Two connected large epiploic appendixes make a loop: A case report
Ali Mehri Co-first author
Abstract
Small bowel obstruction (SBO) is a common cause of hospitalization in surgery ward and brings a notable morbidity and mortality with 30,000 annual deaths. In some cases, SBO develops due to the internal hernia. In this case, we present a case of internal hernia in a woman with normal large epiploic appendixes.
1 INTRODUCTION
Small bowel obstruction (SBO) is a common cause of hospitalization in the surgery ward and brings notable morbidity and mortality with 30,000 annual deaths. This condition is responsible for 15% of all acute abdominal surgeries.1, 2 It is reported that around 65–75 percent of SBOs are due to postoperative adhesions that usually occur within the first postoperative 4 weeks. The other pathologic factors that may cause SBO are malignancies (10%–20%), groin hernias (10%–20%), inflammatory bowel disease (5%), and volvulus (3%).3
Moreover, in around 0.2%–0.9% of the patients, SBO develops due to an internal hernia. This herniation may be developed due to the presence of abnormal changes in anatomy or the presence of normal anatomical variations. It is reported that the torsion and subsequent ischemia in epiploic appendices cause epiploic appendagitis and enlargement. In this situation, the enlarged appendixes may provide a condition for internal herniation.4
However, even some people have large epiploic appendixes that are normal but a part of an anatomic variation. These large epiploic appendixes are also a prone location for internal hernia.5 Still, the amount of herniation through large epiploic appendixes in the absence of appendagitis is very.6-10 Here, we present a case of internal hernia in a woman with normal large epiploic appendixes.
2 CASE PRESENTATION
An 87-year-old Caucasian female patient presented at the emergency room with the chief complaint of loss of defecation for 1 week. She also reported one episode of bilious vomiting. However, the gas passing was present. She also reported no symptoms of chill and fever but mild-to-moderate periumbilical abdominal pain. The past medical history was positive for a 20-year-old history of hysterectomy, hypertension, and cerebrovascular accident. Other parts of the history had no notable findings. In the case of vital signs assessment, the temperature was 36.9°C, respiratory rate was 17 times per minute, pulse rate was 80 beats per minute, and blood pressure was 150/90 mmHg. The physical examination revealed normal lung and heart auscultation. The abdomen was normal in observation, except for a moderate distention, and a midline scar for hysterectomy with no evident herniation. Abdominal sounds were decreased generally. Moreover, a periumbilical tenderness was present in the absence of rebound tenderness. The patient also underwent a digital rectal examination that showed normal fecal material.
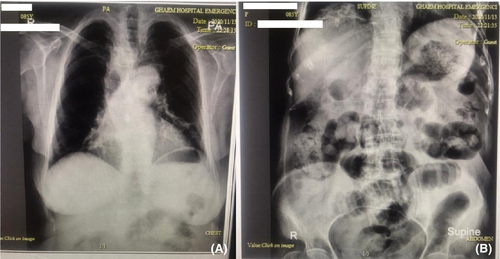
The subsequent laboratory examination also showed a white blood cell count of 10,100/dl with 80 percent neutrophils, hemoglobin of 14 g/dL, and platelet count of 208,000/dl. A biochemistry study reported a blood sugar level of 124 mg/dL, creatinine of 1 mg/dL, and amylase 39 of U/L. The electrolyte level assessment showed a sodium level of 140 mEq/dL and potassium of 3.7 mEq/dL. Furthermore, prothrombin time (PT), partial thromboplastin time, and international normalized ratio were 13 s, 28 s, and 1, respectively. In addition, as the patient was suspected of a lower GI obstruction, plain abdominal and chest radiographs were asked. The chest X-ray was normal; however, the abdominal X-ray revealed several distended loops of the small intestine, all were suggestive of obstruction (Figure 1). As serial abdominal examination showed a progressive tenderness intensity, a CT scan was not conducted for the patient.
