Radiculopathies caused by spontaneous pneumorrachis: Two case reports and review of literature
Funding information
Not applicable
Abstract
Pneumorarchis is a rare condition of low back pain. It is usually asymptomatic and secondary to trauma. Spontaneous pneumorrachis is scarce.
1 INTRODUCTION
Pneumorrachis is a rare condition. We report two cases of radiculopathy caused by spontaneous pneumorrachis. Patients complain for back pain. The radiological findings showed the intra spinal gas comprising the nerve root. Conservative treatment was sufficient to improve symptom.
Pneumorrachis is a rare phenomenon defined as the presence of intraspinal air. It can be caused by various etiologies, mainly trauma, and medical procedures such as spine surgery or epidural anesthesia. Less common causes of pneumorrachis include spinal infection, tumoral, or degenerative disk diseases. It is usually an asymptomatic and incidental imaging finding. However, it can seldom lead to radicular or spinal nerve compression.1
We report herein two cases of spontaneous pneumorrachis due to degenerative disk disease and discuss the mechanism, diagnosis, and management of this rare condition.
2 CASE 1
A 78-year-old woman presented with a 1-year history of progressive low back mechanical pain associated with low right limb paraesthesia. She has no history of trauma or spinal surgery. The lumbar spine range of motion was limited (Schober's test = 10 mm) and the Leri test was positive. The neuromuscular examination was unremarkable. Biochemical investigations were normal (Table 1).
| Author | Sex |
Age (years) |
Symptoms duration | Spinal location | Neurologicsymptoms | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Bouraoui et al13 | M | 56 | 6 months | L3–L4 | None | Conservative treatment | 4 weeks later: improvement |
| Kim18 | M | 64 | 3 weeks | L5–S1 | Left big toe dorsiflexion weakness | Selective nerve L5 block | 2 months later: clinical improvement and nearly complete disappearance of intraspinal air on CT |
| Giraud et al16 | M | 55 | 4 months | S1 | None | Epidural glucocorticoid injection | 5 months later: complete relief |
| F | 69 | - | L5 | Foot flexor weakness | Conservative treatment | 1 month later: complete relief and improvement of motor deficit | |
| M | 58 | - | S1 | None |
Hemilaminectomy Light disc curettage |
Relapse 1 year later | |
| Tamburelli et al26 | M | 61 | - | L4–L5 | Dysesthesia of the right foot |
Hemilaminectomy Incision of the PLL Foraminotomy |
- |
| Odderson et Matthies17 | M | 73 | 6 months |
L4–L5 S1 Apophyseal joints at L5–S1 level |
None | Conservative treatment |
Complete relief CT: resorption of the intraspinal gas |
| Demierre et al11 | F | 37 | Acute | S1 | Sensory deficit | CT guided aspiration |
Relapse 2 months later. 1st surgery: removal of little disc material Relapse one week later. 2nd surgery: removal of the pseudo-cyst and the PLL 1 year later: free of pain |
| Belfquih et al24 | F | 45 | 9 months | L5–S1 | None | Removal of the pseudo-cyst | 1 year later: complete relief |
| Lee et al12 | F | 76 | 2 years | L4 | Left ankle dorsiflexion weakness |
Hemilaminectomy Removal of the PLL flavectomy |
6 months later: complete relief |
| Impiombato et al19 | F | 85 | 2–3 years | L5 | None | Aspiration under fluoroscopic guidance |
6 months later: complete relief CT: absence of gas |
| Akhaddar et al25 | F | 37 | 6 months | L5 | None | Removal of the pseudo-cyst | Improvement |
| Kumar et al21 | M | 64 | 1 year | L3 | Motor and sensory deficit |
L3 hemilaminectomy Removal of the cyst |
Complete relief |
| Kawaguchi et al27 | F | 60 | 1 month | L3–L4 | Sensory deficit |
Laminectomy Cyst removal |
1 year later: complete relief |
| Bosser et al 10 | F | 62 | 6 months | L5 | None | CT guided aspiration |
Relapse few days later Surgery with complete relief |
| Ricca et al 22 | M | 57 | 1 month | L5–S1 extended to L4 | Sensory deficit |
Removal of the cyst Disc curettage |
Complete relief |
| Song et Lee 15 | M | 72 | 1 month | C7 causing cervical myelopathy | Bilateral motor weakness and sensory deficit of the lower limbs | C7 total laminectomy | 4 weeks later: full recovery |
- Abbreviations: CT, computed Tomography; F, Female; M, Male; PLL, Posterior longitudinal ligament.
