SARS-CoV-2 infection with bilateral intralabyrinthine hemorrhage
Abstract
A 47-year-old woman presented with the complaint of sudden hearing loss associated with vertigo. Serological testing was positive for IgM and negative for IgG COVID-19 antibodies, with no other associated factors. Magnetic resonance imaging of the brain showed bilateral intralabyrinthine hemorrhage.
1 INTRODUCTION
The World Health Organization declared the coronavirus disease 2019 (COVID-19), a pandemic in March 2020. In the following months, the virus spread rapidly around the world. The disease can be asymptomatic or vary from mild to very severe symptoms. In general, studies of COVID-19 symptoms report fatigue, cough, headache, fever, myalgia, arthralgia, and diarrhea. The most common otolaryngological symptoms are anosmia (38.2%) and dysgeusia (36.6%).1 Some reports in the literature indicate an association between severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and hearing loss; however, in many cases, patients have been in intensive care for a long time and receiving ototoxic drugs.2, 3 Chari et al.4 in a study conducted in a tertiary referral hospital in the United States, compared 2 time periods (before and during the pandemic) and found no proportional increase in cases of sudden hearing loss during the peak of the COVID-19 pandemic. As the virus has been known for less than 2 years, the mechanisms underlying its pathogenesis remain unclear, despite the efforts of the scientific community worldwide.
2 CASE REPORT
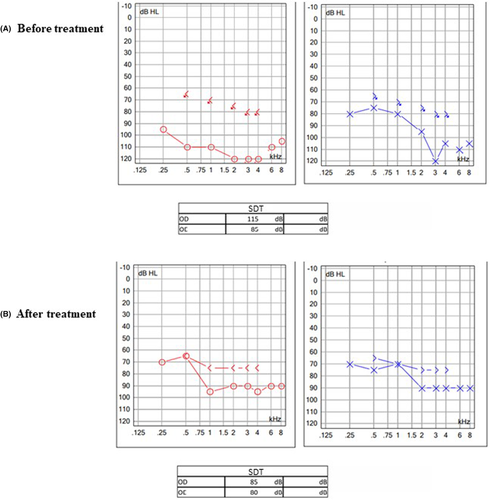
A 47-year-old woman presented with the complaint of sudden hearing loss associated with vertigo, which started 2 days before her initial visit. She reported a condition of runny nose and sneezing 10 days before the onset of symptoms, without fever, hyposmia, dysgeusia, or dyspnea. She denied previous auditory or vestibular symptoms. Family history was negative for hearing loss or vertigo. She was not taking any medications and had no allergies. Otoscopy was normal. Horizontal nystagmus was present, and she had a positive Romberg test. Audiometric testing showed profound sensorineural hearing loss (SNHL) in the right ear and severe to profound SNHL in the left ear (Figure 1). Treatment was initiated with prednisolone 80 mg/day, tapered by 20 mg every 3 days for a total duration of 15 days. The patient received an intratympanic injection of dexamethasone (2 mg) in each ear. We ordered laboratory tests and magnetic resonance imaging (MRI) of the brain.
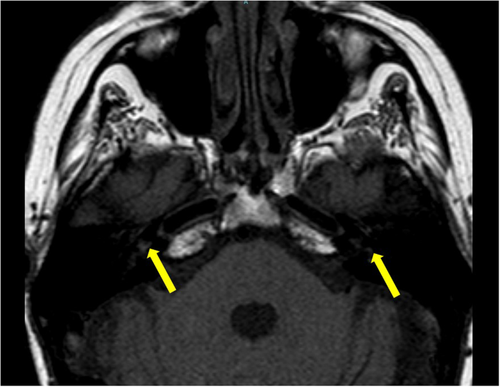
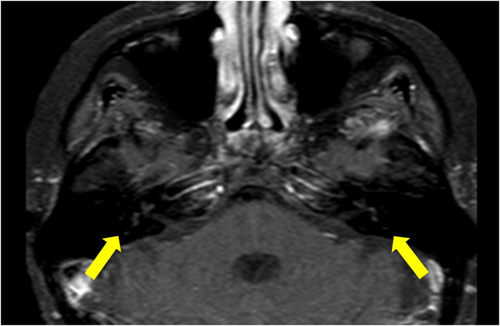
Serological testing was positive for IgM and negative for IgG COVID-19 antibodies. MRI images demonstrated signal abnormality on T1-weighted sequences showing blood components in the cochleae, semicircular canals, and bilateral vestibule, suggesting intralabyrinthine hemorrhage (ILH), with persistent high signal on post-contrast images (Figures 2 and 3).
