Counting gross fetal movement using a fetal movement acceleration measurement recorder in two fetuses with gastroschisis
Abstract
We used the fetal movement acceleration measurement recorder to count gross fetal movement in two fetuses with gastroschisis. In conclusion, both fetuses moved as much as normal fetuses, which suggested that normal fetal movement could indicate reassuring status also in fetuses with malformation when they have normal neurological developments.
1 INTRODUCTION
Gastroschisis is a congenital malformation with bowel herniation through a right-sided abdominal wall defect near umbilicus, and its prevalence has been increasing.1 The incidence of stillbirth is increased,2 but the long-term outcome for survivor is excellent in this malformation; therefore, the most important prenatal care is to ensure fetal reassuring status for avoiding fetal demise.
In current practices in gastroschisis management, the nonstress test and biophysical profile were used to assess a reassuring status.3 One of the biological profile scores is counting gross fetal movements; however, until now, it has been no report as to whether a fetus with gastroschisis moves as much as a healthy fetus.
We have developed a fetal movement acceleration measurement recorder (FMAM recorder, http://e-mother.co-site.jp) which enables the long-term recording of gross fetal movement at home.4, 5 This time, we had opportunities to use the FMAM recorder to count gross fetal movement in two fetuses with gastroschisis.
2 METHODS AND CASES
2.1 FMAM recorder
The FMAM recorder was explained in detail in our previous studies.4, 5 The weight is 290 g, and it can be used at home. It is composed of a recorder and two sensors. The sensor is disk-shaped, 20 g in weight, and 2.8 cm in diameter. It is handy, non-invasive, and can be used by most women comfortably although some women complained of slight contact dermatitis. One sensor is a fetal movement sensor that attaches to the mother's abdominal wall; the other is a mother's movement sensor that attaches to her thigh. The sensitivities of the fetal and maternal sensors are 700 mV/0.1G and 120 mV/0.1G, respectively. The fetal movement sensor picks up abdominal wall movement caused by fetal gross movement. The recorder is not suitable when a mother is active, so in principle, movement is recorded at night. Mothers do move occasionally during sleep, so only when the mother's movement sensor detects no movement of the leg, and the fetal movement sensor detects abdominal wall movement, gross fetal movement is judged to have occurred. In a previous study,4 we confirmed that agreement between gross fetal movement observed by ultrasonography and mother's abdominal oscillation sensed by FMAM recorder was almost perfect and the sensitivity and specificity were around 80%–85% and 90%–91%, respectively, after 28 gestational weeks.
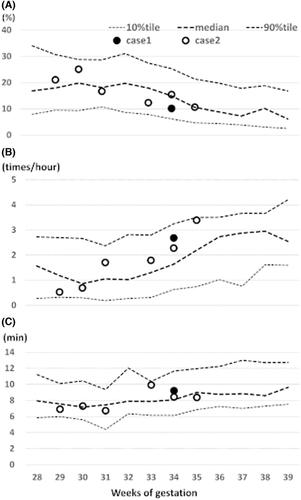
In this study, the ratio of the number of positive 10-second epochs to the total time for each night was calculated and defined as the movement ratio index. When a positive epoch did not appear for more than 5 min, this period was defined as a no-movement period. The mean frequency per hour and the mean duration of the no-movement periods were calculated for each night as no-movement indices. Normal reference values for these indices were made from 64 normal fetuses in our previous study.5
2.2 Case 1
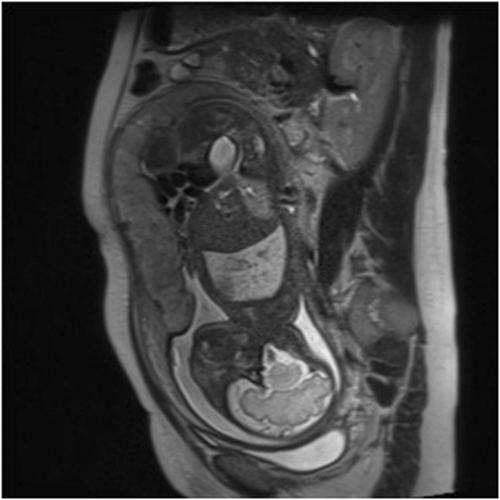
A 22-year-old woman, para 0, was referred to our hospital at 13 gestational weeks because an abnormal mass was found at the abdominal region of the fetus. She smoked 20 cigarettes per day before pregnancy. Ultrasonography revealed a protruding mass through the right side of the abdominal wall near the umbilicus. MRI revealed the same finding (Figure 1), and gastroschisis was diagnosed. Other anomalies were not found, and her pregnancy progressed uneventful after that.
After written informed consent was obtained, she recorded fetal movement once at home using the FMAM recorder at 34 weeks. She underwent fetal heart rate monitoring every time she visited the hospital, which showed reassuring status.
