Retroperitoneal myxosarcoma in a cat
Abstract
This report details a retroperitoneal myxosarcoma in a cat that exhibited extremely aggressive biological behavior. An exploratory midline celiotomy revealed a left-sided retroperitoneal mass firmly adhered to the hypaxial musculature. Histopathological evaluation identified the mass as a myxosarcoma. Following surgical excision, the mass rapidly recurred within 6 weeks after surgery.
1 INTRODUCTION
Soft tissue sarcomas (STSs) constitute a heterogenous group of mesenchymal neoplasms that arise from various connective tissues throughout the body. Although they can develop in any anatomic location, they frequently involve the cutaneous and subcutaneous tissues.1 Most STSs display similar biological behaviors, characterized by pseudo-encapsulated and locally invasive masses capable of infiltrating into fascial planes.1 Histopathology is used to further classify these neoplasms according to phenotypic characteristics or tissues of origin, and is also used for tumor grading.2 The treatment of choice for STSs is wide surgical excision; histologic grading and evaluation of surgical margins are performed after surgical resection to inform the likelihood of local recurrence and metastatic disease development.1 Included within the population of STSs are liposarcomas, perivascular wall tumors, fibrosarcomas, and myxosarcomas.1
Myxosarcomas are neoplasms that are fibroblastic in origin and characterized by the production of an abundant myxoid matrix rich in mucopolysaccharides.3 These tumors are infrequently diagnosed in middle-aged or older dogs and cats, and of the available literature, they are more commonly reported in dogs.1 Although most myxosarcomas in canines occur as subcutaneous neoplasms of the trunk or limbs, they have also been reported in the heart, eye, spleen, brain, temporomandibular joint, vertebra, and lungs.3-10 There are at least two reports available on myxosarcomas in cats, which describe one myxosarcoma arising from the kidney and one arising from the hindlimb musculature.11, 12 Both reports describe different tumor locations (muscle and kidney) and survival (both cats alive at 6 and 14 months after surgery).11, 12 Thus in order to better characterize the biological behavior and expected prognosis of myxosarcoma in felines, additional cases need to be evaluated and reported. The current report describes the clinicopathologic findings of the first documented case of a myxosarcoma arising from the hypaxial musculature in a cat.
2 CASE REPORT
A 13-year-old spayed female domestic longhaired cat was referred to the Animal Cancer Care and Research Center at Virginia Tech for further evaluation of a large soft tissue mass palpable in the left flank. The owner reported a history of decreased activity levels and impaired ambulation, which the owner believed were caused by the size of the mass; otherwise, the cat had been doing well at home with a normal appetite. The referring veterinarian had previously obtained fine-needle aspirate samples of the mass, which were interpreted cytologically as spindle cell proliferation with moderate atypia. A biopsy for histopathological evaluation was recommended for further characterization of the mass. Upon presentation to the Animal Cancer Care and Research Center, the patient was fractious and could not be evaluated until sedation was administered. A physical examination was performed, which revealed a subcutaneous soft tissue mass measuring 10.5 × 11.6 cm in the region of the left flank. The skin overlying the mass was grossly normal in appearance and was freely moveable over the mass. The mass was firm and immoveable, adhered to the underlying muscle, and its deep extent was ill-defined. The other physical examination findings were largely unremarkable. A complete blood count (CBC), serum biochemistry profile, and blood lactate level were performed. The CBC revealed a normocytic, normochromic non-regenerative anemia without reticulocytosis (hematocrit 29.1% [30.3–52.3] and reticulocyte count 15.3 K/μl [3.0–50.0]) with a mild and mature neutrophilia of 10.51 K/μl (2.30–10.29). The biochemistry panel showed an increase only in gamma-glutamyl transferase (GGT), which was elevated at 8 U/L (0–4). A computerized tomography (CT) scan with contrast was performed of the patient's thorax and abdomen. A small volume of pleural effusion was noted bilaterally. In the abdomen, a large fluid attenuating, heterogeneously enhancing mass was present in the left dorsal retroperitoneal space from about the level of T13 to L5 (Figure 1). The mass appeared to originate from the left psoas muscle at the level of L3 and caused marked displacement of the left kidney. While the caudal vena cava was also displaced medially, the abdominal aorta was closely associated with the medial aspect of the mass and followed it until the aortic bifurcation. Within the liver, multiple hypoattenuating, non-enhancing nodules were present in several liver lobes. Although the other abdominal viscera visualized within normal limits, the adrenal glands were not visible and may have been displaced by the retroperitoneal mass. A small volume of peritoneal effusion was present. Following the CT scan, a fine-needle aspirate (FNA) of the retroperitoneal mass was collected. The cytologic interpretation concluded that the mass represented spindle cell proliferation, and was a potential sarcoma. The ultrasonographer determined that the small amounts of pleural and peritoneal effusion and the liver nodules were not readily accessible for aspiration due to obstruction by the retroperitoneal mass.

