Simultaneous occurrence of subarachnoid hemorrhage and cerebral venous sinus thrombosis: A systematic review of cases
All authors contributed equally to the paper.
Abstract
Although the leading causes of subarachnoid hemorrhage (SAH) are aneurysm rupture and arteriovenous malformations, cerebral venous sinus thrombosis (CVST) can, in rare cases, be associated with SAH. This phenomenon is an uncommon presentation, with less than a hundred cases reported based on our review of the literature. The purpose of this review is to highlight what is known regarding these cases, how they are managed and to highlight the need for further studies that will serve as a basis for the development of a standard management guideline across board. The following databases were searched: PubMed and Ovid Embase. A complementary search of Google Scholar and AJOL was done. Gray literature search was also conducted on the Google search engine for any additional relevant papers. We were able to extract data regarding 33 cases from 29 identified studies. The mean age was 46.6 ± 14.08. 17 (51.5%) of the cases were female, and the female-to-male ratio is 1.1:1. Headache was by far the commonest symptom, occurring in 82% of cases followed by seizures in 42% of cases. Four patients (12%) had loss of consciousness while 5 patients (15%) had some form of focal neurologic deficit. Twenty patients had cerebral venous sinus thrombosis in at least two different sinuses. The superior sagittal sinus was the most common location for CVSTs (79%), followed by the transverse sinus (57.5%). Twenty-nine cases (89%) were managed with anticoagulation alone and one case had a mechanical thrombectomy. We have performed a comprehensive review of cases that had the simultaneous occurrence of SAH and CVST and have identified their peculiarities and the challenges to management. Further research is needed in order to identify a causal relationship and to serve as a basis for the development of a standard management guideline across the board.
1 INTRODUCTION
Although the leading causes of subarachnoid hemorrhage (SAH) are aneurysm rupture and arteriovenous malformations, cerebral venous sinus thrombosis (CVST) can, in rare cases, be associated with SAH.1 This phenomenon is an uncommon presentation, with less than a hundred cases reported based on our review of the literature. CVST itself typically presents with headache, nausea, vomiting, weakness, loss of vision, and seizure.2 Because of its rarity, a high index of suspicion is important in making the diagnosis.3
CVST accounts for 1% of all strokes4, 5 and has a mortality as high as 30% with the annual incidence ranging from 0.22 to 1.57 per 100,000. It is more common in women than men.6, 7 Multiple reversible and irreversible factors are associated with CVST and include surgery, thrombophilia, antiphospholipid syndrome, cancer, inflammatory bowel disease, use of the oral contraceptive pill, infection, and pregnancy.8
The reason why SAH might occur together with CVST is still debated. In some cases, they could be coincidental. However, there are many hypotheses with regards a causal relationship between the two entities; hence, there is a need to review all the cases in the existing literature to see the similarities and differences across these rare cases and presentations. The purpose of this review is to highlight what is known regarding these cases, how they are managed and to highlight the need for further studies that will serve as a basis for the development of a standard management guideline across board. In this article, we systematically reviewed all such published cases of CVST and SAH occurring concurrently, noting their common characteristics, imaging findings, treatment, and outcomes.
2 METHOD AND MATERIALS
2.1 Source of information and search
We followed the PRISMA guidelines for conducting systematic reviews. To identify potentially relevant papers, the following databases were searched: PubMed and Ovid Embase. A complementary search of Google Scholar and African Journal Online (AJOL) was done. Gray literature search was also conducted on the Google search engine for any additional relevant papers. The results were exported into an excel document and duplicates were removed. The search strategy is presented in Table A1 in Appendix 1.
2.2 Selection criteria
We identified cases where SAH and CVST occurred together. We included case reports and case series, which included the aforementioned. We excluded posters, abstract-only papers, reviews, meta-analyses, commentaries, and letters to the editor. We excluded articles that were not written in the English language.
