Diagnostic test accuracy meta-analysis of PRAME in distinguishing primary cutaneous melanomas from benign melanocytic lesions
Abstract
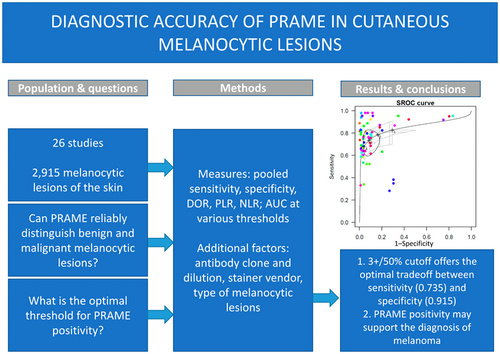
PRAME is a novel immunohistochemical marker that aids the diagnosis of melanocytic lesions. Diffuse PRAME positivity suggests melanoma, whereas benign naevi are negative or only weakly positive. However, the factual diagnostic accuracy of PRAME is not well established. Moreover, some studies have suggested that the threshold of 3+/50% positive cells may be more useful in practice than the most widely used cut-off (4+/75% of positive cells). Hence, we performed a systematic review and diagnostic accuracy meta-analysis to evaluate sensitivity, specificity, likelihood ratios and optimal threshold for PRAME in distinguishing benign melanocytic proliferations from melanomas. Twenty-six studies were enrolled into the meta-analysis. A total of 2915 melanocytic lesions were analysed. The optimal threshold for PRAME positivity was estimated at 3.11, which translates into 3+ in practice. Sensitivity and specificity calculated from SROC at the 3+ threshold were 0.735 (0.631–0.818) and 0.915 (0.834–0.958), respectively, compared to 0.679 (0.559–0.957) and 0.957 (0.908–0.981) at the 4+ cut-off. In subgroup analysis, the spitzoid subgroup was characterised by the lowest sensitivity and diagnostic odds ratio of PRAME. Our findings indicate that PRAME immunohistochemistry may serve as an ancillary marker to support the diagnosis of melanoma. Nevertheless, the accuracy of PRAME may be lower in spitzoid neoplasms. Our meta-analysis suggests that the 3+/50% threshold might be more useful in practice than the 4+/75% cut-off, as it shows higher sensitivity with retained satisfactory specificity.
Graphical Abstract
PRAME immunohistochemistry may serve as an ancillary marker to support the diagnosis of melanoma, but its performance is low in spitzoid lesions. The meta-analysis suggests that the 3+/50% threshold might be more useful in practice than the widely recommended 4+/75%, as it shows higher sensitivity with retained satisfactory specificity.
Conflicts of interest
The authors declare no conflicts of interest.
Open Research
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.