Design and evaluation of a prosthetic socket for a patient with diabetic-related transtibial amputation: A case report
Abstract
This is a report of a diabetic transtibial amputee with severe pain and ulcer in the antero-distal of the tibia. A novel prosthetic socket with an antero-distal silicone wall was designed. The result showed that the patient's satisfaction was increased and the average peak pressure was reduced by using the new socket design.
1 INTRODUCTION
Transtibial amputation (TTA) is the most prevalent amputation with a rate of 28% of all lower-limb amputees.1 Its successful surgery outcome depends on having a cylindrical shape of the residual limb, good padding of the distal tibia and also stable muscles.2 Interface pressure distribution between the residual limb and socket can affect an amputee's comfort, weight-bearing capability, and function during prosthetic use. Therefore, the prosthetic socket fit for individuals with insufficient residual limb soft tissue is challenging, and socket/residual limb interface pressure is important among this population.2
The patellar tendon bearing (PTB) and the total surface bearing (TSB) socket designs are the most common types for individuals with TTA. Using the TSB socket with silicon/gel liner, the socket/residual limb interface pressure could evenly be distributed across the residual limb compared with applying local pressure in certain parts of the PTB socket design.2 It has previously been observed that weight acceptance, gait symmetry, and balance can improve with the TSB socket.3 However, some authors found that satisfaction level is similar in both the TSB and the PTB sockets.4 The PTB socket design was developed based on applying pressure on the tolerant areas and relieving pressure on the intolerant areas.5 Some authors state that there is a significant pressure in the antero-distal of tibia of the PTB socket. However, others have found out that the PTB socket can decrease pressure on the distal intolerant parts of the residual limb and increase the amputees' comfort.5 The underlying factors leading to these findings have not been investigated yet.
Individuals undergoing amputation for diabetes usually have poor health condition, and their post-operative prosthetic rehabilitation is challenging. Manufacturing a well-fitted prosthesis may improve their health-related quality of life and mobility.6
This case report investigated whether changing the materials in the antero-distal end of the TSB socket can minimize pain and socket/residual limb interface pressure to increase socket-related satisfaction in an individual with major problems in the antero-distal end of the residual limb.
2 METHODS AND MATERIALS
2.1 Case report
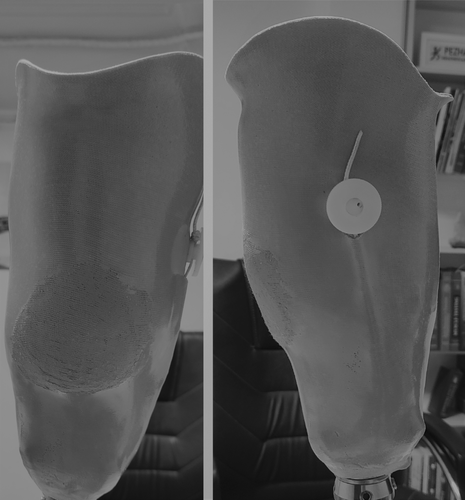
This case was a 58-year-old diabetic man with unilateral TTA who had been using prosthesis for 2 years. According to the Medicare Functional Classification Level,7 he had K3 level of activity. He had an unstable soft tissue in the residual limb with fluctuating edema. He used a TSB socket for ambulation. However, he had severe pain and sensitivity at the antero-distal end of his residual limb during gait. Therefore, he had severe limitation on the amputated leg while doing the routine daily activities. The patient also had a scar of healed ulcer and tenderness at the antero-distal of the tibia even when he was not wearing the socket (Figure 1). He had changed his socket, alternating between the PTB and TSB designs in the last 1.5 year due to the severe pain and multiple ulcers in the antero-distal part of his residual limb. The prosthetic components included a single-axis foot and a 6 mm thick gel liner with pin/lock suspension system.

2.2 Design consideration of the socket
A prosthetic socket positive cast mold was fabricated based on Ossur's transtibial hand casting and modification technique. Before casting, the gel liner was isolated by a single layer of plastic film to ensure all the areas of the liner were covered. The bony landmarks including the patella, fibula head, crest of tibia, and sensitive antero-distal of the tibia were marked. The circumference of the residual limb was recorded at 2 cm interval from the patellar tendon to the distal end.
The patient was asked to hold his knee in a relaxed extension. Then, we prepared a 4-ply of Plaster of Paris slab to embrace the distal sensitive area of the residual limb. After that, the plaster impression was conducted with a circumferential figure-of-8 manner. Because it needed to be total contact, the plaster was carefully smoothed across the residual limb to transfer pressure from the distal painful end and sensitive segments to the tolerant parts. The patellar tendon, pretibial muscles, medial flare of the tibia, lateral shaft of fibula, and the posterior compartment were considered the pressure tolerant parts.
A positive mold was prepared by filling the negative cast with liquid plaster that was dried afterward. After removing the negative cast from the positive model, we compared the measurements with the recorded measures and calculated the reduction percentage from the positive model. The volume of the proximal end was reduced by 3%–5%, focusing on the pressure tolerant parts.
