Cutaneous eccrine spiradenoma: Insights into cytomorphological features via fine needle aspiration biopsy and a comprehensive literature review
Abstract
Eccrine spiradenoma (ES) is an uncommon and benign adnexal tumour originating from sweat glands. The cytological examination of ES poses a diagnostic challenge, as it can be mistaken for various benign and malignant basaloid skin neoplasms. The cytomorphologic features of ES are infrequently documented in existing literature. This study seeks to present a thorough exploration of the cytomorphologic traits associated with ES, accompanied by an analysis of ancillary testing that contribute to the accurate identification of this entity in cytological specimens.
Eccrine spiradenoma is infrequently encountered in fine needle aspiration (FNA) cytopathology, and the available literature on its cytomorphologic features is limited. The challenge arises from its similarity to other benign and malignant dermal basaloid neoplasms, emphasizing the critical role of clinicopathologic correlation and immunohistochemical staining in achieving a precise diagnosis.
1 INTRODUCTION
Eccrine Spiradenoma (ES) is a rare benign dermal-based adnexal tumour that was first described in 1956 by Kersting and Helwig.1 ES usually affects adults between 15 and 35 years of age with no gender preference .2 In most cases, ES presents as a solitary asymptomatic nodule predominantly in the head and neck region3 and less commonly encountered in the extremities and trunk.4 ES is usually asymptomatic, although a painful presentation has been described in the literature.5 The precise etiology is unknown and most cases occur sporadically. The clinical presentation of multiple skin lesions and the association of other adnexal tumour types suggest a further assessment for a defect in the CYLDI gene at chromosome 16 at location 12.1 for Brooke-Spiegler syndrome evaluation.6
Due to the rarity of ES occurrence on cytology specimens, limited data regarding its cytomorphologic characteristics have been reported in the literature. Our objective is to present an expanded analysis of the characteristic cytologic features and the immunohistochemical (IHC) staining pattern of ES, along with a discussion on the differential diagnosis of this rare entity on cytology specimens. Furthermore, we aim to provide a literature review of ES cases to highlight the importance of clinicopathologic correlation and histopathological evaluation accompanied by IHC that is essential for an accurate diagnosis.
2 CASE PRESENTATION
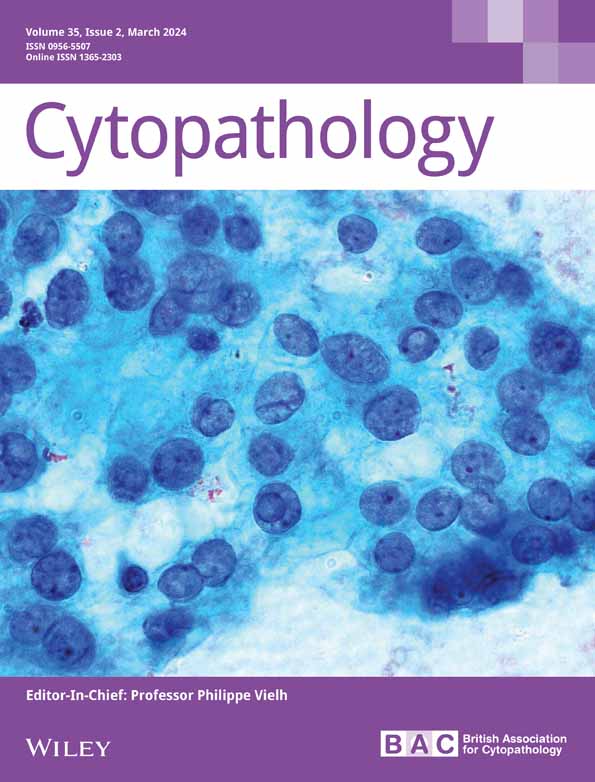
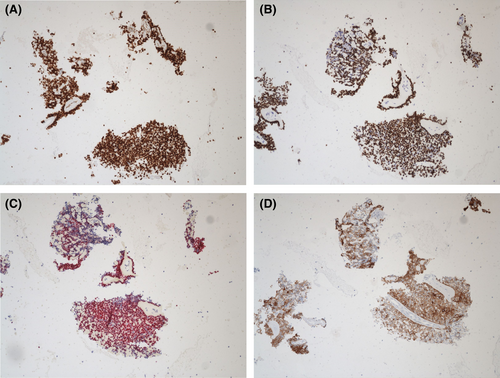
A 75-year-old male with a notable medical history of metastatic malignant melanoma of the posterior base of the neck presented with a new firm, round and smooth nodule on the scalp. Given the patient's history of malignant melanoma, there was a heightened suspicion of a metastatic melanoma prompting the performance of an fine needle aspiration (FNA) biopsy. Cytologic smears and cell block evaluation revealed a cohesive multilayered cluster of biphasic cellular composition, consisting of a round to oval epithelioid cell population with relatively vesicular nuclei and eosinophilic cytoplasm, and few myoepithelial cells with hyperchromatic nuclei and scant cytoplasm. Prominent