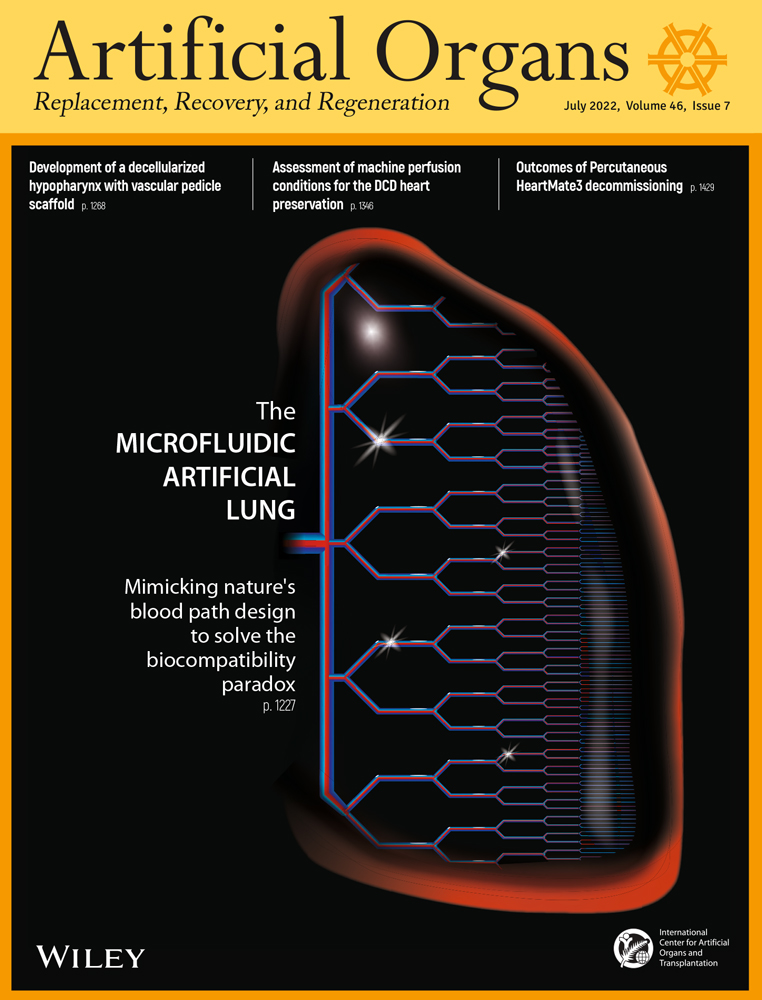
The microfluidic artificial lung: Mimicking nature's blood path design to solve the biocompatibility paradox
Todd L. Astor
Biomembretics, Inc., Boston, Massachusetts, USA
Department of Medicine, Massachusetts General Hospital, Boston, Massachusetts, USA
Search for more papers by this authorCorresponding Author
Jeffrey T. Borenstein
Draper, Cambridge, Massachusetts, USA
Correspondence
Jeffrey T. Borenstein, Bioengineering Division, Draper, 555 Technology Square, Mail Stop 32, Cambridge, MA 02139, USA.
Email: [email protected]
Search for more papers by this authorTodd L. Astor
Biomembretics, Inc., Boston, Massachusetts, USA
Department of Medicine, Massachusetts General Hospital, Boston, Massachusetts, USA
Search for more papers by this authorCorresponding Author
Jeffrey T. Borenstein
Draper, Cambridge, Massachusetts, USA
Correspondence
Jeffrey T. Borenstein, Bioengineering Division, Draper, 555 Technology Square, Mail Stop 32, Cambridge, MA 02139, USA.
