Intracranial Aneurysmosis with Multilobular Aneurysms and Brain Microaneurysms
A 55-year-old woman with chronic headache underwent magnetic resonance imaging that incidentally identified bilateral irregularly shaped middle cerebral artery (MCA) bifurcation aneurysms. Further characterization with computed tomography angiography and digital subtraction angiography showed multilobular appearances (Fig, A, arrow). Past medical history included Graves' disease, dyslipidemia, and hypertension. She had two cousins with intracranial aneurysms (IAs), but no genetic tests were performed. Four-year surveillance imaging showed stable right MCA aneurysm and increased size of left MCA aneurysm, from 3.7 to 5.5mm in diameter. The patient successfully underwent elective stent-assisted coil embolization of the unruptured left MCA aneurysm (Fig, B, arrow). During recovery, she developed diffuse subarachnoid hemorrhage (SAH), presumably from the left distal M3 branch that showed contrast extravasation on the procedural angiogram (Fig, B, arrowhead). Despite maximum medical and surgical interventions, she died 4 days later. Autopsy neuropathologic examination revealed multiple microaneurysms in several brain regions, including thalamus (Fig, C) and leptomeninges–subarachnoid spaces (Fig, D), as well as cerebellar meningeal vascular malformation (Fig, E, asterisks; Fig, F, magnification of box in E; arrows highlight focal elastic lamina), in addition to the MCA aneurysms and SAH.
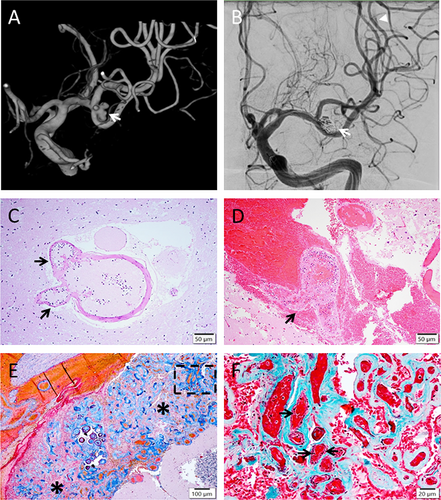
Aneurysmosis is a rare condition characterized by development of diffuse or multiple aneurysms of varying shapes, which is usually seen with connective tissue disorders such as Ehlers–Danlos syndrome, Kawasaki disease, and neurofibromatosis.1-3 The pathophysiology of aneurysmosis is poorly understood, but it is thought to result from various genetic and/or acquired factors leading to arterial wall degeneration and dilatation.1 Eight to 20% of IAs are likely multiple and familial; genetic variations in 9p21 and 19q13 have been linked to increased risk of IAs.2 A few cases of aneurysmosis without genetic and connective tissue disorder have been reported.1-3 Nonhereditary factors of IAs include hypertension, which our patient had, and inflammatory/infectious conditions affecting the vasculature.2, 3 Aneurysmosis has been described typically in the aorta, visceral and intercostal arteries.1-3 While a case report showed concomitant extracranial aneurysms and IAs,2 our case is the first to demonstrate intracranial aneurysmosis with multilobular IAs and multiple brain microaneurysms including Charcot–Bouchard aneurysms and other radiologically undetectable foci, as well as meningeal vascular malformation. Irregular/multilobular shapes of IAs were shown to have the strongest correlation with its rupture, independent of other risk factors, including size, location, and patient-related factors.4 In our case, after successful treatment of an irregular IA, SAH occurred from another site, which suggests a diffuse vascular wall pathology with increased rupture risk not only at the macroscopic sites of IAs, but also grossly normal-appearing distal vessels with aneurysmosis. Our case brings awareness of intracranial aneurysmosis that is potentially associated with irregular IAs, and its increased propensity for intracranial hemorrhage. The treatment of aneurysmosis requires a multidisciplinary approach.1 Endovascular embolization of extracranial aneurysms has shown success in a small number of cases, but it is challenging to feed some distal arteries.3 The detection and management of intracranial aneurysmosis deserve further investigation.
Author Contributions
A.J. contributed to drafting the manuscript and preparing the figure. C.F. and J.-Q.L. contributed to the acquisition and analysis of data. J.-Q.L. contributed to the conception and design of the study.
Potential Conflict of Interest
Nothing to report.