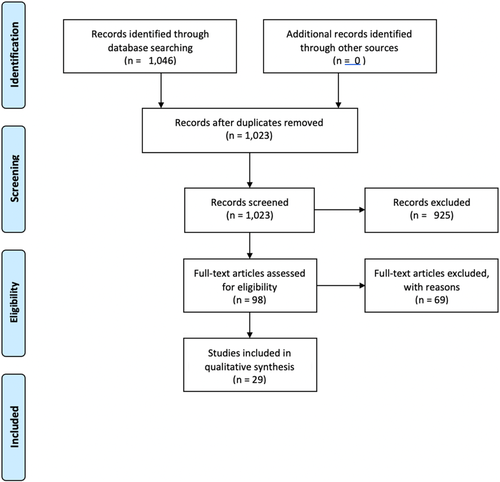
2.3 Selection of sources of evidence
Three reviewers working independently evaluated the titles, abstracts, and then full text of all cases identified by our searches for relevant papers. We resolved disagreements on study selection and data extraction by consensus where necessary. The process is summarized in Figure 1.
2.4 Data extraction
A data-charting form was jointly developed by the three authors to determine which data to extract. The reviewers then read each article extensively and populated the data extraction form with relevant details. The authors continually discussed the results and continuously updated the data-charting form in an iterative process. We extracted data on the characteristics of each patient/case (Age, gender, symptoms at presentation and their duration), diagnostic modalities for the subarachnoid hemorrhage and CVST, the location of the SAH and CVSTs, possible etiology (presence of aneurysms, trauma, coagulation disorders), the treatment modalities and the outcomes. We were able to extract data regarding 33 cases from 29 identified studies. A summary of the case studies is seen in Table A2 in Appendix 1.
2.5 Investigated patient characteristics
The mean age was 46.6 ± 14.08. 17 (51.5%) of the cases were female, and the female-to-male ratio was 1.1:1. One case had hyperhomocysteinemia while another had C667T mutations (Heterozygous for methylenetetrahydrofolate reductase). Only one case had a recent use of antiplatelets (Clopidogrel) prior to the diagnosis of CSVT and SAH.
2.6 Clinical symptoms and Imaging
Headache was by far the commonest symptom, occurring in 82% of cases followed by seizures in 42% of cases. Four patients (12%) had loss of consciousness while 5 patients (15%) had some form of focal neurologic deficit. Other symptoms included dizziness, nausea, vomiting, gait disturbance and ataxia. The diagnostic modalities used included a non-contrast computed tomography (CT) scan, computed tomography angiography (CTA), computed tomography venography (CTV), magnetic resonance imaging (MRI), magnetic resonance venography (MRV), and digital subtraction angiography (DSA). Twenty-five (75.7%) of the studies had an MRI done, while only 17 (51.5%) of them had a further MRV done to confirm the venous thrombosis. Twenty-seven of the cases had a non-contrast CT scan done which showed evidence of subarachnoid hemorrhage. Four patients later had a CTA, while another three had a magnetic resonance angiography (MRA) done to exclude an aneurysmal cause. Only one patient had a CTV done.
2.7 Diagnosis, treatment, and outcomes
Twenty patients (60.6%) had cerebral venous sinus thrombosis in at least two different sinuses. Of the different locations for the CVSTs, the superior sagittal sinus was the most common location (79%), followed by the transverse sinus (57.5%). Only one case of CVST and SAH had an accompanying intracerebral hemorrhage (ICH). The locations of the subarachnoid hemorrhage were more diverse, ranging from the perimesencephalic areas and cerebral convexities to the Sylvian fissures and interhemispheric fissures. Twenty-five of them involved the cerebral convexities while 7 of them involved the subarachnoid cisterns. Most of the subarachnoid hemorrhages were non-aneurysmal. Only one patient had an aneurysmal rupture; the location of the aneurysm was in the anterior communicating artery. Twenty-nine cases (89%) were managed with anticoagulation alone and one case had a mechanical thrombectomy first prior to anticoagulation. One case was managed with dehydration, scavenging free radicals, and nerve protective therapy, while another was managed with hydration and osmotic diuresis (with an eventual decompressive craniectomy for persistent raised ICP). The only case of the aneurysm was managed with coil embolization. All 28 cases that discussed the status at discharge and a few weeks after reported different ranges of improvement; recovery ranged from improvement in symptoms and partial recanalization to full recovery and full recanalization of the vessels.