Email: [email protected]
Search for more papers by this authorAbstract
The increasing prevalence of chronic lung disease worldwide, combined with the emergence of multiple pandemics arising from respiratory viruses over the past century, highlights the need for safer and efficacious means for providing artificial lung support. Mechanical ventilation is currently used for the vast majority of patients suffering from acute and chronic lung failure, but risks further injury or infection to the patient's already compromised lung function. Extracorporeal membrane oxygenation (ECMO) has emerged as a means of providing direct gas exchange with the blood, but limited access to the technology and the complexity of the blood circuit have prevented the broader expansion of its use. A promising avenue toward simplifying and minimizing complications arising from the blood circuit, microfluidics-based artificial organ support, has emerged over the past decade as an opportunity to overcome many of the fundamental limitations of the current standard for ECMO cartridges, hollow fiber membrane oxygenators. The power of microfluidics technology for this application stems from its ability to recapitulate key aspects of physiological microcirculation, including the small dimensions of blood vessel structures and gas transfer membranes. An even greater advantage of microfluidics, the ability to configure blood flow patterns that mimic the smooth, branching nature of vascular networks, holds the potential to reduce the incidence of clotting and bleeding and to minimize reliance on anticoagulants. Here, we summarize recent progress and address future directions and goals for this potentially transformative approach to artificial lung support.
CONFLICT OF INTEREST
One of the authors (TLA) is the Founder of Biomembretics, Inc., a biomedical company that is developing artificial lung technology related to the content in the manuscript.
REFERENCES
- 1 Global Health Estimates 2020. Deaths by cause, age, sex, by country and by region, 2000-2019. A summary of data sources and methods is available. Geneva: World Health Organization; 2020.
- 2 WHO COVID-19 Dashboard. Geneva: World Health Organization; 2020 [cited 2022 Apr 24]. Available from: https://covid19.who.int/
- 3Goligher EC, Ferguson ND, Brochard LJ. Clinical challenges in mechanical ventilation. Lancet (London, England). 2016; 387: 1856–66.
- 4 No Title [cited 2022 Apr 3]. Available from: https://www.elso.org/Registry/ELSOLiveRegistryDashboard.aspx
- 5 Forum of International Respiratory Societies. The global impact of respiratory disease. 3rd ed. European Respiratory Society; 2021 [cited 2021 Sep 22 ]. Available from: firsnet.org/images/publications/FIRS_Master_09202021.pdf
- 6Broman LM, Taccone FS, Lorusso R, Malfertheiner MV, Pappalardo F, Di Nardo M, et al. The ELSO Maastricht Treaty for ECLS Nomenclature: abbreviations for cannulation configuration in extracorporeal life support—a position paper of the Extracorporeal Life Support Organization. Crit Care. 2019; 23:36.
- 7Yu TZ, Tatum RT, Saxena A, Ahmad D, Yost CC, Maynes EJ, et al. Utilization and outcomes of extracorporeal CO2 removal (ECCO2R): systematic review and meta-analysis of arterio-venous and veno-venous ECCO2R approaches. Artif Organs. 2021; 46: 763–74. https://doi.org/10.1111/aor.14130
- 8Braune S, Sieweke A, Brettner F, Staudinger T, Joannidis M, Verbrugge S, et al. The feasibility and safety of extracorporeal carbon dioxide removal to avoid intubation in patients with COPD unresponsive to noninvasive ventilation for acute hypercapnic respiratory failure (ECLAIR study): multicentre case-control study. Intensive Care Med. 2016; 42: 1437–44.
- 9Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, et al. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet (London, England). 2020; 396: 1071–8.
- 10Barbaro RP, MacLaren G, Boonstra PS, Combes A, Agerstrand C, Annich G, et al. Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international Extracorporeal Life Support Organization Registry. Lancet (London, England). 2021; 398: 1230–8.
- 11Doyle AJ, Hunt BJ. Current understanding of how extracorporeal membrane oxygenators activate haemostasis and other blood components. Front Med. 2018; 5:352.
- 12Sniderman J, Monagle P, Annich GM, MacLaren G. Hematologic concerns in extracorporeal membrane oxygenation. Res Pract Thromb Haemost. 2020; 4: 455–68.
