Patterns of treatment in older patients with newly diagnosed advanced bladder cancer: A SEER dataset analysis
Contribution to the manuscript in large part occurred while at the University of Colorado Cancer Center, Cancer Control and Prevention.
Abstract
Background
Bladder cancer is one of the top 10 cancers diagnosed in Americans with a median age of 73. This is the patient population that tends to be older with multiple medical conditions, and previously described variability in treatment in the earlier stages of the disease. This study aimed to evaluate the first-line therapeutic choices for older adults newly diagnosed with advanced bladder cancer. In addition, this work evaluated predictors of response as well as the role of events of functional importance in relation to treatment assignment.
Methods
A population-based cohort study was conducted using the SEER-Medicare database of patients with advanced stage bladder cancer not eligible for curative intent therapy between 2010 and 2013. Patient groups of interest were compared via univariate and multivariate associations. Additionally, a latent class analysis was applied to identify classes with similar features in reference to events of functional importance—events linked to the maintenance or improvement of physical function status.
Results
Within the sample, we noted that a minority of patients received a standard cisplatin-containing regimen (14.77%) and a majority did not receive any chemotherapy (59.69%). Most patients were over age 75. The adjusted odds ratio of no chemo versus cisplatin in patients aged 76 and older compared to patients 66–75 was 6.61 (4.79–9.13; p < 0.0001). We applied latent class analysis methods to the dataset, and three classes demonstrated very low and moderate levels of functional events in the 12 months prior to a person's first outpatient visit for advanced bladder cancer care.
Conclusions
Patients with new diagnosis of advanced bladder cancer largely do not receive the recommended first-line systemic therapy of cisplatin chemotherapy, and a significant majority does not receive any treatment. When evaluating the association between class assignment and predictors of chemotherapy use, such as comorbidity and age, patients with “low usage overall” were more likely to receive chemotherapy. Yet even patients who received chemotherapy had some events of functional importance.
1 INTRODUCTION
Bladder cancer generally affects patients over the age of 65. Most patients are diagnosed with superficial disease, which is curable or highly manageable.1 Yet the patients diagnosed with advanced disease generally face a poor prognosis and limited treatment options. Older adults with advanced bladder cancer are already facing aging-related changes to overall health and functional status and often have multiple comorbid conditions.2 Many patients are unable to receive the preferred standard component of systemic therapy, cisplatin, due to abnormal renal function, functional performance status, hearing deficit, or significant neuropathy.3 Consequently, oncologists alter the chemotherapy regimens to either use carboplatin or forgo the use of platinum altogether. There are data showing the low level of chemotherapy use in the curative-intent perioperative setting, despite evidence supporting its role in improving survival. Small single-institution reports have also reflected low levels of platinum use in advanced disease. Cisplatin-based therapy remains the cornerstone of first-line therapy, even with the emergence of checkpoint inhibitors and antibody drug conjugates. The limited real-world data available show that standard practice is not routinely followed for patients with more limited bladder cancer.4 A population-based understanding of chemotherapy prescribing practices will offer insight into opportunities to further understand and potentially intervene with prescribers.
This generally older population may have extensive heterogeneity in physiologic age and health. Older patients represent a unique population in which a cancer diagnosis oftentimes intersects with concurrent health conditions that are also quite complex. These patients can have underlying health conditions, social considerations, and organ dysfunction that generally hinder or exclude their participation in clinical trials.5 As a result, the available trial data are limited in its true reflection of treatment for this unique group. Geriatric oncology experts recommend a number of considerations when approaching the care of older patients with advanced cancer with the understanding that chronologically older people may have a much different physiologic age due to their functional status, comorbid conditions, and cognition among other things.6
The prospective clinical studies in bladder cancer have traditionally enrolled a younger-than-average population.7 Thus, we aimed to evaluate the systemic treatments patients with advanced bladder cancer in the SEER-Medicare population receive. We grouped these treatments into the receipt of standardized cisplatin, other chemotherapy, or no systemic therapy. At the same time, we aimed to evaluate treatment assignment in association with events of functional importance in order to achieve a real-world sense of prescribing patterns. There are clear considerations that may contribute to treatment assignment such as kidney function and performance status, yet there may also be functional status components that influence treatment planning. Predicting treatment assignment from claims data is a challenge in that variables easily collected in the dataset tend to surface as predictive variables. However, in the clinical care of older persons, physiologic age and functional status are very important factors in deciding upon treatment and these may not be captured clearly in a claims dataset. In order to analyze claims data in a manner that allowed for assessment of classes of patients so that one or two variables would not overshadow the remaining data, we evaluated functional status by identifying events of functional importance and used latent class analysis (LCA) to create subgroups based on patient heterogeneity. Using this approach, we aimed to identify classes of patients with similar patterns for various claims for functional supportive care, and explored how class assignment was associated with treatment. Within each of the treatment groups, we examined healthcare utilization measures and survival in the 12 months after diagnosis as secondary aims of our research. Through an understanding of population-based treatment patterns, future research may then explore how these treatment decisions are made, and identify opportunities to align treatment with the health and values of this complex patient group.