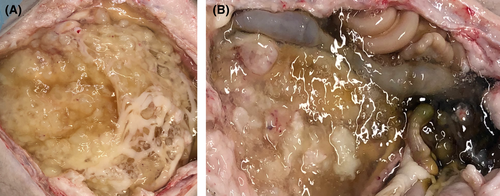
General anesthesia was performed for an exploratory midline celiotomy. Upon entering the abdomen, a moderate amount of slightly cloudy, tan, and highly viscous free fluid was visualized. Multiple yellow opaque nodules were found adhered to the omentum and were subsequently resected using a combination of blunt dissection and monopolar electrocautery. Multiple raised lesions, some of them cystic in appearance, were observed in all lobes of the liver, and a biopsy sample from the quadrate liver lobe was obtained using the Guillotine method. There was a large, left-sided, irregular mass present in the left retroperitoneal space that had displaced the left kidney both medially and ventrally, and displaced the small intestinal loops medially across midline. The left retroperitoneal membrane was penetrated, and the left kidney and ureter were carefully dissected away from the mass and retracted medially. The mass was marginally excised using a combination of blunt dissection, dissection with monopolar and bipolar electrocautery, and the LigaSure™ Small Jaw handpiece (Medtronic). The retroperitoneal mass was firmly adhered to the left abdominal body wall, and consequently, a portion of the body wall musculature that was adhered to the mass and appeared grossly abnormal was resected together with the mass. The mass was also found to be adhered to the aorta and caudal vena cava (CVC). The aorta and the caudal vena cava were carefully dissected away from the mass. Additionally, the mass was very firmly adhered to the hypaxial musculature at the caudal thoracic and cranial lumbar vertebrae; part of this musculature was excised along with the mass using a combination of the Ligasure™ Small Jaw handpiece and bipolar electrocautery. Following removal, the abdomen was lavaged with warm sterile saline before closure. The excised tissues (Figure 2) were placed in 10% neutral buffered formalin and submitted for histopathologic evaluation.

Throughout the perioperative period, the patient was noted to experience volume-responsive hypotension. This hypotension persisted into the post-operative period. The patient's volume support under anesthesia consisted of a combination of intravenous Hetastarch and Lactated Ringer's Solution. The patient was subsequently administered a unit each of packed red blood cells (RBC) and fresh-frozen plasma in the intensive care unit (ICU) post-surgery for continued volume support. The hypotension resolved, and her blood pressure remained stable for the remainder of her stay in the ICU. Postoperatively, the cat was maintained on a CRI of ketamine (2 μg/kg/min), IV buprenorphine (0.02 mg/kg every 6 h), and PO gabapentin (8 mg/kg every 8 h) for analgesia. Pain scoring was performed every 2 h and the cat's pain score remained acceptable, indicating appropriate pain management after surgery. Two days after surgery, the ketamine CRI was discontinued, but the PO gabapentin was continued at the same dose and frequency to maintain patient comfort. During her post-operative recovery in hospital, the cat was noted to have developed right hindlimb weakness. Both the withdrawal reflex and motor responses were present in the right hindlimb, which maintained strong femoral and dorsal pedal pulses. The cat was deemed suitable for discharge from hospital 3 days after surgery, and pain management was continued with gabapentin (PO) and buprenorphine (transmucosal) for 2 weeks after surgery. The cat took nearly 2 weeks to regain moderate strength in the limb after discharge. To date, no reasonable explanation has been proposed to explain this observation.