- 13Nagler B, Hermann A, Robak O, Schellongowski P, Buchtele N, Bojic A, et al. Incidence and etiology of system exchanges in patients receiving extracorporeal membrane oxygenation. ASAIO J. 2021; 67: 776–84.
- 14Figueroa Villalba CA, McMullan DM, Reed RC, Chandler WL. Thrombosis in extracorporeal membrane oxygenation (ECMO) circuits. ASAIO J. 2021. https://doi.org/10.1097/MAT.0000000000001605
- 15Davies MG, Hagen PO. Systemic inflammatory response syndrome. Br J Surg. 1997; 84: 920–35.
- 16Adrian K, Mellgren K, Skogby M, Friberg LG, Mellgren G, Wadenvik H. Cytokine release during long-term extracorporeal circulation in an experimental model. Artif Organs. 1998; 22: 859–63.
- 17Graulich J, Sonntag J, Marcinkowski M, Bauer K, Kössel H, Bührer C, et al. Complement activation by in vivo neonatal and in vitro extracorporeal membrane oxygenation. Mediators Inflamm. 2002; 11: 69–73.
- 18Graulich J, Walzog B, Marcinkowski M, Bauer K, Kössel H, Fuhrmann G, et al. Leukocyte and endothelial activation in a laboratory model of extracorporeal membrane oxygenation (ECMO). Pediatr Res. 2000; 48: 679–84.
- 19Millar JE, Fanning JP, McDonald CI, McAuley DF, Fraser JF. The inflammatory response to extracorporeal membrane oxygenation (ECMO): a review of the pathophysiology. Crit Care. 2016; 20: 387.
- 20Kowalewski M, Fina D, Słomka A, Raffa GM, Martucci G, Lo Coco V, et al. COVID-19 and ECMO: the interplay between coagulation and inflammation-a narrative review. Crit Care. 2020; 24: 205.
- 21Gu SX, Tyagi T, Jain K, Gu VW, Lee SH, Hwa JM, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol. 2021; 18: 194–209.
- 22Yusuff H, Zochios V, Brodie D. Thrombosis and coagulopathy in COVID-19 patients requiring extracorporeal membrane oxygenation. ASAIO J. 2020; 66: 844–6.
- 23Zimmerman GA, McIntyre TM, Prescott SM. Thrombin stimulates the adherence of neutrophils to human endothelial cells in vitro. J Clin Invest. 1985; 76: 2235–46.
- 24He T, He J, Wang Z, Cui Z. Modification strategies to improve the membrane hemocompatibility in extracorporeal membrane oxygenator (ECMO). Adv Compos Hybrid Mater. 2021; 4: 847–64.
- 25Rungatscher A, Tessari M, Stranieri C, Solani E, Linardi D, Milani E, et al. oxygenator is the main responsible for leukocyte activation in experimental model of extracorporeal circulation: a cautionary tale. Mediators Inflamm. 2015; 2015:484979.
- 26Novosel E, Borchers K, Kluger PJ, Mantalaris A, Matheis G, Pistolesi M, et al. New approaches to respiratory assist: bioengineering an ambulatory, miniaturized bioartificial lung. ASAIO J. 2019; 65: 422–9.
- 27Burgess KA, Hu HH, Wagner WR, Federspiel WJ. Towards microfabricated biohybrid artificial lung modules for chronic respiratory support. Biomed Microdevices. 2009. https://doi.org/10.1007/s10544-008-9215-2
- 28Kniazeva T, Epshteyn AA, Hsiao JC, Kim ES, Kolachalama VB, Charest JL, et al. Performance and scaling effects in a multilayer microfluidic extracorporeal lung oxygenation device. Lab Chip. 2012; 12. https://doi.org/10.1039/c2lc21156d
- 29Potkay JA. The promise of microfluidic artificial lungs. Lab Chip. 2014. https://doi.org/10.1039/c4lc00828f
- 30Gimbel AA, Hsiao JC, Kim ES, Lewis DJ, Risoleo TF, Urban JN, et al. A high gas transfer efficiency microfluidic oxygenator for extracorporeal respiratory assist applications in critical care medicine. Artif Organs. 2021. https://doi.org/10.1111/aor.13935
- 31Dabaghi M, Rochow N, Saraei N, Fusch G, Monkman S, Da K, et al. A pumpless microfluidic neonatal lung assist device for support of preterm neonates in respiratory distress. Adv Sci Weinheim, Baden-Wurttemberg, Ger. 2020; 7:2001860.
