Penetrating vertebral artery injury treated by combining the “zone” approach and imaging tests: A case report
Abstract
Patients with vertebral artery injury from penetrating neck trauma may not present with signs of vascular injury because of anatomical characteristics and concomitant conditions, such as hypothermia and shock. If patients are hemodynamically stable, imaging tests should be performed to examine the posterior components, including the vertebral artery.
1 INTRODUCTION
Penetrating injury to the vertebral artery (VA) is uncommon because the proximal third of the VA lies in the deepest plane at the root of the neck and the remaining two-thirds are surrounded by the cervical vertebrae.1 The anterior aspect of the VA is covered by organs (such as the thyroid gland, trachea, and esophagus), muscles, and ligaments. Therefore, it is more difficult to access the VA than the carotid artery and jugular vein during surgery.2 Accordingly, in cases of stab wounds to the neck, it is difficult to predict the presence of VA injury (VAI). In the present case, VAI was discovered fortuitously. Bleeding from VAI caused hypothermia and severe metabolic acidosis due to decreased blood pressure, which is one of the three signs of death. In addition, the wound was temporarily hemostatic due to the decrease in blood pressure. However, we were able to save the patient's life by performing VA embolization after temporary surgical treatment of the wound. Here, we report the early-phase treatment.
2 CASE HISTORY
A 67-year-old woman with a history of depression attempted suicide by stabbing her neck with a kitchen knife. She was found lying outside her house and was urgently transferred to our hospital. The ambient air temperature was low on that day. On admission, she had consciousness disturbance and a 3-cm stab wound with surrounding hematoma on the left side of the neck.
Her blood pressure and O2 saturation were unmeasurable, pulse was 102 bpm, and respiratory rate was 34 breaths/min. She had metabolic acidemia with a low body temperature of 30°C. The results of blood tests other than that for metabolic acidemia on admission were unremarkable (Table 1). The cause of unmeasurable blood pressure was considered to be the effect of hypothermia or bleeding from the neck. Therefore, as the patient could not be moved to the computed tomography (CT) room, we performed tracheal intubation and started searching for the source of bleeding under general anesthesia while treating her for hypothermia in the emergency room. As the stab wound was located in Zone II, we searched for the source of bleeding by exposing the internal jugular vein, common carotid artery, trachea, and thyroid gland; however, we could not find a source of bleeding other than bleeding from the sternocleidomastoid and platysma muscles. Simultaneously, her body temperature increased by warmed fluid replacement and her pH normalized, which led to an increase in blood pressure and stabilization of hemodynamics during the first surgical procedure. Therefore, we planned to clean and close the wound. However, when we shifted the trachea to the right for wound irrigation, we observed pulsating bleeding from the deep portion of the wound, and her blood pressure rapidly decreased. An approximately 2-cm penetrating wound was found in the anterior longitudinal ligament and the scalene muscle at the anterior aspect of the left cervical cord at C5. The transverse process immediately below was fractured, and there was arterial hemorrhage from the site. The patient was diagnosed with hemorrhagic shock due to left VAI.
| Blood | Blood gas analysis | (O2 mask 10 L/min) | |
|---|---|---|---|
| WBC | 7900 U/μl | pH | 7.195 |
| RBC | 327 × 104 U/μl | pO2 | 381 Torr |
| Hb | 9.7 g/dl | pCO2 | 36.1 Torr |
| Plt | 23.5 × 104 U/μl | HCO3− | 13.4 mEq/L |
| Na | 139 mEq/L | SaO2 | 99.9% |
| K | 4.3 mEq/L | Lactate | 9.0 mmol/L |
| Cl | 106 mEq/L | ||
| AST | 107 U/L | ||
| ALT | 60 U/L | ||
| LDH | 233 U/L | ||
| Tp | 6.6 g/dl | ||
| Alb | 4.0 g/dl | ||
| BUN | 25.0 U/L | ||
| Cr | 1.18 mg/dl | ||
| CRP | 0.1 mg/dl | ||
| BS | 448 mg/dl | ||
| HbA1c | 5.6 | ||
| PT | 100% | ||
| PT-INR | 1.1 | ||
| APTT | 29.1 s | ||
| Fib | 162 mg/dl | ||
| FDP | 8.2 µg/ml |
- Abbreviations: Alb, Albumin; ALT, alanine aminotransferase; APTT, activated partial thromboplastin time; AST, aspartate transaminase; BS, blood sugar; BUN, blood urea nitrogen; Cl, chloride; Cr, creatinine; CRP, C-reactive protein; FDP, fibrinogen degradation product; Fib, Fibrinogen; Hb, hemoglobin; HbA1c, glycated hemoglobin; K, potassium; LDH, lactate dehydrogenase; Na, sodium; Plt, platelets; PT, partial thromboplastin; RBC, red blood cells; Tp, total protein; WBC, white blood cells.