2 METHODS
2.1 Data source
This retrospective analysis was conducted using the Surveillance, Epidemiology, and End Results (SEER)-Medicare database. The database comprised cancer registry data collected by the SEER program, covering approximately 28% of the US population, matched to Medicare enrollment and administrative claims for beneficiaries enrolled in Medicare Fee-for-Service (FFS). The linkage provides demographic and tumor characteristics collected on incident cancer cases, plus covered healthcare services received over the duration of Medicare FFS enrollment. The data used for this analysis contain SEER cases diagnosed from 2010 through 2013 matched to Medicare claims from 2009 through 2014.
2.2 Sample selection
We selected patients whose most recent primary tumor was urinary bladder cancer (SEER Site Recode 29010) diagnosed from 2010 to 2013 (N = 51,123). We further restricted to patients with advanced bladder cancer, which we defined as American Joint Committee on Cancer (AJCC), 6th Edition TNM categories of T4, M1, T3N1, or T3N2 (N = 3613).
To limit the study to patients with complete claims, we restricted to patients age 66 years and older at diagnosis (N = 3024) and excluded patients diagnosed at autopsy or missing diagnosis date (n = 9). To capture comorbidities prior to diagnosis and services received during and after treatment, we required that patients be continuously enrolled in Medicare FFS Part A and Part B from 12 months prior to diagnosis through 12 months following diagnosis, or until death if prior to 12 months (N = 1822). We excluded patients with no paid claims during the study period (n = 11) and kept only patients with treatment consistent with advanced bladder cancer, for a final analysis sample of 1754. This is detailed in Figure 1.

2.3 Measures
We aimed to assess treatment patterns in the delivery of systemic therapy to older people with advanced bladder cancer. Specifically, we aimed to describe whether patients received standardized first-line cisplatin-based therapy; a modified systemic regimen (defined as anything without cisplatin); or no systemic therapy at all. We also evaluated the use of other aspects of cancer care such as radiation, cystectomy, palliative care, and hospice. Additionally, we aimed to better understand the geriatric health of the patients by looking at comorbidity, disability, and functional health by defining “events of functional importance.” Current Procedural Terminology (CPT) codes, Healthcare Common Procedure Coding System (HCPCS) codes, International Classification of Diseases, 9th Revision (ICD-9) procedure and diagnosis codes, and National Drug Codes (NDC) were used to identify cystectomies, chemotherapy, and radiation therapy initiated in the first 6 months of claims following diagnosis (see Appendix). We defined treatment as cisplatin based if at least one claim reported cisplatin, other chemotherapy if at least one claim reported any other chemotherapy agents and no cisplatin, and no chemotherapy if no claims identified chemotherapy. Carboplatin is substituted for cisplatin in some cases, yet is not viewed as first-line standard therapy by many expert panels. Thus, patients receiving carboplatin were categorized as having received modified therapy. Checkpoint inhibitors were not FDA approved for the treatment of advanced bladder cancer during the years analyzed, thus these agents were not included. For patients who died within the 12-month observation period, we also measured hospice use and palliative care. In our survival analysis, we evaluated overall survival, defined as the number of months from diagnosis to death due to any cause.
In addition, we aimed to assess events of functional importance that occurred in the 12 months leading to diagnosis and outpatient follow-up for advanced bladder cancer. We assessed events that signified changes to, or improvement of, functional status. We termed these as “events of functional importance” and they included both acute stays and outpatient services such as durable medical equipment (DME) prescription. We then used latent class analysis to identify any underlying subgroups within this population characterized by multiple functionally focused dimensions.
