An incidental finding of unroofed coronary sinus during angiography confirmed by 3D echocardiography; A case report
Abstract
Unroofed coronary sinus (UCS) is an uncommon congenital heart anomaly and the most unusual type of atrial septal defect. This report presents a 71-year-old female with palpitation and dyspnea following an emotional stress, who was referred for ablation of typical atrial flutter. Finally diagnosed with a partially unroofed CS causing a bidirectional shunt.
1 INTRODUCTION
A normal coronary sinus drains the cardiac veins to the right atrium. An Unroofed Coronary Sinus (UCS) drains the cardiac veins and unusually connects with the left atrium. This abnormal communication is because of a deficit in growth of a section between the left atrium and the coronary sinus. An alternative explanation is the subsequent dissolution of this partition.1 The UCS syndrome is a rare congenital heart anomaly2 and the most uncommon type of atrial septal defect,3 in which there is partial or complete lack of the roof of the coronary sinus,3 and may be associated with other congenital anomalies.4 It is necessary to diagnose this anomaly to determine the patient's prognosis, as it could be a source of brain abscess or cerebral emboli due to right–left shunt. Its diagnosis could be missed because of nonspecific clinical manifestations.5 Here, researchers report a case of UCS with a nonspecific presentation.
2 CASE PRESENTATION
A 71-year-old female admitted in our hospital for radiofrequency ablation due to atrial flutter. She had no known risk factor for coronary artery disease and no previous history of drug consumption. She complained of paroxysmal palpitation, dyspnea (NYHA functional class I-II) for the past 3 months, and typical exertional angina in the last week. She had been admitted 3 times due to symptomatic atrial flutter in this period. The laboratory data were normal. On physical examination, she was slightly cyanotic. Cardiac auscultation revealed a loud P2 and wide splitting of S2. The chest X-ray showed cardiomegaly, prominent bilateral pulmonary hilum, and signs of enlarged left and right atrium. To investigate probable underlying disease causing right atrium (RA) dilatation and atrial flutter, echocardiography was requested. Transthoracic echocardiography (TTE) was done and showed normal left ventricle (LV) size with ejection fraction of 55%; associated with right ventricle (RV), RA, and left atrium (LA) dilatation (Figure 1). First, trans-esophageal echocardiography (TEE) in another center confirmed these data and showed a 2 mm sized patent foramen oval (PFO) with bidirectional shunt. Moreover there were moderate tricuspid regurgitation (TR), severe pulmonary hypertension (PH) (pulmonary artery pressure [PAP] = 60 mmHg), and severely dilated main pulmonary artery (PA) (4.1 cm). No atrial septal defect (ASD) was found.
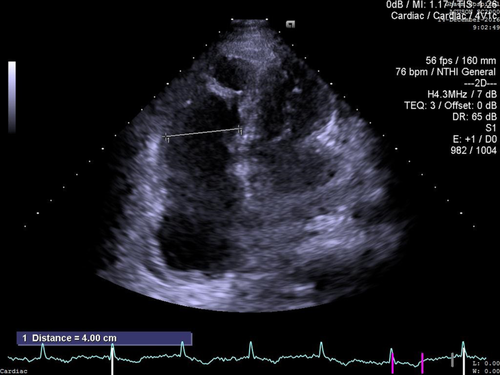
In Cathetherization laboratory before ablation, the patient underwent coronary angiography due to her recent chest pain, and showed no obstructive coronary artery disease; however, in the venous phase of the left coronary angiogram, coronary sinus (CS) was drained into the left atrium before its termination in RA. Therefore, with the suspicion of UCS, right heart catheterization was done, and blood gas analysis of the samples from all heart chambers was performed. As seen in Table 1, the results of the blood gas analyses are consistent with bidirectional shunt through the unroofed CS. Repeated TEE with an expert echocardiologist demonstrated severely dilated coronary sinus (22 mm) with large Thebesian valve. Incomplete UCS in the mid portion of the CS (defect size: 14 mm) confirmed by 2D, 3D, and contrast study and was associated with significant bidirectional shunt (Figure 2). Neither persistent left superior vena cava (PLSVC), nor anomalous pulmonary venous connection was detected. Finally, the patient was referred for corrective surgery with the diagnosis of partial UCS (Type III).
