (b) tibiotalocalcaneal fusion with bone allograft interposition, may ensure a good clinical outcome.
1 CASE PRESENTATION
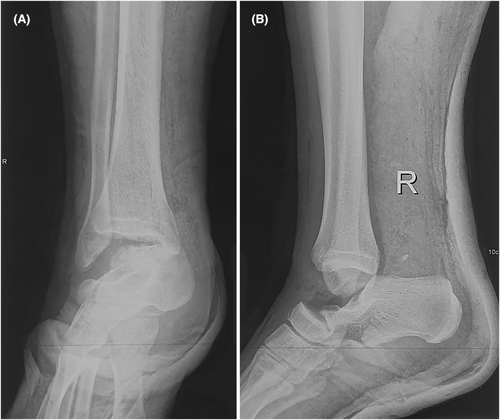
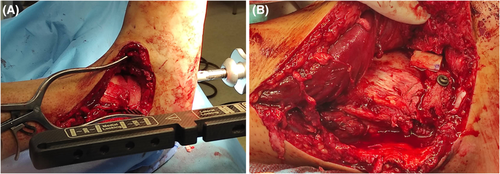
A 24-year-old man with an unremarkable medical history sustained head and visceral trauma along with a twisting “open” right ankle injury in a highway motor vehicle accident and presented unconscious with a contaminated laceration of the lateral side of the ankle in a local District General Hospital. The ATLS guidelines were followed, and he was transferred in our hospital hemodynamically stable. The sensory and vascular findings of the foot were normal. The radiographs of the ankle revealed complete talus absence, which was never found in the accident site (Figure 1). A bilateral CT imaging was performed (Video S1). He was taken to the operating room later the same day for debridement followed by implantation of a cement spacer impregnated with 1 g vancomycin and 1 g gentamycin, which was fashioned by hand according to the dimensions of the contralateral talus (Figure 2). The spacer was positioned to stabilize the clear space and avoid capsular ligament retraction. Three months postoperatively, the laboratory infection markers were within normal limits and the second reconstruction stage was performed. Through a transfibular approach, a distal fibular resection was performed, and the spacer was replaced by a femoral head allograft. Fusion of the ankle and subtalar joints were achieved with a tibiotalocalcaneal nail with interposition of the allograft, and the “talo-navicular” joint was stabilized with partial-threaded screws (Figures 3 and 4A). The fibula was resected as part of the approach and used as bone autograft (Figure 4B). The postoperative course was uneventful, and the radiographic evaluation revealed a well-incorporated allograft fusion. Six months postoperatively, the “talo-navicular” screws were removed, and a painless fibrous union was identified. The patient remains asymptomatic 2 years after the injury (Figure 5, Video S2). The two-year follow-up American Orthopedic Foot and Ankle Society ankle-hindfoot score was 73 of 100 and the Olerud and Molander ankle score was 75 of 100.



2 DISCUSSION
Complete talar dislocation—extrusion is an uncommon sequela of high-energy trauma.1 Reimplantation of the talus is a reasonable option; however, the appropriate treatment in cases of missing bone or severely contaminated talus remains controversial. Complications such as infection, deformities, leg length discrepancy, and post-traumatic arthritis may compromise the outcomes. A staged treatment plan with (a) the use of an antibiotic cement spacer followed by (b) tibiotalocalcaneal nail with allograft interposition and fibrous union of the “talo-navicular” joint, may ensure a good clinical outcome.2 The allograft interposition ensured the preservation of leg length and hindfoot anatomy, and the stabilization of the “talo-navicular” joint resulted in a fibrous union, which remained mobile and asymptomatic.
AUTHOR CONTRIBUTIONS
DK drafted and submitted the manuscript. DR obtained the photographs and contributed to patient care. DR and IS extracted patient history and assisted in completing edits. DG and VL contributed to patient care and critically reviewed the manuscript. IB critically reviewed the paper.
FUNDING INFORMATION
No funding was received for this study.
ACKNOWLEDGMENT
None.
CONFLICT OF INTEREST
There is no conflict of interest associated with this publication, and there has been no financial support for this work that could have influenced its outcome.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordence with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.