These events include codes for system utilization that are functionally focused: that is, implemented in response to functional change, implemented to preserve function, or have the potential to impact function. We incorporated DME prescriptions, physical and occupational therapy outpatient services, home healthcare claims, skilled nursing stay, and acute hospital stay. The DME was limited to claims for functionally important assistive devices such as walker or wheelchair, with equipment such as oxygen excluded. Functional assessment drives many oncologic treatment decisions and may offer some insight into differences in physiologic age amongst older persons. Thus, we attempted to enrich our understanding of the functional status of older persons with a recent advanced bladder cancer diagnosis within the limitations of a claims database. We used a latent class analysis to identify subpopulations of patients based on shared patterns in these events of functional importance. With this work, we evaluated the population for any resultant groupings when looking at events of functional importance (use of functionally focused therapies) and subsequent prediction of belonging to our defined treatment groups, including age and comorbidity considerations and how these groupings, or class memberships, predicted treatment group assignment. Classes are constructed to maximize similarity of individuals’ characteristics within a class and dissimilarity of individuals across classes. This provides a picture of the variability among events of functional importance in an older population with a new diagnosis of advanced bladder cancer.
2.4 Covariates
In multivariate analyses, we controlled for year of diagnosis, age at diagnosis, sex, race/ethnicity, marital status, geographic region, population density (metropolitan, non-metropolitan), percent of census tract population below poverty, and TNM category. We also used claims in the 12 months prior to diagnosis to generate measures for baseline health status. To control for prior comorbidities, we used the Charlson Comorbidity Index (CCI).8 To control for baseline functional status, we used a claims-based disability status (DS) measure designed by Davidoff et al. to approximate the Eastern Cooperative Oncology Group (ECOG) performance status measure.9 We used the DS cutoff value determined by Davidoff et al. to dichotomize the patient population into good and poor DS.
2.5 Statistical analysis
To evaluate our primary question of use of systemic therapy, we used chi-square tests to evaluate univariate associations between categorical characteristics and chemotherapy treatment assignment. We used multivariate polytomous logistic regression to obtain adjusted odds ratios (ORs) predicting treatment assignment among all of the covariates. We evaluated differences in survival based on these treatment assignments and produced survival curves using the Kaplan–Meier method. These analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and significance was evaluated at p-value <0.05.
Latent class analysis (LCA) was conducted to identify subpopulations based on shared response patterns to items measuring our aim of outcomes of functional importance. Using this approach, classes of individuals are expected to be similar to one another for the variables of interest, and different from individuals in other classes. The following variables were used as indicators in LCA modeling: (a) inpatient acute stays, categorized as 0 stays, 1 stay, or 2+ stays; (b) inpatient stays in a skilled nursing facility (SNF), yes or no; (c) home health claims, yes or no; (d) physical therapy, yes or no; (e) occupational therapy, yes or no; and (f) any use of durable medical equipment, yes or no. LCA was conducted using Mplus Version 8.6, starting with a one-class model and increasing the number of classes until the best-fitting model was observed. Multiple random perturbations of start values were used for each model, all models converged, there were no negative indications with regard to model identification, and the log likelihood value was replicated for all solutions. Models were evaluated via a variety of metrics assessing absolute and relative fit. Absolute fit was assessed via a likelihood ratio chi-square value. Relative fit indices based on information-heuristic criteria included Akaike's Information Criterion (AIC) and the Bayesian Information Criterion (BIC). Additionally, the Lo–Mendell–Rubin likelihood ratio test (LMR-LRT) was assessed to compare a given k-class model under consideration to a k-1 class, where a significant p-value indicates that the estimated model fits the data significantly better than a model with one fewer class. The three-class model was chosen as the best-fitting model based on model fit indices, and was interpreted further in terms of item homogeneity (individuals within a class responding similarly to a given item, typically reflected by item response probabilities of >0.70 or <0.30), and item separation (individuals in different classes responding distinctly to a given item).