3 DISCUSSION
Subarachnoid hemorrhage should be considered in the event of a sudden worsening headache.9 The diagnostic modality of choice for subarachnoid hemorrhage in the initial stages is a non-contrast CT scan.9, 10 With an equivocal result, a lumbar puncture is advised; however, given the increased sensitivity of a non-contrast CT scan within the six-hour timeframe, the choice to undertake a lumbar puncture should be through a shared decision-making process.9 As aneurysms are a common cause of SAH, CTA scans are important in demonstrating a causative aneurysm.9 A non-contrast CT scan is also a useful diagnostic modality for diagnosing a CVST as it can show findings that include, but are not limited to, venous sinus or deep vein hyper-density.11, 12 CT venography and/or MR venography are recommended diagnostic modalities of choice, as recommended by the European Stroke Organization.13
Transverse sinuses, superior sagittal sinuses, and the sigmoid sinus are the most common sites of CVSTs, and in most cases, multiple sinuses are affected.14-16 This is consistent with the findings of our review study, which showed that multiple sinuses were frequently affected with the superior sagittal sinus and the transverse sinus being the commonest sites. In cases with a coexisting cerebral venous sinus thrombosis, the perimesencephalic region is a common location for non-aneurysmal SAH.17, 18 The most common locations for aneurysms are in the circle of Willis, particularly the anterior communicating artery and the internal carotid artery.19, 20
A third of CVST cases might present with intracerebral hemorrhage.21 However, there is a paucity of literature on how common it is for CVST to occur with subarachnoid hemorrhage. One hypothesis of why SAH may occur simultaneously with CVST is that the blood from the ensuing hemorrhagic infarct (resulting from the venous thrombosis) may extend into the subarachnoid space.22 This may certainly be the case in some of our findings where there was parenchymal hemorrhage besides the presence of CVST and SAH; however, its absence (also seen in many of the cases identified) may suggest a more direct causal relationship. A leading hypothesis supporting this stipulates that when CVST occurs, the ensuing secondary venous hypertension could be transmitted to the cortical veins, leading to the dilation and rupture of the fragile thin-walled cortical veins in the subarachnoid space.17, 23 Sometimes, the occurrence of both entities together could be coincidental, as seen in instances with an aneurysmal cause of the SAH, like in some of the identified cases.
Regardless of etiology, the treatment of a patient with SAH and CVST occurring concurrently can pose a dilemma. The risk of rebleeding in SAH is high, and in the absence of immediate surgical intervention for aneurysmal SAH, antifibrinolytics have been advised.24 This is in sharp contrast to the standard treatment of CVSTs, which involves rapid anticoagulation and the stoppage of any prothrombotic medications.11 Using systemic anticoagulation where simultaneous subarachnoid hemorrhage exists might worsen the hemorrhage. In cases of simultaneous CVST and ICH, endovascular interventional therapy has been beneficial.25 There is a possibility that such interventions may also yield positive results when used in cases of CVST occurring with SAH. Interestingly, in our study, despite the SAH, most of the patients were treated with anticoagulant therapy with good outcomes reported. Despite our comprehensive review, this study was not without limitations. Because we excluded articles that were not in the English Language, we could have potentially missed relevant literature. There was also heterogeneity in the way the case reports were reported which meant some relevant data could have been missed. Regardless, this review will contribute to the growing body of work on this occurrence.
4 CONCLUSION
We have performed a comprehensive review of cases that had the simultaneous occurrence of SAH and CVST and have identified their peculiarities and the challenges to management. Further research is needed in order to identify a causal relationship and to serve as a basis for the development of a standard management guideline across the board.
AUTHOR CONTRIBUTIONS
D.J involved in conceptualization, methodology, software, validation, formal analysis, investigation, resources, data collection, data curation, writing—original draft, writing—review and editing, project administration, supervision, submission, and correspondence. O.O and T.M involved in conceptualization, methodology, software, validation, formal analysis, investigation, resources, data collection, data curation, writing—original draft, writing—review and editing.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST
The authors hereby declare that there are no competing interests.
CONSENT
As this was a review of cases in already literature, no individual consent was required. Consent was however obtained by the individual case reports used in this review in accordance with the journal's patient consent policy.
