Rectal foreign body in adult male: Unusual case report and literature review
Abstract
The majority of rectal foreign bodies inserted by adults are for self-gratification. As a result, they will probably be smooth, rounded, tubular, or egg-shaped to make insertion and extraction easier. Herein, we describe a 50-year-old man who inserts a water bottle into a region 10 mm from the anorectal junction.
1 INTRODUCTION
Rectal foreign body (RFB) insertion has only been reported occasionally in published papers. Colorectal foreign bodies (CFBs) are a common occurrence in emergency and colorectal surgical departments, with some writers suggesting that the prevalence is on the increase.1 RFBs can be a challenging diagnostic and therapeutic issue, starting with the emergency department (ED) examination and continuing to the post-extraction stage. Instruments can be inserted into the rectum for a variety of reasons, including diagnostic or therapeutic purposes, self-treatment of anorectal disorders, criminal assault or accidents, and (most commonly) sexual reasons.2 Although most instruments are inserted through the anus, a foreign body (FB) can also be ingested, transported through the gastrointestinal tract, and held up in the rectum.3 Various instruments, including bulbs, bottles, billy clubs, impulse body spray cans, and turkey basters, have been described as having retained RFBs. A comprehensive approach to the diagnosis and treatment of RFBs is necessary due to the large variety of instruments and the variation in injury produced to local tissues of the rectum and distal colon.4 Delay in presentation is one of the most common challenges in the management of RFBs, since many patients are ashamed and hesitant to come to the hospital.4
The majority of these individuals come to the ED after attempting to extract the instrument at home. Furthermore, patients in the ED may be less than honest about the cause of their visit, resulting in prolonged workups and further delays. Complications such as delayed perforation or severe bleeding from the rectum may occur even after the FB has been extracted. As a result, a step-by-step procedure that includes diagnosis, removal, and post-extraction assessment is required.4
A useful categorization of RFBs is that it classifies them into two categories: voluntary and involuntary, as well as sexual and nonsexual. Devices that are inserted voluntarily and for sexual stimulation are one of the most common types of RFBs. The FBs commonly described were plastic or glass bottles, cucumbers, light bulbs, as well as tube lights, ax handles, broomsticks, carrots, wooden, or rubber instruments.3-5 Rape and sexual assault are the most common causes of involuntary sexual FBs. Nonsexual FBs are more commonly observed in the elderly, adolescents, and people with psychological disorders. The instruments can cause severe trauma. As a result, all FB maintained in the rectal region should be considered potentially dangerous.4 Herein, we describe a 50-year-old man who was inserting a large FB into the rectum. The patient had no obvious signs of perforation, and we managed to extract it without surgical procedure.
2 CASE PRESENTATION
On February 10, 2022, a 50-year-old man with a history of depression attempted to insert a large FB (a bottle containing 250 cc of water) into his anus. After 3 days, he was brought to the ED by his wife due to anorexia, abdominal pain, and lack of defecation. Because of his embarrassment and fear of his wife, he did not provide any history of the presence of a FB in the rectum and arrived at the ED late.
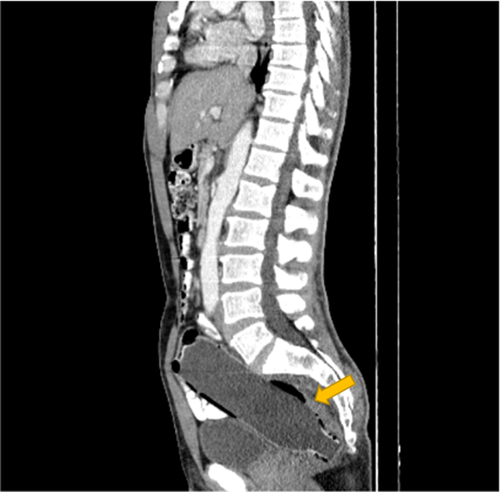
On examination, he had normal vital signs and was not ill. Laboratory findings were not abnormal. An ultrasound examination revealed evidence of a FB in the rectum. A contrast-enhanced computed tomography scan (CT scan) of the abdomen and pelvis showed a bottle full of water (measuring about 193 mm × 47 mm) in a region 10 mm from the anorectal junction without any obvious perforation (see Figure 1). The basal of the bottle was in the proximal region of the colon, and the opening of the bottle was near the anus.