3 RESULTS
The general characteristics of the sample are listed in Table 1. Of the 1754 cases identified according to our search criteria in the years 2010–2013, most patients were male (almost 70%) and older than 75 years old. Most patients were non-Hispanic Whites, and nearly 80% were in areas of low poverty. There was little difference amongst the incidence in each year assessed.
| Total overall | Cisplatin | Other chemo | Supportive care | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Values | N | % | N | % | N | % | N | % | p-Value for other chemo vs. cisplatin | p-Value for supportive care vs. cisplatin |
| All patients | 1754 | 100.00 | 259 | 100.00 | 448 | 100.00 | 1047 | 100.00 | |||
| Age category (years) | 66–75 | 667 | 38.03 | 188 | 72.59 | 191 | 42.63 | 288 | 27.51 | <0.0001 | <0.0001 |
| ≥76 | 1087 | 61.97 | 71 | 27.41 | 257 | 57.37 | 759 | 72.49 | |||
| Sex | Female | 553 | 31.53 | 71 | 27.41 | 134 | 29.91 | 348 | 33.24 | 0.4807 | 0.0722 |
| Male | 1201 | 68.47 | 188 | 72.59 | 314 | 70.09 | 699 | 66.76 | |||
| Race/ethnicity category | White NH | 1455 | 82.95 | 214 | 82.63 | 390 | 87.05 | 851 | 81.28 | 0.2180 | 0.3973 |
| Black NH | 124 | 7.07 | 15 | 5.79 | 23 | 5.13 | 86 | 8.21 | |||
| Other/unknown | 175 | 9.98 | 30 | 11.58 | 35 | 7.81 | 110 | 10.51 | |||
| Registry region at diagnosis | Northeast | 368 | 20.98 | 42 | 16.22 | 106 | 23.66 | 220 | 21.01 | 0.0539 | 0.2180 |
| Midwest | 241 | 13.74 | 37 | 14.29 | 66 | 14.73 | 138 | 13.18 | |||
| South | 372 | 21.21 | 51 | 19.69 | 94 | 20.98 | 227 | 21.68 | |||
| West | 773 | 44.07 | 129 | 49.81 | 182 | 40.63 | 462 | 44.13 | |||
| Patient urban/rural recode category | Metropolitan | 1445 | 82.38 | 213 | 82.24 | 376 | 83.93 | 856 | 81.76 | 0.5617 | 0.8570 |
| Non-metropolitan | 309 | 17.62 | 46 | 17.76 | 72 | 16.07 | 191 | 18.24 | |||
| TNM categories | T3N1 or T3N2 | 150 | 8.55 | 44 | 16.99 | 48 | 10.71 | 58 | 5.54 | 0.0035 | <0.0001 |
| T4 | 576 | 32.84 | 89 | 34.36 | 127 | 28.35 | 360 | 34.38 | |||
| M1 | 1028 | 58.61 | 126 | 48.65 | 273 | 60.94 | 629 | 60.08 | |||
| Charlson Comorbidity Index category | 0 | 733 | 41.79 | 152 | 58.69 | 194 | 43.30 | 387 | 36.96 | <0.0001 | <0.0001 |
| 1 | 402 | 22.92 | 66 | 25.48 | 112 | 25.00 | 224 | 21.39 | |||
| 2 | 225 | 12.83 | 21 | 8.11 | 63 | 14.06 | 141 | 13.47 | |||
| ≥3 | 394 | 22.46 | 20 | 7.72 | 79 | 17.63 | 295 | 28.18 | |||
| Disability status quartile | Other | 1283 | 73.15 | 232 | 89.58 | 371 | 82.81 | 680 | 64.95 | 0.0144 | <0.0001 |
| Highest disability status quartile | 471 | 26.85 | 27 | 10.42 | 77 | 17.19 | 367 | 35.05 | |||
| Radiation therapy in first 6 months | No | 1324 | 75.48 | 194 | 74.90 | 299 | 66.74 | 831 | 79.37 | 0.0228 | 0.1173 |
| Yes | 430 | 24.52 | 65 | 25.10 | 149 | 33.26 | 216 | 20.63 | |||
| Cystectomy in first 6 months | No | 1368 | 77.99 | 155 | 59.85 | 349 | 77.90 | 864 | 82.52 | <0.0001 | <0.0001 |
| Yes | 386 | 22.01 | 104 | 40.15 | 99 | 22.10 | 183 | 17.48 | |||
3.1 Treatment assignment patterns
We divided the outcome of treatment assignment into three groups: patients who had received a standard cisplatin-containing regimen (14.77%); patients who had received some other chemotherapy that was defined as “modified from recommended first line” (25.54%); and patients who had received no chemotherapy (59.69%). We also evaluated patients who had been treated with either radiation or cystectomy within 6 months and found that 5.25% of the cisplatin-treated patients had received cystectomy and 3.02% had received radiation therapy (unknown site). Cystectomy was performed in 4.85% of patients treated with modified chemotherapy and 9.75% in the no-chemotherapy group. Radiation therapy was used in 7.70% of the modified chemotherapy group and 11.63% of the no chemo. There were no significant differences among treatment assignment year to year.
