Continuous facial myokymia in multiple sclerosis
Abstract
Facial myokymia is a clinical sign that can occur as a manifestation of demyelinating lesions. As seen in our patient with multiple sclerosis, acute-onset continuous facial myokymia can be indicative of an active lesion and can have localizing value.
A 54-year-old woman with relapsing-remitting multiple sclerosis (MS) presented with 3 days of continuous facial “quivering” after self-discontinuing dimethyl fumarate. Examination revealed continuous right perioral myokymia (Video S1). Figure 1 shows her neuroimaging. She received intravenous methylprednisolone. At 1-month follow-up, facial myokymia (FM) had resolved and dimethyl fumarate was restarted.
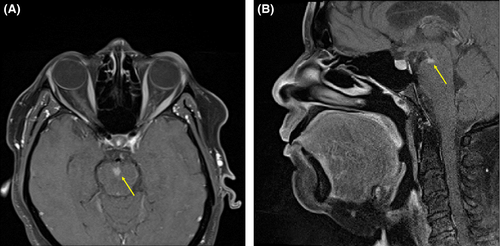
Facial myokymia is an involuntary, abnormal activity consisting of undulating, vermicular movements.1, 2 FM has been associated with lesions of the postnuclear, postgenu portion of the ipsilateral facial nerve intra-axially in the dorsolateral pontine tegmentum.1 However, many cases show no intra-axial demyelination of the facial nerve.2 In MS patients, FM is usually self-limited.2
ACKNOWLEDGMENT
Published with written consent of the patient.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
JLC: contributed to the case concept and design, acquired the data, interpreted the data, and wrote the manuscript. MFV: contributed to the case concept and design, acquired the data, interpreted the data, and wrote the manuscript.