The constrictive consequences of pericardial calcifications
Abstract
A 53-year-old man presented with symptomatic severe pulmonary valve regurgitation. He underwent a diagnostic catheterization. A heavily calcified pericardium and the pressure tracings illustrate typical features of constrictive pericarditis physiology, including the "square root sign." This condition is important to recognize given the progressive nature and poor prognosis if untreated.
A 53-year-old male with a history of surgical pulmonary commissurotomy at the age of 12 presented with progressive shortness of breath, right-sided pleural effusion, and peripheral edema. He was in atrial fibrillation with adequate rate control. Echocardiogram showed normal systolic biventricular function and severe pulmonary regurgitation (dilated right ventricle with signs of volume overload; wide origin color flow regurgitation jet, dense continuous wave signal, steep deceleration [pressure half time 80 ms]). Patient responded well to diuretics and underwent a successful cardioversion, after which rhythm control strategy was pursued. A diagnostic cardiac catheterization was performed in the workup for a pulmonary valve replacement. How should the findings shown in Figure 1 be interpreted?
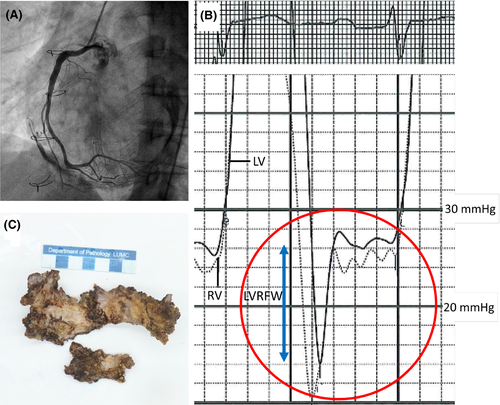
The diagnostic catheterization revealed constrictive pericarditis physiology. Extensive pericardial calcifications were evident during X-ray exposure. Mean right atrial pressure was significantly elevated at 12 mm Hg (SvO2 69%). Simultaneous right (SvO2 67%) and left (SaO2 98%) ventricular pressure tracings revealed diastolic pressure equilibration (23-26 mm Hg) and the pathognomonic "dip and plateau pattern," also known as the "square root sign".1 Left ventricular rapid-filling (LVRFW) wave was accentuated and measured ±10mm Hg. LVRFW > 7mm Hg is representative of the increased early diastolic ventricular filling and is a sensitive marker for constrictive physiology.2 Mean pulmonary artery pressure was 25 mm Hg. Patient had no obstructive coronary artery disease. He underwent a resection of the heavily thickened and calcified pericardium and a pulmonary valve replacement with a homograft. The postoperative recovery period was uneventful, and the patient is currently symptom-free 6 months after the operation.
ACKNOWLEDGMENTS
We greatly acknowledge Mr T. Doeleman for providing the photograph of the specimen in panel C. All procedures performed involving the human participant were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The patient provided consent for publication of this clinical image case.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
AUTHOR CONTRIBUTIONS
All authors were involved in analysis and interpretation of the diagnostic data described in the manuscript, were involved in writing and editing of the manuscript, and have approved the manuscript for submission in its current form.