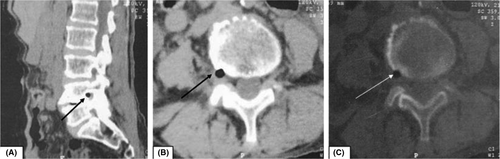
The plain X-ray of the spine showed disk space narrowing at L4-L5 and L5-S1. Computed tomography (CT) visualized a degenerated L4-L5 disk with a vacuum phenomenon as well as a moderate protrusion at L5-S1 space. A gas bubble was noticed in the right lateral recess at L4-L5 with probable evidence of right L4 root compression (Figure 1).
The patient was treated conservatively with analgesics combined with spine rehabilitation.
3 CASE 2
A 61-year-old, retired sheet metal worker, with chronic low back pain presented with a 2-month history of left sciatica that irradiated to the foot in the L5 dermatome. Past medical history was unremarkable. There was no paraesthesia, weakness, or bowel or bladder dysfunction. Physical examination demonstrated a full range of motion. Motor and sensory functions were normal and the straight leg-raising test was positive in the left. Biological tests showed hemoglobin level at 13 g/dl, white blood cell count 7600 elements/mm3, C-reactive protein and erythrocytes sedimentation rate at 5 mg/L and 17 mm; respectively.
Radiographs showed degenerative changes in the lumbar spine. CT scans demonstrated a foraminal disk protrusion with intradiscal gas compressing the left L5 nerve root (Figure 2). The patient improved on conservative management or symptomatic treatment (Table 2).

| Author | Sex |
Age (years) |
Symptoms duration | Spinal location | Neurologicsymptoms | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Konya et al28 | F | 78 | 5 years | L4–L5 | Sensorydeficit | Conservative treatment |
1 year later: moderate improvement CT: persistence of the intraspinal gas |
|
Ryu et al |
M | 72 | 4 weeks | L3–L4 | None | Removal of gas-containing disc and PLL | Complete relief |
| Ovejero30 | F | 64 | 2 years | L2–L3 | Motor and sensory deficit | Laminectomy + Durotomy + removal of disc fragments | 3 years later: improvement of motor weakness, moderate lumbar pain |
| Mortensen et al31 | F | 63 | 1 year | L4–L5 | None | L4–L5 laminectomy + removal of herniated fragment | Improvement |
| M | 65 | 1 year | L5–S1 | Left toe-raising weakness | Laminectomy + left L5–S1 discectomy | Complete relief | |
| M | 55 | 1 year | S1 | Limited flexion and right toe-raising weakness | Surgery |
Improvement Mild weakness |
|
| Mehta et Sharp14 | - | 78 | Acute | L4–L5 | Cauda equina syndrome | L4–L5 laminectomy + wide posterior lumbar spinal decompression |
Improvement of pain Persistence of bowl and bladder dysfunction |
|
Anda et al |
M | 40 | Acute | L5 | Motor and sensory deficit | Conservative treatment | - |
| Pierpaolo et al9 | F | 62 | 3 months | L4–L5 | None | Removal of the herniated disc | Complete relief |
| Pak et al20 | M | 83 | Acute | L5–S1 | none | Aspiration under fluoroscopic guidance | 6 months later: complete relief |
| Cheng et al23 | M | 80 | 6 weeks | L2 | None | Hemilaminectomy + Facectomy of inferior L2 and superior L3 facets on the left side | Complete relief |
- Abbreviations: CT, computed Tomography; F, Female; M, Male; PLL, Posterior longitudinal ligament.
4 DISCUSSION
In addition to trauma causes, other air sources may be found as epidural infection with gas-producing organisms, air introduction via lumbar puncture, or spinal surgery. Relatively rare, the presence of epidural gas in the degenerative spine was reported in a few cases of literature, secondary to vacuum phenomenon.