The patient did not show significant hearing improvement with treatment (Figure 1B) after 30 days of follow-up. She showed complete resolution of her vertigo symptoms. The patient used hearing aids, but with the poor audiological result, cochlear implant surgery was indicated.
3 DISCUSSION
Several pathologies are associated with sudden hearing loss: infections, vascular disease (hemorrhage or ischemia), immune-mediated diseases, neurological diseases, neoplasms, and ototoxicity. ILH has been described in patients with aplastic anemia, sickle cell disease, endolymphatic sac tumor, systemic lupus erythematosus, and leukemia, as well as secondary to head trauma, use of anticoagulants, after surgery for vestibular schwannomas, and reported in a patient with COVID-19. The patient reported here had mild COVID-19 symptoms. Both were not hospitalized or treated with anticoagulants. Therefore, SARS-CoV-2 infection is the most likely factor associated with hearing loss.
ILH is often unilateral and sudden or rapidly progressive. Lee et al5 compared 2 groups of patients with idiopathic SNHL with and without ILH and found a quantitative difference in hearing impairment between the ILH and non-ILH groups (94.09 vs. 66.66 dB). Hearing recovery over 2 months was significantly worse in the ILH group (p = 0.014). The symptom of dizziness was more common (92%) in patients with ILH. Patients with both SNHL and ILH had a worse prognosis than patients with idiopathic SNHL. Our patient had minimal hearing improvement despite treatment with corticosteroids, thus confirming a poor hearing prognosis.
Some mechanisms may explain the presence of hemorrhage in patients with COVID-19. SARS-CoV-2 has been reported to bind to angiotensin-converting enzyme 2 (ACE2) receptors, which are largely present in the brain vessels and could cause endothelial damage and disruption. Endothelial cell infection has been demonstrated in COVID-19 by histological identification of viral elements within endothelial cells, accumulation of inflammatory cells, and apoptosis.6 These mechanisms may explain more severe symptoms, such as stroke. However, it is still difficult to explain a localized bleeding without any other neurological impairment, as presented by the two patients reported so far.
MRI is used to evaluate patients with SNHL, although a distinct pathology can only be identified in 10% of patients. On MRI, high signal intensity on T1-weighted sequences may, in theory, result from fat, protein, or blood. Perilymph and endolymph are usually isointense to cerebrospinal fluid on all MRI sequences. On MRI, ILH is characterized by high signal intensity on T1-weighted sequences (Figure 2), but without enhancement after gadolinium injection (Figure 3). Plain T2-weighted images are not useful because signal intensity may vary. On MRI, intralabyrinthine schwannomas differ from ILH by a signal intensity enhancement after intravenous injection of contrast medium (gadolinium).
There is a similar report in the literature, described by Chern et al.7 of a case of bilateral sudden SNHL and ILH in a patient with positive IgG serological testing performed several weeks after onset of symptoms. In the case reported here, serological testing was positive for IgM and negative for IgG COVID-19 antibodies, indicating a recent COVID-19 infection. Thus, SARS-CoV-2 infection is the most likely factor responsible for the hearing loss in the case reported here. Another similarity between the cases is the poor prognosis of patients and poor response to corticosteroids.
4 CONCLUSION
Much remains to be learned about the histopathological mechanisms of COVID-19 infection. Despite some evidence that the virus may cause hearing loss, only a histological analysis of the cochlea could confirm c as the causative agent of this condition. Future studies may confirm or refute these hypotheses.
AUTHOR CONTRIBUTIONS
Drs. Vagner Antonio Rodrigues da Silva and Joel Lavinsky drafted the manuscript and acquired, analyzed, and interpreted the data. Drs André Pinto Villarim; Monine Couto Farias Bem; and Mauro Caldas Mendes Filho drafted the manuscript and revised it critically for important intellectual content, provided final approval of the final draft. Drs. Thiago Bezerra Arthur Menino Castilho contributed substantially to the study design and approved the final draft.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable.