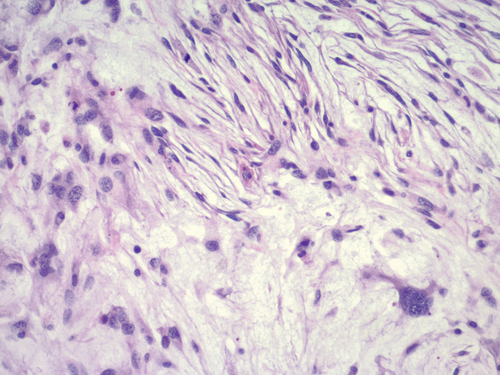
The histopathology report described the retroperitoneal mass as being poorly demarcated and infiltrative, with large necrotic areas. The mass infiltrated surrounding adipose tissue and was composed of cells that formed small streams and stacks among large amounts of myxoid matrix. The cells were medium-sized to large and stellate to fusiform with small amounts of eosinophilic cytoplasm and indistinct cell borders (Figure 3). There were 14 mitotic figures in ten 400× fields (2.37 mm2), and tumor cells extended into multiple surgical margins. Based on the matrix produced and the presence of stellate cells, the mass was diagnosed as a retroperitoneal myxosarcoma. The hepatic biopsy sample was diagnosed as a biliary telangiectasia. The omental nodules that had been resected were not submitted for histopathologic evaluation. Adjuvant radiation therapy was not recommended due to the size of the radiation field, the option of trying a chemotherapeutic protocol was discussed with the owner, with the understanding that the efficacy of chemotherapy in feline myxosarcoma is undetermined. The owner declined adjuvant chemotherapy and was advised to follow-up with routine active surveillance to monitor for local recurrence and metastasis.
The owners reported that the cat initially did well after being discharged from the hospital. She continued to gain strength in her right hindlimb, maintained a good appetite, and exhibited a positive change in her behavior—she became more affectionate and interactive with the owners. This change in behavior was also noted by the veterinary staff who worked with the cat during her post-surgery recheck, reporting that the cat was much more amenable to handling. Approximately 5 weeks after surgery, the owner contacted the Animal Cancer Care and Research Center to report that the mass had rapidly recurred. The cat's previously voracious appetite had decreased, and she was no longer defecating regularly. At her 6-week post-surgical recheck, a firm subcutaneous mass was noted on the patient's left flank (approximately 15.0 × 14.0 cm). The mass was firmly adhered to the underlying musculature, and the ventral aspect of the mass was ill-defined. An abdominal ultrasound was performed, which revealed a large lobulated intraabdominal mass with mixed echogenicity displacing abdominal viscera to the right. The sonographer could not reliably delineate the mass due to its large size and thus could not obtain an accurate measurement of size. Although cytological or biopsy samples were not obtained, based on the location and ultrasonographic appearance of the mass, it was suspected to be an aggressive recurrence of the retroperitoneal myxosarcoma that was previously excised. Neither surgical re-excision nor radiation therapy was considered to offer the patient any clinical benefit, and the owners elected for palliative care at home. The cat's appetite continued to decrease and her defecation remained irregular. Approximately 8 weeks after surgery, the owners elected for humane euthanasia of their pet. Gross examination of the cat during necropsy revealed the entire abdominal cavity to be filled with a gelatinous mucoid material that adhered to and enveloped the serosal surfaces of all abdominal organs (Figure 4). Multiple soft-to-firm white indiscrete masses expanded the mesenteric adipose. A soft fluid-filled lobulated mass was noted on the ventral surface of the left lateral liver lobe. Multiple soft-to-firm white coalescing masses were noted to be firmly adhered to the hypaxial muscles from L1-L6. The histopathology report described effacement of the mesenteric adipose by the tumor. Similar to the microscopic description of the original tumor, these tumor cells were spindle cells arranged in short stacks or whorls, embedded in an abundant myxomatous stroma (Figure 5). The histopathologic diagnosis of the tumor was an abdominal myxosarcoma with sarcomatosis of the liver and left kidney.

3 DISCUSSION
This case report details the clinical presentation and outcome of a 13 year-old spayed female domestic cat diagnosed with a retroperitoneal myxosarcoma that recurred aggressively after surgical resection. Due to the sparse amount of clinical data available on feline myxosarcomas, the information in this case report will contribute to building the body of knowledge needed to understand the disease. Myxosarcomas are a subset of STSs that are uncommonly observed in veterinary species, especially in the cat, and histopathology is necessary to differentiate malignant myxosarcomas from benign myxomas. This differentiation between myxosarcomas and myxomas can be challenging, but myxosarcomas have some distinct characteristics. For instance, myxosarcomas are often more vascularized and more cellular then myxomas, and contain mitotic figures and nuclear pleomorphism.13 Irrespective of histologic differentiation of malignancy, myxosarcomas and myxomas are characteristically described as being infiltrative growths will poorly defined margins, with myxosarcomas displaying moderate-to-high rates of recurrence following surgical excision.13, 14 Metastasis can occur with myxosarcomas, but the reported rates of metastasis have been variable.13-16 There is one recent report describing synovial myxomas in 16 cats.15 These synovial myxomas were described as slow-growing and locally infiltrative, no metastases were noted, and no deaths were attributed to the tumors. These authors postulated that synovial myxomas in cats may originate as synovial herniation and periarticular cysts in degenerative joint disease, and progressing to myxomas.