- 32Vedula E, Isenberg B, Santos J, Lai W, Lewis D, Sutherland D, et al. Multilayer scaling of a biomimetic microfluidic oxygenator. ASAIO J. 2022. 68. https://doi.org/10.1097/MAT.0000000000001647
- 33Whitesides GM. The origins and the future of microfluidics. Nature. 2006; 442: 368–73.
- 34Sackmann EK, Fulton AL, Beebe DJ. The present and future role of microfluidics in biomedical research. Nature. 2014; 507: 181–9.
- 35Yager P, Edwards T, Fu E, Helton K, Nelson K, Tam MR, et al. Microfluidic diagnostic technologies for global public health. Nature. 2006; 442: 412–8.
- 36Riahi R, Tamayol A, Shaegh SAM, Ghaemmaghami AM, Dokmeci MR, Khademhosseini A. Microfluidics for advanced drug delivery systems. Curr Opin Chem Eng. 2015; 7: 101–12.
- 37Tandon V, Kang WS, Robbins TA, Spencer AJ, Kim ES, McKenna MJ, et al. Microfabricated reciprocating micropump for intracochlear drug delivery with integrated drug/fluid storage and electronically controlled dosing. Lab Chip. 2016; 16. https://doi.org/10.1039/c5lc01396h
- 38Kaazempur-Mofrad MR, Vacanti J, Krebs N, Borenstein JT. A MEMS-based renal replacement system. Cleveland OH: Transducers Research Foundation; 2004.
- 39Kang JH, Super M, Yung CW, Cooper RM, Domansky K, Graveline AR, et al. An extracorporeal blood-cleansing device for sepsis therapy. Nat Med. 2014; 20: 1211–6.
- 40Borenstein JT, Terai H, King KR, Weinberg EJ, Kaazempur-Mofrad MR, Vacanti JP. Microfabrication technology for vascularized tissue engineering. Biomed Microdevices. 2002; 4. https://doi.org/10.1023/A:1016040212127
- 41Khademhosseini A, Langer R, Borenstein J, Vacanti JP. Microscale technologies for tissue engineering and biology. Proc Natl Acad Sci U S A. 2006; 103. https://doi.org/10.1073/pnas.0507681102
- 42Choi NW, Cabodi M, Held B, Gleghorn JP, Bonassar LJ, Stroock AD. Microfluidic scaffolds for tissue engineering. Nat Mater. 2007; 6: 908–15.
- 43Zhang Y, Yu Y, Chen H, Ozbolat IT. Characterization of printable cellular micro-fluidic channels for tissue engineering. Biofabrication. 2013; 5:25004.
- 44Borenstein JT, Weinberg EJ, Orrick BK, Sundback C, Kaazempur-Mofrad MR, Vacanti JP. Microfabrication of three-dimensional engineered scaffolds. Tissue Eng. 2007; 13. https://doi.org/10.1089/ten.2006.0156
- 45Federspiel W, Henchir K. Encyclopedia of biomaterials and biomedical engineering. Vol. 4, 2nd ed. New York: Marcel Dekker; 2008.
- 46Dornia C, Philipp A, Bauer S, Hoffstetter P, Lehle K, Schmid C, et al. Visualization of thrombotic deposits in extracorporeal membrane oxygenation devices using multidetector computed tomography: a feasibility study. ASAIO J. 2013; 59: 439–41.
