Multiple nodular lesions following Pneumocystis pneumonia in a non-HIV immunocompromised patient
Key Clinical Message
Cytomegalovirus superinfection is associated with a poor prognosis in non-HIVPneumocystis pneumonia (PCP) and can cause deterioration of PCP not only simultaneously but also after initiating PCP treatment. Cytomegalovirus pneumonia should be considered in cases with deterioration after initiating PCP treatment; multiple nodular lesions are useful findings for the diagnosis.
An 80-year-old man presented with a 3-week history of progressive dyspnea. He was diagnosed with acute exacerbation of interstitial pneumonia with respiratory failure; administration of prednisolone (1 mg/kg/day) and cyclosporine (2 mg/kg/day) was initiated. Trimethoprim (80 mg/day)/sulfamethoxazole (400 mg/day) was also administered for Pneumocystis pneumonia (PCP) prophylaxis owing to his immunosuppressive state. Based on previous history and physical and laboratory investigations, he had no evidence of connective tissue disorder. His respiratory condition improved 31 days after admission (Fig. 1A). On day 39, he complained of worsening dyspnea; computed tomography (CT) revealed bilateral patchy ground glass opacity (Fig. 1B). Based on β-D-glucan level, PCP was diagnosed, and trimethoprim/sulfamethoxazole was subsequently increased from prophylactic dose to treatment dose (trimethoprim 720 mg/day and sulfamethoxazole 3600 mg/day). His respiratory condition improved and then deteriorated on day 49, and multiple nodules were noted on CT (Fig. 1C–G). Tests for Aspergillus galactomannan, Candida mannan, and Cryptococcus antigens were negative. Sputum and blood culture showed no remarkable findings. Bronchoscopy was not performed owing to severe respiratory failure during the disease course; however, based on conversion into positive cytomegalovirus (CMV) pp65 antigenemia, CMV pneumonia was diagnosed. Ganciclovir was administered in addition to trimethoprim/sulfamethoxazole; his condition improved, with negative conversion of CMV pp65 antigenemia. CMV pneumonia and PCP were completely treated for 21 days.
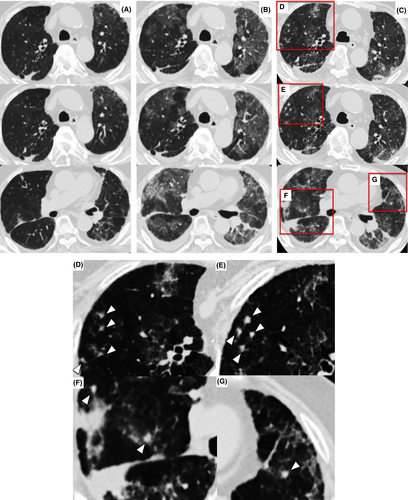
CMV superinfection is associated with a poor prognosis in non-HIV PCP 1. Although ground glass opacity is observed on CT in both diseases, variously sized multiple nodules are observed more frequently in CMV than in PCP 2. Aspergillus, Cryptococcus, and Nocardia infection are included in the differential diagnosis of pulmonary nodules in a non-HIV immunocompromised patient; however, the nodules in CMV pneumonia are smaller (<1 cm) on CT 3. CMV pneumonia should be considered in cases showing not only simultaneous infection with PCP but also deterioration after initiating PCP treatment; small multiple nodular lesions are useful findings for confirming the diagnosis.
Conflict of Interest
None declared.