We also assessed predictors of chemotherapy group (standard, modified, none). Thirty-eight percent of patients were aged 66–75. Patients aged 75 years and older were more likely to receive either modified and no chemotherapy versus those aged 66–75, with a nearly inverse proportion among cisplatin and no chemotherapy in the two age groups. The adjusted OR of no chemo versus cisplatin in patients aged 76 and older compared to patients 66–75 was 6.61 (4.79–9.13; p < 0.0001). Additionally, there was a statistically significant difference in treatment group assignment for patients with a CCI score ≥2. These patients were more likely to not receive chemotherapy (p < 0.0001). Patients with a score of two versus zero had an OR of 2.45 (1.40–4.29) for modified chemo versus cisplatin and OR of 2.57 (1.51–4.38) of no chemo versus cisplatin. We also evaluated the DS, as a poor DS score correlates with an Eastern Cooperative Oncology Group performance status of 3 or above. For patients above the poor disability cutoff, the OR for no chemo versus cisplatin was 4.62 (1.80–11.86) and the OR of modified chemotherapy versus cisplatin was 2.20 (0.80–6.00).
3.2 Functional status indicators
We applied latent class analysis methods to the dataset and three classes demonstrated very low and moderate levels of functional events in the 12 months prior to a person's first outpatient visit for advanced bladder cancer care. The entropy value of the three-class model was 0.80, with average posterior class probabilities of 0.87, 0.86, and 0.95 across the three classes, respectively, reflecting good classification certainty. Figure 2 depicts the model-estimated item response probabilities for each of the six indicators of the three-class solution. The first class (n = 84) demonstrated a high proportion of short stays and moderate usage of functional resources such as DME, home health, and even SNF stays. This class had a much higher usage of outpatient physical therapy (PT) and occupational therapy (OT) consultation relative to the other classes and was subsequently labeled as the “more outpatient support class.” The other classes included the “less outpatient support” group (n = 394) with patients who were more highly supported with facility-based functional supports provided by the health system, and less-so outpatient physical and occupational therapy resources. The third class, the largest class by a wide margin, is the “low usage overall” class (n = 1062), demonstrating minimal functional support and minimal facility stays.
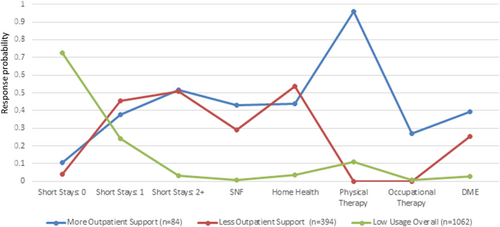
Table 2 presents patient age, CCI, and treatment category in association with class membership. In multinomial logistic regression models, class membership (“more outpatient support” as the reference class) was examined as a predictor of age category (younger age, reference), CCI category (0 [reference], 1, 2, and 3+), and treatment category (cisplatin [reference], other chemo, and no chemotherapy). The “low usage overall” class had the highest proportion of patients under 76 years old, and had the lowest CCI scores. Patients in the “low usage overall” class were most likely to receive cisplatin, or other chemotherapy, with a significant difference in treatment between the “less outpatient support” group. The two groups that received more supportive services had similar treatment distribution, yet the “less outpatient support” class demonstrated more comorbidities and slightly older age relative to the “more outpatient support” class.