The vacuum phenomenon is a radiological finding defined as the presence of gaseous collection in the intervertebral disk space resulting from the movement of the spine, especially extension and traction.2 It is a common finding that has been detected or reported in 46% of patients aged over 40 years.3
The intradiscal gas diffuses from the extra-cellular fluid into areas of subatmospheric pressure and it cannot be reabsorbed because the degenerated disk is avascular. Some authors have discussed the role of disk aging in the genesis of the gas.2, 4 This would be due to dehydration and the decrease in the proportion of proteins in the disk.5 The gas is composed of 90%–92% nitrogen along with oxygen, carbon dioxide, and other trace gases.2, 6
The vacuum phenomenon has been mostly observed in L5-S1 disk with decreasing frequency at a higher lumbar level.7
Whereas the vacuum phenomenon is a common finding, the presence of gaseous collection within the spinal canal is unusual. The gas formation is often associated with a disk herniation such as in our second case, but it can also be found free within the spinal canal as in the first case.8, 9
In most previous cases, the gas-containing cyst has been noticed at the level of an intervertebral disk with a vacuum phenomenon suggesting that the gas is originated from the intervertebral disk.10
Interestingly, the gas can migrate to the spinal canal within a degenerated nucleus pulposus, resulting in a gas-containing disk herniation. Otherwise, the gas that fills the disk is expulsed in the spinal canal by a “valve-pump” mechanism through ruptures in the annulus fibrosus and collects under pressure within a fibrous capsule or a pseudo-capsule.6
The histological study of a few cases of free gas noticed that the gas cyst was surrounded by the posterior longitudinal ligament (PLL) suggesting that air coming from the disk was trapped between the PLL and the bone. Furthermore, no recurrence has been observed after the PLL removal.11, 12 Damierre et al. reported the case wherein gas aspiration was failed due to the persistence of pseudo capsules. Surgical removal of membrane proved identical PLL tissue of capsule and improved patient pain.11
Mostly asymptomatic, only a few cases of intraspinal gas can cause compressive radiculopathy. The clinical features are similar to those of common sciatica. Moreover, we can notice an exacerbation of the pain at the change of positions reflecting the free movements of the air in the epidural space.13 Furthermore, only a few cases reported neurological symptoms as lower extremity paresthesia and paralysis. An acute cauda equina syndrome and cervical myelopathy have been reported.14, 15
On standard spine x-rays, we often notice degenerative modifications of the spine and sometimes a vacuum phenomenon.13
CT scan is currently the imaging tool of choice to diagnosis pneumorrachis showing the degenerative modifications of the spine with a vacuum phenomenon and, at the same level, the intraspinal gas collection with a density from −200 to −900 Hounsfield units.16 On MRI, gas is seen in low signal on the T1 and T2 weighted sequences.16
For the management of intraspinal gas, most authors recommend conservative therapy including bed rest, analgesics, non-steroidal anti-inflammatory drugs, myorelaxant drugs, and epidural glucocorticoid injections.16 Intraspinal gas may disappear spontaneously.17, 18 In our cases, we noticed an improvement without using invasive procedures.
Some authors reported the efficacy of the CT-guided aspiration of the gas cyst.19, 20 However, in some cases, intraspinal gas recurred with a relapse of the radicular syndrome.10, 11 Indeed, this procedure does not modify the local environment, and the origin of the air remains.
Surgery is the preferred treatment for patients who failed to respond to conservative therapy. The procedure combines gas evacuation with a disk curettage to prevent recurrence.12, 21-25
5 CONCLUSION
Pneumorrachis caused by degenerative disk disease is a rare condition that can rarely lead to a radicular syndrome. Its prevalence increases with age and it may be due to two mechanisms: a gas-containing disk herniation or an intraspinal free gas. CT scan is the preferred imaging technique. The treatment is conservative at first. CT-guided needle aspiration can be suggested despite the risk of relapse. Surgery remains the treatment of choice in case of neurological signs or recurrence under conservative treatment.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST
None declared.
AUTHORS CONTRIBUTIONS
HLF, KM, DBN, and WT: analyzed and interpreted the patient data and provided advice for treatment. DK ensured the clinical follow-up of the patient. LBA wrote the manuscript; and all authors: read, revised, and approved the final manuscript.
CONSENT
Written informed consent was obtained from the two patients for the publication of this case report.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




