Rare case of pneumoperitoneum in nonintubated COVID-19 patient
Abstract
We report a rare case of a 50-year-old female patient with COVID-19 presented to the emergency department where supplementary oxygen is delivered via noninvasive face mask ventilation. X-ray imaging confirmed the existence of pneumoperitoneum. CT scan was not applicable due to the advanced status of the patient.
1 BACKGROUND
COVID-19 was first appeared in the late 2019, which is a highly infectious disease that spreads rapidly around the world.1 It commonly causes respiratory manifestations such as coughing, shortness of breath, fever, and fatigue. However, a small percentage of patients have shown severe symptoms such as hypoxia and respiratory failure, which require special care to prevent them from fatal complications.2 Thus, the severe case may need supportive ventilation to remain their oxygen saturation in normal range.3 Despite that, sometimes excessive invasive ventilation or nasal cannula can cause treatment complication such as subcutaneous emphysema, and pneumomediastinum which can lead to pneumoperitoneum by Macklin effect.4 However, pneumoperitoneum is the presence of air within the peritoneal cavity that commonly occurs by surgical intervention, visceral perforation, gastric or duodenal ulcers or by spontaneous bacterial peritonitis thoracic causes such as pneumothorax, or cardiopulmonary resuscitation. Spontaneous pneumoperitoneum is a rare subtype that usually caused by barotrauma due to mechanical ventilation, or emergency intubation, and it is called an idiopathic spontaneous pneumoperitoneum when there is no obvious reason for its occurrence.5, 6 Herein, we report a rare case of spontaneous pneumoperitoneum secondary to supplementary oxygen delivery via face mask ventilation in a patient with severe COVID-19 infection.
2 CASE PRESENTATION
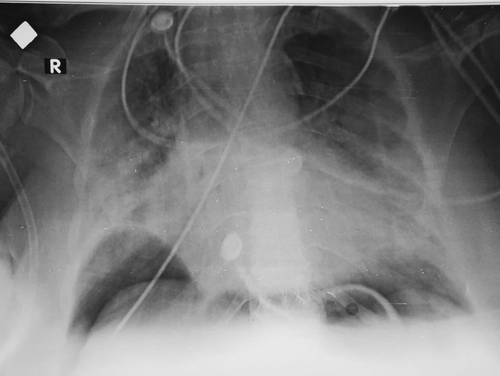
A 50-year-old female patient presented to the emergency department of Aleppo University Hospital complaining of shortness of breath. The medical history revealed a watery diarrhea, headache, fever, malaises for 6 days, and shortness of breath on the same day she came to the hospital. Physical examination revealed cyanosis, and vital signs were as follows: temperature, 39°C; oxygen saturation (SO2), 35%; blood pressure (BP), 120/60 mmHg; heart rate, 100 bpm; and respiratory rate, 35 breath/min; she was conscious and able to talk and breath; thus, she was admitted in the intensive care unit (ICU), with conducting noninvasive ventilation (NIV) with oro-facial mask to prevent respiratory arrest and exacerbation of cyanosis. After that, full blood tests and blood gases tests were performed, which revealed increased levels of C-reactive protein (134 mg/L), WBC (32,900/cmm3), and decreased hemoglobin (9.6 g/dl), and hematocrit (30.7%). After the ventilation, the patient's general condition was improved, as the oxygen saturation (SO2) was 90%, heart rate 90 bpm, and the cyanosis disappeared. After that, polymerase chain reaction (PCR) assay for COVID-19 was conducted. Next day, PCR test revealed positive infection of COVID-19; thus, she started COVID-19 treatment plan. By following up the patient's condition on the next day, chest X-ray revealed bilateral air bubble sign with 3.5 cm diameter under the right lung with no signs of pneumothorax (Figure 1). The patient’s condition was not appropriate to conduct a CT scan. The abdominal examination was clear, and abdominal ultrasound was performed which showed no signs of perforated organs; thus, the diagnosis was confirmed as spontaneous pneumoperitoneum. The surgical abdominal investigation was not appropriated due to the patient’s condition; thus, the patient continued the treatment of COVID-19 with NIV. After 3 days in the ICU, the vital signs deteriorated with a severe pneumonia, and unfortunately, the patient died.
3 DISCUSSION
Pneumoperitoneum is defined as the presence of air or another type of gas within the peritoneum cavity. The main symptoms are abdominal pain, infection, and diarrhea. There are many causes that lead to pneumoperitoneum, but the most common is a perforation or rupture within any organ in the abdominal cavity, whether this is due to a perforated peptic ulcer, tumor, or abdominal trauma.7 But when the pneumoperitoneum is idiopathic, it is usually called spontaneous pneumoperitoneum, where it can result from mechanical ventilation or tracheal rupture after emergency intubation.8 This has been observed during the COVID-19 pandemic, where patients have an increased risk of spontaneous pneumoperitoneum, in the ICU suffers from hypoxia and dyspnea, which requires treatment by intubation and mechanical ventilation. There are a few cases in the medical literature that reported pneumoperitoneum in COVID-19 patients as a result of intubation or mechanical ventilation. According to Ramon Vidrio Duarte et al.8 a 63-year-old male patient with diabetes was admitted to the COVID-19 unit at their institution. After conducting a high-flow nasal cannula, an X-ray showed bilateral, multifocal, and peripheral infiltration with ground-glass pattern, along with apparent subdiaphragmatic free air. The computed tomography (CT) showed pneumoperitoneum, with a radiological sign of the Macklin effect, and no evidence of visceral perforation or other possible cause of gas gathering in the peritoneal cavity. In our case, because of the patient's bad status, we could not perform a CT scan to exclude the Macklin effect. SARS-CoV-2 infects cells through the angiotensin-converting enzyme-2 receptor, which is very abundant in the lungs but also exists in the intestinal mucosa which causes direct damage to the mucosa cells, in addition to the ischemic mechanisms secondary to arterial and venous splanchnic thrombosis.9 The severe systemic inflammatory response secondary to COVID-19 infection leads to thromboembolic complications at multiple levels.10 The aforementioned could lead to a micro-intestine perforation that could be the reason for the pneumoperitoneum in our case, but unfortunately, the progression of fibrinogen or D-dimer levels is not available for our patient to exclude this theory.
4 CONCLUSION
Pneumoperitoneum is a rare complication of COVID-19 infection, and it may occur during the management of critical cases, which could associate with other serious complications. Therefore, we recommend that physicians should take this complication into consideration in patients with COVID-19 in order to ensure rapid action to save the patient and prevent severe conditions.
AUTHOR CONTRIBUTIONS
All authors have participated in writing and reviewing the manuscript.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report. A copy of the written consent is available for review by the editor-in-chief of this journal.