- 47Page TC, Light WR, Hellums JD. Oxygen Transport in 10 Micron Artificial Capillaries. In: A Eke, DT Delpy, editors. Oxygen transport to tissue XXI. Advances in Experimental Medicine and Biology. New York: Springer Science; 1999.
10.1007/978-1-4615-4717-4_82 Google Scholar
- 48Potkay JA, Magnetta M, Vinson A, Cmolik B. Bio-inspired, efficient, artificial lung employing air as the ventilating gas. Lab Chip. 2011. https://doi.org/10.1039/c1lc20020h
- 49Hoganson DM, Pryor HI, Bassett EK, Spool ID, Vacanti JP. Lung assist device technology with physiologic blood flow developed on a tissue engineered scaffold platform. Lab Chip. 2011. https://doi.org/10.1039/c0lc00158a
- 50Kniazeva T, Hsiao JC, Charest JL, Borenstein JT. A microfluidic respiratory assist device with high gas permeance for artificial lung applications. Biomed Microdevices. 2011; 13. https://doi.org/10.1007/s10544-010-9495-1
- 51Rochow N, Manan A, Wu WI, Fusch G, Monkman S, Leung J, et al. An integrated array of microfluidic oxygenators as a neonatal lung assist device: in vitro characterization and in vivo demonstration. Artif Organs. 2014. https://doi.org/10.1111/aor.12269
- 52Hendrix RHJ, Ganushchak YM, Weerwind PW. Contemporary oxygenator design: shear stress-related oxygen and carbon dioxide transfer. Artif Organs. 2018. https://doi.org/10.1111/aor.13084
- 53Fernando UP, Thompson AJ, Potkay J, Cheriyan H, Toomasian J, Kaesler A, et al. A membrane lung design based on circular blood flow paths. ASAIO J. 2017; 63: 637–43.
- 54Hall JE. Handbook of Medical Physiology. 14th ed. New York: Elsevier; 2021.
- 55Runyon MK, Kastrup CJ, Johnson-Kerner BL, Van Ha TG, Ismagilov RF. Effects of shear rate on propagation of blood clotting determined using microfluidics and numerical simulations. J Am Chem Soc. 2008. https://doi.org/10.1021/ja076301r
- 56Murray CD. The physiological principle of minimum work: I. The vascular system and the cost of blood volume. Proc Natl Acad Sci U S A. 1926. https://doi.org/10.1073/pnas.12.3.207
10.1073/pnas.12.3.207 Google Scholar
- 57Emerson DR, Cieślicki K, Gu X, Barber RW. Biomimetic design of microfluidic manifolds based on a generalised Murray's law. Lab Chip. 2006. https://doi.org/10.1039/b516975e
- 58Sakariassen KS, Orning L, Turitto VT. The impact of blood shear rate on arterial thrombus formation. Futur Sci OA. 2015. https://doi.org/10.4155/fso.15.28
- 59Santos JA, Gimbel AA, Peppas A, Truslow JG, Lang DA, Sukavaneshvar S, et al. Design and construction of three-dimensional physiologically-based vascular branching networks for respiratory assist devices. Lab Chip. 2021; 21: 4637–51.
- 60Malankowska M, Julian I, Pellejero I, Rho HS, Schlautmann S, Tiggelaar RM, et al. Understanding blood oxygenation in a microfluidic meander double side membrane contactor. Sens Actuators B. 2019; 288: 414–24. https://doi.org/10.1016/j.snb.2019.02.110
- 61Hoganson DM, Anderson JL, Weinberg EF, Swart EJ, Orrick BK, Borenstein JT, et al. Branched vascular network architecture: a new approach to lung assist device technology. J Thorac Cardiovasc Surg. 2010; 140. https://doi.org/10.1016/j.jtcvs.2010.02.062
- 62Wu WI, Rochow N, Chan E, Fusch G, Manan A, Nagpal D, et al. Lung assist device: development of microfluidic oxygenators for preterm infants with respiratory failure. Lab Chip. 2013. https://doi.org/10.1039/c3lc41417e
- 63Lee JK, Kung MC, Kung HH, Mockros LF. Microchannel technologies for artificial lungs: (3) open rectangular channels. ASAIO J. 2008. https://doi.org/10.1097/MAT.0b013e31817eda02
- 64Dharia A, Abada E, Feinberg B, Yeager T, Moses W, Park J, et al. Silicon micropore-based parallel plate membrane oxygenator. Artif Organs. 2018; 42. https://doi.org/10.1111/aor.12972
- 65Matharoo H, Dabaghi M, Rochow N, Fusch G, Saraei N, Tauhiduzzaman M, et al. Steel reinforced composite silicone membranes and its integration to microfluidic oxygenators for high performance gas exchange. Biomicrofluidics. 2018; 12:14107.