| Class 1: more outpatient support | Class 2: less outpatient support | Class 3: low usage overall | Class 1 vs. Class 2 (ref) | Class 3 vs. Class 2 (ref) | ||
|---|---|---|---|---|---|---|
| Age category (years) | 66–75 | 19 (24.4%) | 125 (33.4%) | 430 (43.7%) | Ref | Ref |
| ≥76 | 59 (75.6%) | 249 (66.6%) | 553 (56.3%) | 1.56 (0.89–2.73), p = 0.12 | 0.65 (0.50–0.83), p = 0.0006 | |
| Charlson Comorbidity Index category | 0 | 10 (12.8%) | 92 (24.6%) | 505 (51.4%) | Ref | Ref |
| 1 | 12 (15.4%) | 73 (19.5%) | 260 (26.5%) | 1.51 (0.62–3.7), p = 0.36 | 0.65 (0.46–0.91), p = 0.01 | |
| 2 | 19 (24.4%) | 53 (14.2%) | 104 (10.6%) | 3.30 (1.4–7.6), p = 0.005 | 0.36 (0.24–0.53), p < 0.0001 | |
| ≥3 | 37 (47.4%) | 156 (41.7%) | 114 (11.6%) | 2.18 (1.03–4.6), p = 0.04 | 0.13 (0.10–0.19), p < 0.0001 | |
| Treatment | Cisplatin | 8 (10.3%) | 29 (7.8%) | 208 (21.2%) | Refa | Refa |
| Other chemo | 17 (21.8%) | 89 (23.8%) | 305 (31.0%) | 0.47 (0.18–1.23), p = 0.12 | 0.63 (0.39–1.02), p = 0.06 | |
| No chemotherapy | 53 (67.95%) | 305 (68.5%) | 470 (47.8%) | 0.48 (0.20–1.15), p = 0.10 | 0.38 (0.24–0.59), p = 0.0001 |
- a Comparisons adjust for age and Charlson Comorbidity Index score.
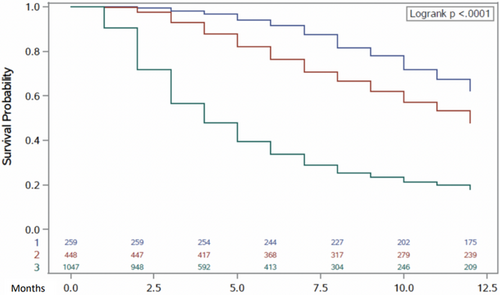
3.3 Survival
Figure 3 demonstrates the survival differences among the three treatment groups. The mean overall survival from diagnosis date for the patients without chemotherapy treatment was 10.67 months (SD 0.1459), 9.47 months (SD 0.1545) for cisplatin-treated patients, and 5.59 months (SD 0.1208) for patients treated with modified chemotherapy. Amongst patients who died, 67% were enrolled on hospice care. Hospice enrollment rates were similar among all treatment groups (Table 3).
| Total overall | Cisplatin | Other chemo | Supportive care | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Values | N | % | N | % | N | % | N | % | p-Value for other vs. cisplatin | p-Value for supportive vs. cisplatin |
| Died within 12-month follow-up | Died | 1189 | 67.79 | 98 | 37.84 | 233 | 52.01 | 858 | 81.95 | 0.0003 | <0.0001 |
| Amongst patients who died: | |||||||||||
| Hospice | None | 388 | 32.63 | 26 | 26.53 | 78 | 33.48 | 284 | 33.10 | 0.2139 | 0.1881 |
| Days | 167 max | 13.62 (mean) | 292 max | 13.71 (mean) | 295 max | 16.93 (mean) | No sig | No sig | |||
| Palliative care | No | 812 | 68.29 | 59 | 60.20 | 147 | 63.09 | 606 | 70.63 | 0.6210 | 0.0336 |
| Yes | 377 | 31.71 | 39 | 39.80 | 86 | 36.91 | 252 | 29.37 | . | . | |
3.4 Health system engagement
We report the admissions to hospital and nursing facilities and most patients were hospitalized at least once. The number of hospital stays was higher in either chemotherapy groups in comparison to the group without any chemotherapy treatment (p < 0.0001), with an increased total number of days in the modified chemotherapy group (mean 17.45 days) versus the no-chemo group (mean 13.79 days). The total number of days in an SNF was significantly higher in the group without chemotherapy treatment compared to the cisplatin-treated group (11.13 vs. 6.51 days; p = 0.0022).