APPENDIX 1
| MeSH/Keywords | Database | Time span | Hits |
|---|---|---|---|
| (“subarachnoid haemorrhage”[All Fields] OR “subarachnoid hemorrhage”[MeSH Terms] OR (“subarachnoid”[All Fields] AND “hemorrhage”[All Fields]) OR “subarachnoid hemorrhage”[All Fields]) AND ((“cerebrally”[All Fields] OR “cerebrum”[MeSH Terms] OR “cerebrum”[All Fields] OR “cerebral”[All Fields] OR “brain”[MeSH Terms] OR “brain”[All Fields]) AND (“venous thrombosis”[MeSH Terms] OR (“venous”[All Fields] AND “thrombosis”[All Fields]) OR “venous thrombosis”[All Fields])) | PubMed | Inception - April 07 | 381 |
| cerebral venous sinus thrombosis.mp. or cerebral sinus thrombosis/ AND subarachnoid hemorrhage.mp. or subarachnoid hemorrhage/ | OVID Embase | 1974 to 2022 April 07 | 665 |
| Case | Author (Year) | Age/Sex | Symptoms (duration) | Imaging | Location of Subarachnoid hemorrhage | Location of CVST | Anticoagulant use/Hypercoagulability | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Gajurel BP et al (2021) | 58F | Holocephalic headache with seizure on presentation (3 days) | CTH, MRV, CTA | Insular, perimesencephalic, ambient and suprasellar cisterns, | Left Transverse Sinus | None/NT | LMWH, Levetiracetam and 3% Hypertonic Saline | Home on dabigatran 150 mg twice daily; stable on follow-up |
| 2 | Syed K et al (2021) | 48 M | Seizure and Altered Mental State (ND) | CTH, MRI, DSA | Bifrontal | Superior Sagittal Sinus | None/ND | IV esmolol 50 mcg/kg/min infusion and nimodipine 60 mg Q4 hourly; levetiracetam 500 mg, then intravenous heparin and later transitioned to coumadin after CVT dx | Treated and discharged with no neurological sequelae |
| 3 | Kumar H et al (2021) | 25F | SOH, Confusion, LOC (2 days) | MRI, MRV | ND (review image) | Right Transverse Sinus | None/−ve | Half dosage LMWH (60 mg subcutaneously once a day); Then full dose; Then warfarin | Thrombosis resolved within 6 weeks |
| 4 | Sun J et al (2018) | 57F | Dizziness; N&V (ND) | CTH, MRA, MRV | Partial gutter of the right frontal, parietal, and occipital lobes | Superior and Inferior sagittal sinus | None/−ve | Dehydration, scavenging free radicals, and nerve protection therapy | 18-month follow-up: no recurrent thrombosis, improvement of non-fluent aphasia, right limb muscle strength was slightly worse than normal. |
| 5 | Amer RR et al (2018) | 44F | SOH (ND) | CTA, MRA, MRv | Prepontine cistern | Left Transverse and sigmoid sinus | None/−ve |
LMWH (Nadroparin, 6150AXaIU, subcutaneous injection, twice daily) in combination with intravenous warfarin 3 mg/day |
ND |
| 6 | Abbas A et al (2018) | 58 M | LOC secondary to diarrhea and vomiting (ND) | CTH, CTV | Left temporal and parietal lobes | Superior sagittal sinus and straight sinus | None/−ve | LMWH and Rivaroxoban | ND |
| 7 | Liu Y et al (2017) | 35F | LOC and Seizures (5 days) | CTH, CTA, DSA | Right temporal lobe | Superior sagittal sinus and bilateral transverse sinus | None/ND | Mechanical thrombectomy; Catheter with Urokinase infiltration; LMWH, then anticoagulant | ND |
| 8 | Fu FW et al (2017) | 45 M | Occipital headaches, N&V (6 hours) | CTH, CTA, DSA, MRI | Perimesencephalic and prepontine cisterns | Right Transverse Sinus | None/−ve | LMWH (Nadroparin, 6150AXaIU, subcutaneous injection, twice daily), warfarin 14 days later | Improvement of symptoms 10 days post-treatment, complete absorption of hemorrhage at day 16, no neurologic deficit at 3 weeks |
| 9 | Uniyal R et al (2017) | 38 M | Holocranial headache; Vomiting; R arm weakness (ND) | CTH, MRI, MRA, MRV | Left central sulcus | Superior sagittal sinus | None/ND | LMWH followed by oral anticoagulation | Recovered completely in 7–10 days |