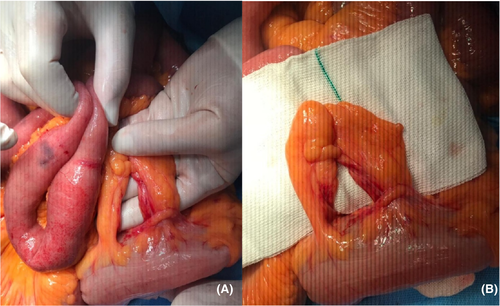
With this regard, a diagnosis of obstruction was confirmed, and the patient was prepared for open surgery. A nasogastric tube was inserted, and fecaloid material was evident in the bag with a one-liter volume. Because of the prolonged obstruction, small intestine materials were turned fecaloid. According to the obstructive pattern in imaging and the fecaloid material with evident stinky smell, the patient was planned for surgery. The patient was reanimated with intravenous fluids according to the urinary output. Then after, she was transferred to the operation room. Due to the fact that laparoscopic operations are not performed in our medical center for emergency patients, the patient underwent open surgery. A midline incision was used to access the small intestine. In the first inspection, although the expectation of adhesion bands due to the previous hysterectomy, the obstruction was not due to the adhesion band formation; a small bowel lope was incarcerated between large epiploic appendixes (Figure 2). The appendixes were excised, and the normal intestinal passage was resumed. The incarcerated small intestine loop with a 100 cm distance from the ileocecal valve and the epiploic appendices were located on the sigmoid colon. There was no evidence of epiploic appendagitis. The patient recovered from the surgery and was discharged with normal status.
3 DISCUSSION
Normally, when a surgeon faces an SBO case, a list of etiologies is suspected. However, the presence of an internal foramen formed from the adherence of two epiploic appendixes is a very rare condition. It is reported that in many cases, the inflammation of these appendixes is the etiology for obstruction; however, in an abdomen without any history of surgical operation, this may also occur. Epiploic appendixes are fat-containing structures that line the transverse and sigmoid colons, with no evident function.10 These usually range in size between 0.5 and 5 cm, according to the degree of the person's obesity. Usually, 50 to 100 numbers of these appendixes are present in a person. The function of these structures remained unknown in the body. These epiploic appendixes may become inflamed and make appendagitis. The enlarged appendixes in this situation can connect and make an aperture that is a suitable location for herniation. However, some cases have large connected epiploic appendixes, even in the absence of appendagitis. These appendixes may have a size as large as 15 cm in length. The case of our study also happened in an old woman with normal but enlarged and connected epiploic appendixes.
The presentation of an SBO patient in the background of incarceration between epiploic appendixes is just similar to the other obstruction cases due to other etiologies and the diagnosis is usually made after the ruling out of other causes during surgery. Imaging barely helps in the diagnosis of internal herniation. An exact inspection of abdominal computed tomography (CT) scan by an expert radiologist. However, plain radiography can sometimes present typical signs of obstruction, as in our case, the distended loops of the small bowel were present in the imaging.
The two most recent similar case reports stated that the number of published cases in this regard is 7 cases throughout history. With this consideration, our case is the eighth one. The first report on this state was published by Lau and Ong in 198411. The second case was reported 13 years later, after the report of the first case by Krijgsman and Salter12 at Westcliff-On-Sea, Essex, United Kingdom. The other five studies are available through the literature,6-10 as the two most recent were published in 201813 and 2020.7 Butt et al.14 also reported another case of SBO due to the entrapment of a small bowel loop between two inflamed epiploic appendices. Their case was a 48-year-old man who presented with colicky abdominal pain. At first, the radiology assessment showed no significant finding; however, the imaging and clinical findings were indicative of a small bowel obstruction after several days of hospitalization. The final diagnosis was made through surgical assessment.
The important issue in SBO due to the strangulation of the loops between two epiploic appendixes is the timely diagnosis. However, as internal hernias are usually diagnosed through surgery, it may take time for the patient to be at this stage and the intestine loop may be gangrene by then. Even this delay may bring fatality.15 However, as there were evident imaging findings in our case, the timely operation helped her to survive the condition.
4 CONCLUSION
The internal small bowel herniation is a rare entity; however, SBO due to the herniation of an intestinal loop between two connected large epiploic appendixes is an extremely rare condition, as less than 10 cases around the world have been reported. This diagnosis should be listed at the end of all differential diagnoses for an SBO. However, through the surgery process and after the exclusion of all other differentials, this diagnosis can be made.
AUTHOR CONTRIBUTIONS
Fariba Zabihi initiated the preparation of manuscript for scientific publication. Ali Mehri coauthored and revised the manuscript and did proofreading. Mohammad Etezadpour done the surgery and reviewed the final version of manuscript. All authors were directly or indirectly involved in the care of the patient.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
There was no specific funding.
CONFLICT OF INTEREST
The authors report no conflict of interest.
ETHICAL APPROVAL
Surgery and all other procedures were done in agreement of 1975 Declaration of Helsinki.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.