- 66Abada EN, Feinberg BJ, Roy S. Evaluation of silicon membranes for extracorporeal membrane oxygenation (ECMO). Biomed Microdevices. 2018. https://doi.org/10.1007/s10544-018-0335-z
- 67Thompson AJ, Ma LJ, Plegue TJ, Potkay JA. Design analysis and optimization of a single-layer PDMS microfluidic artificial lung. IEEE Trans Biomed Eng. 2019. https://doi.org/10.1109/TBME.2018.2866782
- 68Thompson AJ, Marks LH, Goudie MJ, Rojas-Pena A, Handa H, Potkay JA. A small-scale, rolled-membrane microfluidic artificial lung designed towards future large area manufacturing. Biomicrofluidics. 2017; 11. https://doi.org/10.1063/1.4979676
- 69Wagner G, Kaesler A, Steinseifer U, Schmitz-Rode T, Arens J. Comment on “the promise of microfluidic artificial lungs” by J. A. Potkay, Lab Chip, 2014. Lab Chip. 2016; 14: 4122–38. https://doi.org/10.1039/c5lc01508a
- 70Potkay JA. Reply to the “Comment on ‘the promise of microfluidic artificial lungs’” by G. Wagner, A. Kaesler, U. Steinseifer, T. Schmitz-Rode and J. Arens, Lab Chip, 2016, 16, DOI: 10.1039/C5LC01508A. Lab Chip. 2016. https://doi.org/10.1039/c6lc00221h
- 71ASAIO 2021 Annual Meeting Abstracts. ASAIO J. 2021; 67(Suppl 2): 1–155. https://doi.org/10.1097/MAT.0000000000001492
- 72Kovach KM, LaBarbera MA, Moyer MC, Cmolik BL, van Lunteren E, Sen Gupta A, et al. In vitro evaluation and in vivo demonstration of a biomimetic, hemocompatible, microfluidic artificial lung. Lab Chip. 2015; 15: 1366–75.
- 73Thompson AJ, Ma LJ, Major T, Jeakle M, Lautner-Csorba O, Goudie MJ, et al. Assessing and improving the biocompatibility of microfluidic artificial lungs. Acta Biomater. 2020. https://doi.org/10.1016/j.actbio.2020.05.008
- 74Rieper T, Müller C, Reinecke H. Novel scalable and monolithically integrated extracorporeal gas exchange device. Biomed Microdevices. 2015; 17:86.
- 75Mendoza García A, Krane M, Baumgartner B, Sprunk N, Schreiber U, Eichhorn S, et al. Automation of a portable extracorporeal circulatory support system with adaptive fuzzy controllers. Med Eng Phys. 2014; 36: 981–90.
- 76Conway RG, Berk ZB, Zhang J, Li T, Tran D, Wu ZJ, et al. Evaluation of an autoregulatory ECMO system for total respiratory support in an acute ovine model. Artif Organs. 2020; 44: 478–87.
- 77Potkay JA, Thompson AJ, Toomasian J, Lynch W, Bartlett RH, Rojas-Peña A. Toward a servoregulation controller to automate CO2 removal in wearable artificial lungs. ASAIO J. 2021. https://doi.org/10.1097/MAT.0000000000001551