| 10 | Unal Ay et al (2016) | 78 M | Sudden-onset thunderclap headache, Stroke (ND) | CTH, CTH Contrast, MRV | Suprasellar cistern | Transverse sinus, Bilateral Sigmoid Sinus, Superior Sagittal Sinus | Clopidogrel/−ve | Heparin infusion | Symptom relief in two weeks |
| 11 | Neubauer C et al (2016) | 63F | Headache (3 weeks) | CT, MRI, CTA | Left MCA/ACA territories | Superior sagittal and right lateral dural sinus | None/−ve | Heparin followed by oral anticoagulation; Coil embolization, and smasmolytic | Six months follow-up revealed complete aneurysm occlusion and progressive recanalization of CVT |
| 12 | Anderson B et al (2015) | 42 M | Uncontrolled Jerking; Dysesthesia; LOC (ND) | CT, CTA, MRI, MRV | Right frontotemporal convexities | Superior sagittal sinus, right transverse, and sigmoid sinus | None/−ve | Heparin then coumadin therapy | MRI at 2 weeks - SAH resolved; MRI 4 months - partial recanalization of the dural sinuses |
| 13 | Hassan Aet al (2015) | 46 M | Headache; Right-sided Weakness; Focal seizures (3 days) | CTH, MRV, CTA | Paramedian sulci (Bilateral) | Superior sagittal sinus, transverse sinus and sigmoid sinus | None/−ve | Subcutaneous anticoagulation then Oral anticoagulation for 6 months | Headache resolved over 1 week; Neurological symptoms over 4 weeks; Seizure free; Maintained on anti-epileptic drugs |
| 14 | Hassan A et al (2015) | 35 M | Headache; Seizure (2 days) | CTH, MRI, MRV | Bilateral, predominantly over the left frontoparietal sulci | Superior Sagittal Sinus | None/−ve | Dose-adjusted intravenous anticoagulation and then Oral anticoagulation | Symptoms improved; Lost to follow-up at 4 months |
| 15 | Arévalo-Lorido et al (2015) | 70 M | Progressive Occipital Headache and nausea (ND) | CTH, MRI, MRA | Right Parietal region | Right Transverse Sinus | None/Heterozygote for methylenetetrahydrofolate reductase C667T mutations; rest negative | 60 mg LMH to 120 mg and then oral Anticoagulation | ND |
| 16 | Sahin N et al (2014) | 48F | Headache; gait disturbance (7 days) | MRI, MRV | sulci of the bilateral frontoparietal convexity | Superior sagittal sinus | None/ND | Anticoagulation | Improved |
| 17 | Yamamoto et al (2013) | 32F | Head dullness; 9 days later headache and then seizure (ND) | CTH, MRI | Basal cisterns, bilateral sylvian fissures, and anterior interhemispheric fissure | Superior sagittal sinus, straight sinus, right transverse sinus | None/−ve | Hydration | Discharged with only a slight visual field defect in the right eye and returned to her previous occupation |
| 18 | Sayadnasiri M et al (2012) | 42F | Headache, Vomiting, FND, Seizures (3 days) | CTH, MRI, MRV | Right parietal area | Cerebral Dural Sinuses | None/−ve | Anticoagulation | ND |
| 19 | Sayadnasiri M et al (2012) | 36 M | Headache, FND, Seizures (3 weeks) | CTH, MRI, MRV | Right Sylvian fissure | Right lateral and sigmoid sinuses and also superior sagittal sinus | ND/−ve | Anticoagulation | Discharged with partial recovery 2 weeks later. |
| 20 | Kato et al (2010) | 52F | Progressive occipital headache, nausea, and vomiting; generalized seizures 4 days into admission (ND) | Cerebral Angiography, CTH | Right temporal sulcus and bilateral cerebellar sulci | Superior sagittal sinus, straight sinus, transverse sinus, and right sigmoid sinus | None/−ve | IV heparin and then Warfarin | Near-complete neurological recovery within a month. |
| 21 | Sharma et al (2010) | 59 M | Rapidly progressive and pulsatile headache then generalized seizures (ND) | MRI, MRV | right parasagittal high frontoparietal areas | Superior sagittal sinus and bilateral transverse sinus | None/−ve | Subcutaneous LMWH and then oral warfarin | Clinically satisfactory within six weeks |