A 10 mm polypropylene plastic socket was fitted for the patient to check its comfort and fit during gait. Afterward, the modified socket was prepared. A polyvinyl alcohol (PVA) bag was placed in front of the model. A layer of fabric was then placed in contact to the PVA bag. A thin layer of room temperature vulcanizing silicone rubber (shore 20) was applied on the antero-distal part of tibia (Figure 2). Then, we did the resin acrylic lamination. Novel prosthetic socket had a soft wall on the antero-distal portion and rigid walls on the other parts (Socket B) (Figure 3).

2.3 Data processing
To assess the prosthetic socket satisfaction, the patient was asked to fill out the Persian version of the Comprehensive Lower-limb Amputee Socket Survey (CLASS).8 This questionnaire consists of 15 items in four domains of stability, suspension, comfort, and appearance. In this questionnaire, the prosthetic socket fit was evaluated while the patient was sitting, walking, going up stairs, and wearing tight pants. Each item of CLASS consists of a 4-point Likert scale answer ranging from 1 to 4; (1 represents the least satisfaction and 4 represents the highest satisfaction). Each scale of CLASS has an individual total score from 0% to 100%.9 In this case report, the patient was asked to fill out the CLASS when using his previous prosthesis with the rigid wall (socket A) and 4 weeks after using the new prosthesis with socket B. The severity of the pain in the antero-distal part of the residual limb was also evaluated when the patient used socket A and after 4 weeks of using socket B by a 11-point numerical pain rating scale from 0 to 10 with 0 indicating no pain and 10 indicating severe pain.10
The interface pressure was calculated by force-sensitive resistance (FSR) sensor (No. 402, Interlink Electronics) that was located on the antero-distal end of the residual limb. The FSR was calibrated by applying a range of different values of force and measuring the corresponding values of resistances.11 The mean of peak pressure and the pressure distribution in the socket was calculated in two assessments in three standing positions of equal bilateral standing (50% of total weight on each leg) (position A), bilateral standing with the prosthesis side bearing 25% of the total weight (position B), and full weight bearing on the prosthetic side (position C).12
3 RESULTS
Using socket A, the patient's satisfaction in stability, suspension, and comfort domains of CLASS were 75%, 75%, and 62.5%, respectively. However, by using socket B, the patient's satisfaction in stability, suspension, and comfort increased up to 81.25%, 93.75%, and 100%, respectively. The appearance score was the same in both sockets (75%). The score of pain in the antero-distal of tibia was 8/10 while using socket A and 0/10 while using socket B.
In socket A with the pin/lock mechanism, the average peak pressure was 78.26, 36.89, and 81.91 N in positions A, B, and C, respectively. The average of peak pressure using socket B reduced to 77.45, 27.03, and 79.95 N in position A, position B, and position C, respectively.
4 DISCUSSION
We found that, compared with the conventional socket, it seems that using the soft silicon material in the antero-distal area of the tibia could decrease pain and socket/interface pressure and increase the overall satisfaction with the prosthetic socket.
A study on the importance of prosthetic socket fit in individuals with lower-limb amputation showed that the overall satisfaction of participants in stability, suspension, comfort, and appearance of the socket was 70.1%, 70.54%, 69.21%, and 58.13%, respectively.8 It is interesting to note that in all four domains of CLASS, the studied patient was more satisfied with socket B. Rouhani et al. showed that satisfaction was 69.21% with the socket comfort in 124 individuals with lower-limb amputation,8 a bit higher than that of our patient with socket A (62%). However, while using socket B, the level of comfort was 100%, showing a significant increase compared to socket A.
In a study with a different aim, Gholizadeh et al. stated that using the TSB socket with the Velcro suspension system can decrease the local pressure in the patellar tendon area and increase the pressure in the antero-distal part of the residual limb. In their study, the patient complained of severe pain in the patellar tendon area of the PTB socket. Therefore, the authors used a TSB socket with the Velcro suspension system to decrease the peak pressure at the patellar tendon and increase the pressure in the pressure tolerant area in the distal two third of the residual limb and distribute the load more uniformly over the stump.5 On the contrary, we tried to decrease the pressure in the antero-distal area of tibia by modifying the socket design and material. The results showed that the amputee can experience lower pressure in the antero-distal of his residual limb and its related pain using socket B. The most important clinically relevant finding was that using the TSB socket with silicon wall in the antero-distal part could reduce the local pressure in the patellar tendon area and the antero-distal of tibia. This finding is especially important for diabetic and vascular patients who have problems with wound sensation and healing abilities.
5 CONCLUSION
Using a socket with antero-distal silicone wall might be a better option for amputees with loss of the soft tissue in the bony prominence region of antero-distal tibia to control pain, increase comfort, and decrease interface pressure distribution compared with a rigid wall socket.
AUTHOR CONTRIBUTIONS
All authors involved in conceptualization, methodology, investigation, writing–original draft, and writing–review and editing. Mohammadali Mardani involved in resources and supervision.
ACKNOWLEDGEMENT
The authors thanks to Mohammad Hossein Mousavinasab and Alireza Khani to editing this text.
CONFLICT OF INTEREST
There is no conflict of interest.
ETHICAL APPROVAL
This study was supported by the Research Committee of University of Social Welfare and Rehabilitation Sciences (Letter No. IR.USWR.REC.1400.075). Tehran. Iran.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