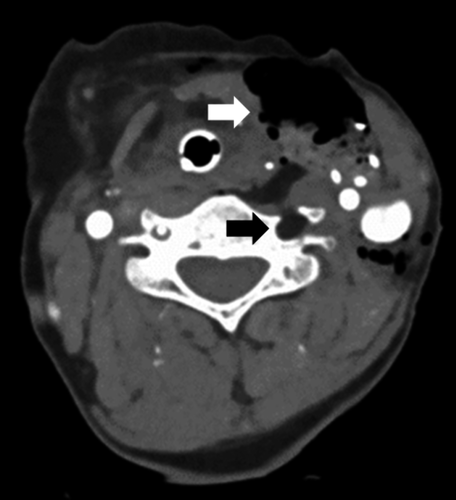
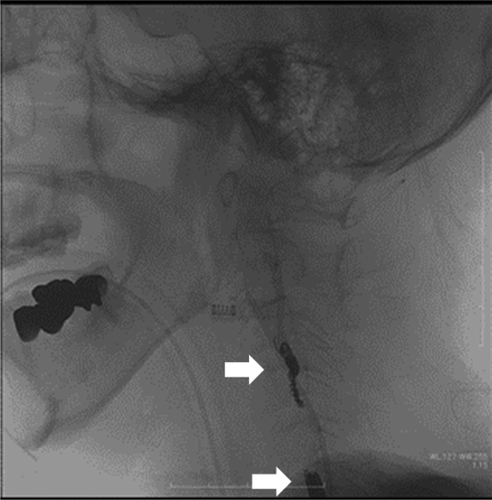
As the injury was located in the V2 segment of the VA, it was difficult to control the bleeding under direct observation. Therefore, bone wax was embedded in the transverse foramen of the cervical vertebra at the injury site, and gauze was inserted in the upper layer for temporary closure of the skin wound, which resulted in successful hemostasis (Figure 1). Contrast-enhanced CT of the neck showed that the bone wax was embedded in the transverse foramen and hemostasis was confirmed (Figure 2). After confirming the absence of other bleeding sources, left VA embolization was scheduled in order to achieve secure hemostasis. Angiography indicated that the left VA was disrupted at the V2 segment, and there was no extravasation of the contrast agent. Anastomosis was observed between the left occipital artery and the left VA, and coil embolization was performed at the V2 segment of the left VA; complete hemostasis was achieved by internal trapping of the affected VA (Figure 3).

After admission to the intensive care unit (ICU), endoscopic examination revealed no esophageal injury, and we removed the gauze and bone wax. The patient was extubated and discharged from the ICU on the 4th day of admission. She was discharged from the hospital on the 106th day of hospitalization following treatment for depression.
3 DISCUSSION
The testing, treatment approach, and management of neck injury differ depending on the areas involved and the severity of injury. For the purpose of evaluating neck injury, the neck is divided into three zones. Zone I is the area below the cricoid cartilage, Zone II is the area between the cricoid cartilage and the angle of the mandible, and Zone III is the area above the angle of the mandible.1, 3-5 The “zone” approach is considered useful because it contributes to better management and improved prognosis. Since Zone II includes the carotid artery, VA, and internal jugular vein, surgeons should exercise caution not to damage these vessels and organs during surgery in this zone.3, 4 However, in recent years, it has been demonstrated that a single wound can extend over multiple zones, and the utility of the “no zone” approach using imaging techniques has been reported.6 There is no consensus on which approach (“zone” or “no zone”) is more useful for the treatment and management of neck injuries. The “zone” approach is more suitable if patients have hard signs and/or are hemodynamically unstable because they need immediate surgery (Table 2).4
| Hard signs of vascular injury |
| Severe or uncontrolled hemorrhage |
| Large, expanding, or pulsatile hematoma |
| Thrills or bruits |
| Shock unresponsive to IV fluid resuscitation |
| Absent or diminished radial pulse |
| Hard signs of aerodigestive injury |
| Air bubbling from a wound |
| Massive hemoptysis or hematemesis |
| Respiratory distress |
- Abbreviation: IV, intravenous.