| Characteristics | SVC | IVC | HRA | LRA | MRA | LA | CS | PA | AO | PV | RV | LV |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PH | 7.43 | 7.42 | 7.4 | 7.43 | 7.4 | 7.41 | 7.43 | 7.44 | 7.43 | 7.42 | 7.44 | 7.47 |
| HCO3 | 30.8 | 31.7 | 33.4 | 31.6 | 32.4 | 28.5 | 31.6 | 33.7 | 29.7 | 31.7 | 33.2 | 35.8 |
| O2Sat | 75.2 | 78.4 | 77.2 | 89.6 | 78 | 89.9 | 89.6 | 82.7 | 90.3 | 94.1 | 83.4 | 92.7 |
- Abbreviations: SVC, superior vena cava; AO, aorta; PV, pulmonary vein; LA, left atrium; RV, right ventricle; IVC, inferior vena cava; CS, coronary sinus; HRA, high right atrium; LRA, low right atrium; PA, pulmonary artery; MRA, mid right atrium.

3 DISCUSSION
- Type I: Completely unroofed with LSVC.
- Type II: Completely unroofed without LSVC.
- Type III: Partially unroofed mid-portion.
- Type IV: Partially unroofed terminal portion.
The diagnosis of UCS has previously been made by cardiac angiography, surgery, or even necropsy.7 Although echocardiography has become one of the main assessment tools, the diagnosis of unroofed coronary sinus remains tricky and needs high degree of suspicion. The TEE is a semi-invasive procedure that improved visualization of most cardiac structure but requires premedication and/or sedation in a large number of patients,5 and in some patients may have a poor echo view. In the current case, the anomaly had been missed in the first TEE, and was suspected in angiography and then confirmed by repeated TEE. One surgical series showed that this condition correctly diagnosed preoperatively in only 6 out of 11 cases.5 In the current report, the authors presented an incomplete type III UCS with bidirectional shunt and PFO. We doubted the presence of UCS during angiography and confirmed it by performing repeated TEE while the first TEE before angiography failed to diagnose the anomaly. The researchers referred the patient for surgery; however, she refused to undergo an operation.
The UCS can cause a variety of symptoms. It could appear as asymptomatic, presented with nonspecific complaints, or with severe dyspnea and symptoms of overt right-sided heart failure from chronic right ventricular volume overload.3 This leads to a diagnosis in older age or a lack of diagnosis. The clinical presentation of UCS is mainly determined by the size of the defect between the CS and the left atrium (i.e., the degree of left-to-right shunting), and associated anomalies such as a persistent left SVC (i.e., brain abscess or infarction caused by a right-to-left shunt).8 According to the difficulty of diagnosis by signs or symptoms, UCS should be considered in patients with left-to-right interatrial shunt, unexplained arterial oxygen desaturation, or cerebral complication.4
TTE is the most commonly used non-invasive diagnostic modality, yet cardiac structures like CS, which is drained to the posterior wall of the LA or pulmonary veins are not well visualized by TTE.9 However, TEE and cardiac MRI could accurately assess these posterior structures.3 There are now many ways for diagnosing this anomaly better and quicker than previous methods, such as multi-detector CT and cardiac MR with their excellent spatial resolution, which allows for the visualization and accurate anatomic and morphological evaluation of the posterior structures of the heart.3, 4 Several case reports have suggested a multi-method for detecting this anomaly for better management.3, 7, 10 Three-dimensional TEE could obviously show the posterior cardiac structure and the connection between the LA and the CS, before the surgery, as done for the current case.11
4 CONCLUSION
In conclusion, this case demonstrated the usefulness of 3D-TEE in detecting the abnormal anatomy and the pathophysiology associated with the rare congenital anomaly of UCS. It is difficult to diagnose UCS because it is rare without specific laboratory findings. Dilated CS, enlarged right heart chambers, and left-to-right shunt flow, particularly without a clearly visualized atrial septal defect, are clues for UCS. The authors confirmed that 3D-TEE has practical and clinical applications, as a useful complementary and supplemental to 2D-TEE findings, for accurate diagnosis of UCS.
AUTHOR CONTRIBUTIONS
Dr. Mohammad Tayyebi analyzed and interpreted the patient data regarding the cardiovascular disease and managed patient. Dr. Afsoon Fazlinezhad helped in data gathering and echocardiographic evaluation. Dr. Mostafa Ahmadi helped in the patient catheterization and management. Dr. Faeze Keihanian helped in the diagnosis and management of the patient, and contributed in writing the first draft of the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENT
None.
CONFLICT OF INTEREST
None.
DATA AVAILABILITY STAteMeNT
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
ETHICAL APPROVAL
This study was performed in accordance with the Helsinki declaration. Data published anonymously.
CONSENT
A written informed consent was obtained from the patient.