4 DISCUSSION
We examined treatment group assignment for older patients with advanced stage bladder cancer and Medicare coverage over a 3-year period. We noted that a majority of patients did not receive any systemic therapy, and of those who did, it was unlikely to be first-line therapy. We hypothesized that there may be predictors of treatment assignment based on recognized variables, such as age and comorbidity. Yet, we also investigated aspects of functional status or claims that suggested events of potential functional significance, and found that patients with a number of events of functional importance leading to diagnosis were less likely to receive any systemic therapy and certainly cisplatin based.
We noted high variability in the treatment assignment in this older patient group. Age and comorbidity were the strongest predictors of treatment group assignment. Yet there were patients with low comorbidity (by the CCI) and DS who did not receive systemic therapy and patients with high DS and comorbidities who received the most aggressive systemic therapy - cisplatin. Chronologic age seemed a primary driver of treatment assignment regardless of comorbidity or disability, factors that may reflect physiologic age more accurately. Despite an agreed-upon definition of cisplatin eligibility,10 many patients with a poor DS, concordant with an ECOG performance status of 3 or higher, received cisplatin-based therapy. Along these same lines, the group without any chemotherapy had a higher number of localized therapies such as cystectomy or radiation therapy. Radiation therapy may have been administered for palliation of symptoms, but palliative cystectomy is rarely performed, or recommended, given the significant risk of morbidity and mortality. These findings also add to our understanding of the variability treatments among patients with advanced bladder cancer, despite fairly clear guidelines as to systemic and local therapy usage and even approach to the care of older persons with cancer.11, 12 Through this retrospective claims-based review, we are unable to comprehensively assess all potentially relevant patient characteristics, and patient–provider discussions that go into a treatment plan decision, yet the correlation of chronologic age with treatment assignment does suggest aspects of bias in treatment planning. This generates question of how much clinician and patient preference drive treatment assignment.
Consideration of physical function and performance status are highly important when determining a treatment plan for a patient with advanced cancer. In fact, in bladder cancer, platinum ineligibility in part is based on functional status. Patients would benefit from assessment of functional performance status as much as they would from tumor stage and organ function when considering potential therapeutic options with their oncologist. Older patients also base many treatment decisions on functional impact and may choose to forego anticancer therapy in order to maintain functional independence.13 Additionally, we know that cancer-related symptoms and treatments may increase the risks of hospitalization, which in turn may impact functional status. Thus, events of functional importance may heavily influence treatment assignment as well as tolerance of a therapy. Our latent class analysis demonstrated classification of patient groups based on variables that grouped these events of functional importance that had occurred in the 12 months leading up to the first outpatient visit for advanced bladder cancer. This methodology may identify nuanced similarities that would be lost in only univariate or multivariate assessment. When we evaluated the association between class assignment and predictors of chemotherapy use, such as comorbidity and age, patients with “low usage overall” were more likely to receive chemotherapy. Yet even patients who received chemotherapy had some events of functional importance. The patients who engaged in “more outpatient support” had significantly higher CCI scores compared to the other classes. Interestingly, the patients who appeared to have the least need for functional support tended to be younger, with less comorbidity and were more likely to then receive systemic therapy. This suggests that there may have been some consideration of functional status in treatment assignment. Yet does not offer much granularity in considering how physiologic and chronologic ages were assessed. Examining data for all available years, not just the year leading to diagnosis, 86% had a least one inpatient stay, 30% of patients had a stay in a SNF, and 47% had a home health claim. Consequently, these patients are at high risk of either events that may negatively impact function or for interventions to help improve or maintain function.
Most patients in this dataset did not receive any chemotherapy for their diagnosis of an advanced cancer. In this group, the use of acute care support was similar to those on chemotherapy. This taken with the comparable rates of hospice enrollment among all groups would suggest that patients without chemotherapy did not have reduced rates of acute care stays, and there was a nonsignificant mean difference of 3 days in hospice care for this group compared to those on cisplatin. Patients with advanced bladder cancer who are not actively receiving systemic anticancer therapy are eligible for hospice care, which has been shown to improve quality of life, reduce distress at the time of death, and offer support to caregivers and family caring for their loved ones.14, 15 Patients with advanced bladder cancer, not pursuing systemic therapy, did not obviously receive this additional care and there is likely an opportunity to improve the level of supportive care to this population.