The current patient had a Zone II penetrating neck injury and was hemodynamically unstable. Assuming that she had hard signs of vascular injury, we utilized the “zone” approach. Our decision was based on the fact that Zone II injury is the most common among patients with penetrating neck injury, and that vascular injury is a frequent cause of death. However, VAI was discovered fortuitously via implementation of the “zone” approach. One of the two unexpected reasons behind this discovery was that the patient had hypothermia and metabolic acidemia on admission. These conditions can cause unstable hemodynamics. The “triad of death” includes hypothermia due to massive bleeding, subsequent abnormalities in the platelet and coagulation-fibrinolysis system, and metabolic acidemia.7 In general, penetrating injury involving the platysma muscle is suggestive of injury to vital organs.3, 8 In the present case, as there was mild injury to the sternocleidomastoid and platysma muscles, we explored the thyroid gland, trachea, carotid artery, and jugular vein, but found no injuries. As the wound was small and the hematoma was not large, at that time, we did not consider that her hypothermia was caused by massive bleeding due to traumatic injury. She sustained the traumatic injury outside her house, where the ambient air temperature was low. Accordingly, we assumed that her hypothermia and metabolic acidemia were due to the effect of the environmental temperature. Therefore, we made no further observation of the wound, and prioritized the treatment of hypothermia and metabolic acidemia.
An insufficient understanding of the anatomical characteristics also contributed to this lack of predictability. Among penetrating neck injuries, carotid artery injury accounts for 6%–17%, internal jugular vein injury accounts for 9%, and VAI accounts for <1% of injuries.5, 9, 10 It is thought that the low proportion of VAI is because the VA runs along the transverse process and is protected by the cervical vertebrae.1 Furthermore, the anterior aspect of the VA is surrounded by fixed organs (such as the thyroid gland, trachea, and esophagus), muscles, and ligaments. In the present case, we shifted the trachea to the right for wound irrigation, leading to the incidental detection of VAI. It is difficult to control bleeding from the VA.11, 12 The zone approach is the typical strategy for anterior penetrating neck injury and is not generally applied for posterior injuries. Therefore, we recommend that surgeons should not manipulate the posterior portion of the neck without careful consideration before an imaging examination. This is important because VAI may be asymptomatic due to compression by structures located anterior to the VA. In addition, we propose that even simple exposure of the VA for observation should be avoided if patients are hemodynamically stable because if there is injury to the VA, exposure will result in uncontrollable bleeding.
We have no objections to the use of the “no zone” approach with imaging techniques for patients with stable hemodynamics. Surgical treatment should be prioritized for patients who are hemodynamically unstable and have hard signs of vascular injury. However, as in the patient in the present study, those with posterior component injury without anterior component injury may temporarily maintain stable hemodynamics. The “zone” approach is applicable to anterior neck injuries.8 In the present case, although a rare situation, VAI was identified fortuitously by dislocating the esophagus to the right side for wound irrigation. Once the vitals were stable, it was considered that the surgical procedure should be temporarily stopped, and the entire wound should be evaluated by imaging.
4 CONCLUSION
Vertebral artery injury from penetrating neck trauma is rare, and patients with this condition may not present with signs of vascular injury because of anatomical characteristics and concomitant conditions, such as hypothermia and shock. Although the “zone” approach may be useful for the surgical treatment of injuries to the anterior components of the neck by localizing the lesion and controlling the bleeding, the “no zone” approach using imaging techniques should be applied when searching for posterior components, including the VA.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
RI wrote and drafted the manuscript and performed the surgery. GS, YN, and HS drafted the manuscript. SY acquired images. MH administered general anesthesia, performed the surgery, and drafted the manuscript. NH performed the surgery. All authors read and approved the final manuscript.
ETHICAL APPROVAL
The patient gave her informed consent, which has been approved by the institutional committee on human and/or animal research. This protocol has been found acceptable by the institutional committee.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and the related photograph.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