| 22 | Lai NK et al (2008) | 34 M | Headache, Seizure (3 days) | CTH, DSA | Right frontoparietal sulci | Superior sagittal sinus | None/−ve | Intravenous heparin, then warfarin, and anticonvulsants | MRI at 3 months demonstrated partial recanalization of the superior sagittal sinus. |
| 23 | Jaiser et al (2008) | 53F | Spontaneous, sudden-onset occipital headache + mild neck stiffness (3 days) | CTH, CTA, MRV | Left frontal | Superior sagittal sinus | None/−ve | IV unfractionated heparin, then warfarin under LMWH cover | Recanalization of superior sagittal sinus after 6 months |
| 24 | Ko YP et al (2007) | 25F | Headache, FND (3 days) | CTH, MRI, MRV | Left frontal | Superior sagittal sinus | None/−ve | LMWH, then warfarin | Symptoms improved within a few days |
| 25 | Lin et al (2006) | 44 M | 1 episode of focal motor seizure of left arm; Thunderclap headache (ND) | CTH, CTA, MRI | Right parietal sulci | Superior sagittal sinus, transverse sinus | None/−ve | IV heparin and then Warfarin | L arm weakness resolved |
| 26 | Rice H et al (2006) | 56F | Headache, neck stiffness, photophobia (ND) | MRI, MRV | Several cortical sulci along the right frontoparietal convexity | SSS, left transverse sinus, Dural sinus | None/ND | Anticoagulation | Clinical improvement within 1 week; Radiological improvement at 3 months |
| 27 | Shukla et al (2006) | 40 M | Sudden headache associated with recurrent vomiting, photophobia and phonophobia + right focal seizures followed by R hemiparesis (ND) | CTH, DSA, MRV | Left sylvian fissure | Superior sagittal, transverse sinuses, inferior sagittal sinus | None/−ve | LMWH, then warfarin | Symptom-free at discharge |
| 28 | Adaletli I et al (2005) | 14 M | Headache, nausea, vomiting, diplopia, and gait disturbance (ND) | CTH, DSA | Basal cisterns, bilateral sylvian fissures, anterior hemispheric fissure | SSS, galenic vein, straight sinus | None/ND | Anticoagulation | Symptoms and signs completely resolved |
| 29 | Oppenheim et al (2005) | 69 M | Sudden-onset headache (ND) | MRI + DSA | subarachnoid spaces of the right frontal convexity | Transverse and sagittal sinuses | Previous history of DVT | IV Heparin | Complete radiologic and clinical recovery at follow-up |
| 30 | Oppenheim et al (2005) | 55F | Headache, neck stiffness, nausea, seizure (ND) | CTH, MRI, DSA | bihemispheric; predominantly in the left insular sulci | sagittal and the left transverse sinus | None/−ve | LMWH | rapid clinical improvement and partial recanalization of the thrombosed sinus |
| 31 | Oppenheim et al (2005) | 32F | partial seizure that was secondarily generalized. Headaches with a sudden-onset with vomiting (3 weeks) | CTH, MRI, DSA | diffuse SAH predominating in the anterior interhemispheric sulci | sagittal and right transverse venous sinuses | hyperhomocystinemia | IV Heparin | complete regression of her neurologic signs and headaches |
| 32 | Oppenheim et al (2005) | 51F | severe headaches associated with focal neurologic symptoms (5 weeks) | CTH, MRI | diffuse bilateral acute SAH, sparing the basal cisterns | Superior sagittal sinus | prophylactic anticoagulant (not specified) for 2 months post ankle surgery | Anticoagulation | Rapid clinical and radiologic improvement |
| 33 | Sztajzel et al (2001) | 58F | Severe headache of sudden-onset (1 day) | CTH, CTA, MRI, MRA | Right cerebellar region | Right lateral sinus; right transverse/sigmoid sinus | Previous history of DVT | ND | Resolution of symptoms after 4 weeks |
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