The incidence of sudden fetal death is known to increase for gastroschisis, and she underwent a Cesarean section at 36 weeks and 2 days and delivered a 2223 g male baby. Apgar scores were 8/9, and the pH of the umbilical artery was 7.389. No other abnormalities were found. The newborn underwent silo plasty on 0 day and abdominal repair on Day 12.
2.3 Case 2
A 22-year-old woman, para 0, was referred to our hospital at 18 gestational weeks because of a suspicion of fetal gastroschisis. She smoked before pregnancy but did not after conception. Gastroschisis was diagnosed by ultrasonography. Fetal growth restriction was found after 27 weeks. The woman came to our hospital weekly, and the fetal heart rate showed a reassuring pattern at every visit.
After written informed consent was obtained, she was very cooperative and recorded fetal movement weekly after 27 weeks at home using the FMAM recorder.
Cesarean delivery was planned at 37 weeks, but uterine contraction increased at 36 weeks, and she was admitted to our hospital. Fetal heart rate monitoring revealed no deceleration but decreased variability, and she underwent an emergency Cesarean section and delivered a 1878 g male baby. Apgar scores were 3/4, and the umbilical artery pH was 7.321. No other abnormalities were found. The newborn underwent silo plasty on 0 day and abdominal repair on Day 10.
3 RESULTS
3.1 Case 1
Fetal movement was recorded for 380.2 min. The movement ratio index was 10.15%, and the no-movement indices, such as the mean frequency and mean duration, were 2.68 times per hour and 9.21 min, respectively. The indices were plotted over the normal reference values (4), and all indices were found to be within the normal range (Figure 2).
3.2 Case 2
Fetal movements were recorded 6 times. The mean (SD) recording time was 435.6 (61.4) minutes. The movement ratio indices were 21.05, 25.09, 16.7, 12.34, 15.44, and 10.64% for 29, 30, 31, 33, 34, and 35 gestational weeks, respectively. The mean no-movement frequencies were 0.52, 0.69, 1.70, 1.79, 2.27, and 3.39 times per hour, and the mean no-movement durations were 6.91, 7.31, 6.72, 9.92, 8.43, and 8.38 min for the same gestational weeks. All indices were within normal range (Figure 2).
4 DISCUSSION
We have shown that two fetuses with gastroschisis moved as much as normal fetuses. This means that normal fetal movement could indicate reassuring status also in a fetus with gastroschisis.
Some parents of a fetus with gastroschisis ask whether or not their baby feels abdominal pain in utero and that could be important for them in deciding whether to continue or terminate the pregnancy. There are consistent evidence that normal fetuses are capable of feeling pain in the third trimester.6 Regrettably, however, no one knows whether a baby with gastroschisis feels pain or not; however, at least, we recognize now that there were two fetuses with gastroschisis who neither increased nor decreased their gross movement because of abdominal pain.
Other than well-being, fetal movement is supposed to reflect neurological developments; however, little of it has been proved actually until today. One reason is that there was no practical way to count fetal movement for long hours. We are now collecting fetal movement data with the newly developed FMAM recorder. This time, we got an opportunity to obtain fetal movement data of two fetuses with gastroschisis. We thought that counting fetal movement of gastroschisis was interesting to see whether fetal movement reflects neurological development because gastroschisis is a serious condition, but extraintestinal anomalies are rarely associated and survivors of gastroschisis generally show good neurological prognosis. Normal gross movement in these two cases seemed to support that fetal movement reflect neurological developments.
In general, little is known about the movement of fetuses with congenital malformations. Does fetal movement also indicate reassuring status in fetuses with congenital malformations? The two cases in this report suggested that fetal movement reflects reassuring status also in cases of congenital malformation when they have normal neurological developments; however, when they have abnormal neurological developments, there are little studies to answer the question. Further studies are needed in this area.
In conclusion, two fetuses with gastroschisis moved as much as normal fetuses, which suggested that normal fetal movement could indicate reassuring status also in fetuses with malformation when they have normal neurological developments.
AUTHOR CONTRIBUTIONS
ER wrote the report. KY collected the data. HK analyzed the data. KN supported the work.
ACKNOWLEDGMENTS
We thank emeritus professor Takuya Ayabe and Mrs. Mieko Fuse, and we appreciate language help by Mr. Howard Stacey. We also appreciate the cooperation of the women who participated in this study.
FUNDING INFORMATION
This study was supported by JSPS (16K10109).
CONFLICT OF INTEREST
The authors have no conflicts of interest relevant to this article.
ETHICAL APPROVAL
This study was approved by the ethical committee of Teikyo University.
CONSENT
Written informed consents were obtained from the patients to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
None.