Myxosarcomas have been reported in dogs to occur in multiple anatomical locations, yet reports describing myxosarcomas in cats are much more limited. To the authors' knowledge, there are only two reports available on feline myxosarcoma.11, 12 One report describes a cat diagnosed with a hindlimb myxosarcoma.12 This cat was an 8-year-old spayed female domestic shorthair that presented for non-weight bearing lameness in its left hindlimb. This cat had experienced a traumatic fracture in its left femur 4 years prior, which was stabilized with an intramedullary pin and four cerclage wires. Due to suspicion of neoplasia, a left hindlimb amputation was performed. The pathologist reported extensive infiltration of neoplastic tissue within the gastrocnemius and other major muscles of the limb. The diaphyses of the femur, tibia, and fibula were necrotic, and fusiform to stellate neoplastic cells within a mucinous stroma observed. The cat was diagnosed with a low-grade myxosarcoma, and no evidence of metastatic disease was observed 6 months postoperatively. The owners last reported that the patient had been doing well at 6 months post-surgery, and the cat was lost to follow-up thereafter.12 A similar clinical outcome was observed in a case report of a feline perirenal/renal myxosarcoma.11 A 12-year-old spayed female domestic shorthaired cat presented for evaluation of a large and firm palpable mass in its cranial abdominal cavity. During an abdominal exploratory laparotomy, a hemoabdomen and mass associated with the right kidney were observed. A right nephrectomy was performed, and during histopathologic examination, neoplastic spindle to stellate cells in an abundant myxoid matrix were observed. Positive immunoreactivity to vimentin and negative immunoreactivity to cytokeratin of the neoplastic cells confirmed a mesenchymal origin, and based on these collective findings, a diagnosis of a well-differentiated renal myxosarcoma was made. Fourteen months postoperatively, no evidence of metastatic disease or tumor recurrence were seen in this patient based on repeated staging diagnostics that included thoracic radiographs and an abdominal ultrasound.11
Based on the available literature, the clinical presentation and outcomes observed in two cats diagnosed with myxosarcomas of the hindlimb and the kidney are considerably different than what was observed in the current report's patient. This patient's mass appeared to have originated from the hypaxial musculature, which has not been previously reported in cats. Although this could not be confirmed histologically, the mass was found to be firmly adhered to the hypaxial musculature during the abdominal exploratory procedure. While its sheer size caused compression and displacement of the surrounding abdominal viscera, no adhesions to them were observed. Despite surgical resection, the tumor in this cat rapidly recurred within the 6-week post-operative window, compared to the longer recurrence-free intervals of the cats from the previous 2 reports.11, 12
The observations from this case combined with the limited literature available on myxosarcoma in cats suggest that a broad spectrum of biological behavior for myxosarcomas exists in feline patients. The extremely limited number of available reports characterizing feline myxosarcomas presents a challenge to clinicians, who lack the historical data to allow for accurate prediction of prognosis, and to guide treatment recommendations. More data are needed in order to better characterize the biological behavior of myxosarcoma in cats.
4 CONCLUSION
The cat in this report had an aggressive recurrence of its retroperitoneal myxosarcoma nearly 6 weeks after surgical resection of the primary tumor. In order to better characterize and treat these neoplasms in cats, additional data are needed. This case report contributes to the building of a body of knowledge to better our understanding of feline myxosarcomas. To the authors' knowledge, this is the first documented case of a myxosarcoma arising from the hypaxial musculature in a cat.
AUTHOR CONTRIBUTIONS
Haleigh Hixson was directly involved with research of the case details and manuscript preparation; Joanne Tuohy, Brittany Ciepluch, and Katharine Kierski were directly involved in clinical management of the case, and manuscript preparation; Kevin Lahmers and Sheryl Coutermarsh-Ott were directly involved in histopathology processing and evaluation, and manuscript preparation.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST
None.
ETHICAL APPROVAL
Verbal consent for publication was obtained from the client prior to manuscript preparation.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