Consultation with the surgical service was requested immediately, and the patient was transferred to the operating room. After prep, drep, and lumbar anesthesia were performed to relieve the spasm of the colon and pain, the bottle was carefully and slowly dragged from the rectum to the opening of the anus, and it was successfully extracted by the surgeon without rupture or bleeding.
Finally, the patient was transferred to the surgical ward and was prescribed ceftriaxone ampoule (1 gr) twice a day (BID) and metronidazole ampoule (500 mg) three times a day (TDS). Sigmoidoscopy showed no evidence of bleeding, injury, or perforation 2 days after the extraction of the FB. After 5 days, he was discharged from the hospital in good general condition and without incontinency and was referred to a psychiatric clinic. The patient had no perforation, bleeding, or fecal incontinence during the one-month follow-up. Written informed consent was obtained from the patient for the publication of this report. This study was conducted according to the Declaration of Helsinki Principles. Also, CARE guidelines and methodology were followed in this study.
3 DISCUSSION
Although patients of different ages and ethnicities have been described with retained RFBs, more than two-thirds of patients with rectal bodies are males between the ages of 30 and 40, and individuals as old as 90 have also been described.4 They may complain of symptoms such as ambiguous abdominal pain, rectal bleeding, pain, and sometimes constipation.3-5
In complicated cases, signs of infection or perforation may be seen. A thorough abdominal examination should be performed to evaluate for the symptoms of peritonitis or the possibility of palpating an object trans-abdominally. The RFB can be sensed in the lower abdomen in either the left or right quadrant. Rectal examination is important in the diagnosis, but it should be done after the X-ray abdomen to avoid accidental injury to the surgeon from sharp instruments. In the case of an RFB patient, laboratory testing is not particularly useful.4
Most RFBs that are inserted into the anus by adults are for self-gratification.6 As a result, the instruments used by patients are usually smooth, rounded, cylindrical, or egg-shaped to make insertion and removal easier. The form, size, and location of the RFB, as well as the presence or absence of perforation and the patient's hemodynamic condition, all determine whether it can be removed trans-anally.5
In a non-perforated stable patient, the instrument should be removed utilizing a local block and/or conscious sedation via the trans-anal technique. In our case, the FB was slowly and carefully removed from the large intestine by the surgeon due to the stability of his hemodynamic state. If the conservative procedure without surgery fails, the patient should be sent to the operating room for general anesthesia and a trans-anal extraction attempt. Patients with perforated or ischemic bowel, as well as those who have failed trans-anal attempts, should have a laparotomy.4
The majority of RFBs can be removed trans-anally, but when they penetrate deeper into the sigmoid colon or there is a large foreign instrument present, extraction is impossible.7 In our patient, the basal, smooth, large part of the bottle was in the proximal colon, which makes it much more difficult to extract with colonoscopy. The surgeon extracted a large bottle of water from the anus.
4 CONCLUSION
In any patient with a history of abdominal pain, psychiatric disorders, and lack of cooperation in the ED, rectal examination (touch rectal) for FB or anal lesions should be considered in addition to abdominal examination. A plain abdominal radiography and a rectal examination confirm the diagnosis. The management of FBs in the rectum should be well organized. Only extremely low-lying objects can be manually extracted without an anesthetic. To assist extraction, patients with high-lying and large FBs usually require general anesthesia to achieve complete relaxation of the anal sphincters. As a whole, only patients with perforation, peritonitis, or FB impaction should have open surgery.
AUTHOR CONTRIBUTIONS
ESB and ASh involved in the collecting of samples and data. MF and ZZ comprised in the interpretation writing, editing of the manuscript. MS preparing the draft and submitted of the manuscript. All authors reviewed and approved the final version of the manuscript.
ACKNOWLEDGEMENT
Declared none.
CONFLICT OF INTEREST
None declared.
Open Research
DATA AVAILABILITY STATEMENT
The data are available with the correspondence author and can be achieved on request.
The study was approved by our local ethics committee.
Written informed consent was obtained from the patient for publication of this report.