Our findings confirm previous research demonstrating limited systemic therapy offerings to patients with urothelial carcinoma. This has been noted in the muscle invasive and advanced settings.16, 17 However, the latent class analysis and events of functional importance provide additional depth to the complexities of patients with advanced bladder cancer. There are some limitations to our work, including examining dates prior to the availability of checkpoint inhibitors for urothelial cancer. These have likely impacted treatment practice patterns. Additionally, due to limitations within the SEER Medicare database, we were not able to analyze patients for cisplatin eligibility within this cohort; performance status is more of a subjective measure of eligibility, which is not captured in this claims dataset. We also did not separate out the variant histologies in bladder primaries, which accounted for 3% of bladder cancer diagnoses in the time period we analyzed. This may have influenced chemotherapy selection, to a degree, although all histologies other than adenocarcinoma would still rely on cisplatin therapy. We limited the follow-up time period to 12 months and the comorbid conditions to the 12 months prior to diagnosis to ensure complete data within the years included. We do not have data on patients who may have previously received therapy for their localized disease, such as neoadjuvant chemotherapy cystectomy or radiation with subsequent recurrence, as we only have data from the time of advanced cancer diagnosis. These patients who received previous neoadjuvant chemotherapy should still be platinum eligible, as more than a year would have passed to recurrence, yet these previous therapies may have influenced subsequent treatment selections. Among these limitations, we hypothesize that these contributed to a small percentage of variability in treatment selected and that the broad differences seen among these groups would not be largely influenced by these infrequent occurrences.
SEER Medicare data do not include patient goals or preferences. Learning of a patient's goals allows for the delivery of goal-concordant care. This model of care delivery accounts for the health conditions of a patient, the preferences and priorities of the patient and then allows the physician and patient to create a care plan together. This approach to caring for a complex older patient population diagnosed with a significant condition is not fully captured in the analysis of the SEER database. However, through this work we identify that those persons who had multiple events of functional importance still received chemotherapy. Additionally, a very low number of patients received hospice care despite not having any systemic therapy and a clearly life-limiting diagnosis. This work has enlightened us to the fact that there is a substantial variability in treatment receipt, as well as some treatment plans that run discordant with other medical conditions and health data. Understanding the patient's goals and values is an important next step in this area of research.
These data reveal a large population of patients with a life-limiting condition receiving care discordant with standard guidelines. These findings also identified age as a primary driver of treatment assignment, suggesting the chronologic age may drive decisions over assessment of physiologic age. This work highlights a need for further research on the treatment planning process, including assessment and communication, in this older and vulnerable patient group. The latent class analysis highlighted the multitude of events of functional importance seen in this population overall, and a clear pattern of treatment assignment appropriate for a population with more events who may then receive less intensive therapy. Bladder cancer is representative of many other tobacco-related malignancies. These data highlight the variability in care for older patients and opportunities to further study treatment assignment and how care may best be aligned.
ACKNOWLEDGMENTS
This project was supported by Population Health Shared Resource, University of Colorado Cancer Center, Grant/Award Number: P30CA046934; National Institutes of Health (NIH)/National Center for Colorado CTSA, Grant Number: 5UL1TR002535-03; Palliative Care Research Cooperative Group funded by the National Institute of Nursing Research, Grant Number: U24NR014637; and American Cancer Society.
CONFLICT OF INTEREST
Elizabeth R. Kessler is an Editorial Board member of Aging and Cancer and a co-author of this article. To minimize bias, they were excluded from all editorial decision-making related to the acceptance of this article for publication.
ETHICS STATEMENT
The authors report no conflicts of interest relative to this work. Additionally, the Colorado Multiple Institution Review Board and determined to not require additional approval.
AUTHOR CONTRIBUTIONS
Study concept and design: Elizabeth R. Kessler, Stacy M. Fischer, and Sarguni Singh. Acquisition of data: Sarguni Singh and Megan Eguchi. Analysis and interpretation of the data: Sarah J. Schmiege, Megan Eguchi, Sarguni Singh, Elizabeth R. Kessler, and Stacy M. Fischer. Drafting the manuscript: Elizabeth R. Kessler, Sarah J. Schmiege, and Stacy M. Fischer. Critical revision of the manuscript: all authors. All authors had full access to the data in the study and take responsibility for the integrity and accuracy of the data and analysis.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the SEER Medicare database. Restrictions apply to the availability of these data, which were used under license for this study.