deposition of thick basement membrane-like material and focal duct formation were noted. No definitive lymphocytes were present. No necrosis or increased mitotic figures activity were noted Figure 1A,B. To further confirm the diagnosis, a panel of IHC stains was performed on the cell block. Positive staining for p40, P63 and SOX-10 was observed, while CK7 showed patchy staining within the tumor cells and ER highlighted scattered cells Figure 2A–D. CK20, PR, Synaptophysin and mCEA showed negative staining Figure 3A–C. A surgical resection of the lesion was performed and showed two distinct cell populations of centrally located large pale cells and small peripherally located dark basaloid cells. The surgical findings correlated with the cytologic findings. The overall findings, in correlation with the clinical presentation and the cytologic findings, supported a diagnosis of ES.

3 DISCUSSION
Rare case reports described ES's FNA cytologic findings. The essential cytomorphologic features of ES include tight multilayered clusters of three-cell populations composed of large cuboidal epithelial cells, spindle-shaped myoepithelial cells and small bland basaloid cells. Prominent basement membrane-like material deposition and occasional T lymphocytes may be seen. Due to the inherent challenges in identifying the dual cell populations within cytology specimens, the utilization of cell block and IHC staining remains essential for accurate identification and characterization. While the luminal epithelial cells show positive expression of the keratins markers such as AE1/3, CAM 5.2, epithelial membrane antigen, CK7 and CK5, the abluminal cells show positive expression of the myoepithelial markers such as p63, smooth muscle actin, calponin and S100. T lymphocytes show expression of T-lymphocyte markers such as CD3 and CD5. The basement membrane-like material deposition can be highlighted with periodic acid-Schiff (PAS) staining. Table 1 demonstrates a review of the clinical presentation, cytomorphologic features and immunohistochemical staining of reported ES cases in the literature.
| Study | Clinical presentation | Cytomorphologic features | Immunohistochemical staining |
|---|---|---|---|
| Sinha et al.34 | A 32-year-old male with complaints of slow growing painful nodular swelling on the back for the last 6 months | Tight multilayered clusters of uniform benign cuboidal epithelial cells along with spindle-shaped myoepithelial cells and occasional lymphocytes. Tumour cells were arranged around perivascular space forming a rosette-like structure | NA |
| Bosch et al.35 | Breast | Bland groups of uniformly sized cuboid cells with scant cytoplasm, round to oval nuclei and inconspicuous nucleoli. Rosette-like structures were noted | NA |
| Kolda et al.36 | Painful mass in the region of the parotid that mimicked an adenoid cystic carcinoma on fine needle aspiration cytology | Three distinct cell types and occasional lymphocytes. Rosette-like structures are noted | NA |
| Punia et al.37 | A 10-year-old female presented with 6 × 6 cm gradually enlarging swelling of the scalp following a trauma 6 years earlier | Hypocellular smears with monomorphic polygonal cells with papilla formation. The nuclei are round and uniform, and the cytoplasm is moderate and clear. No pleomorphism or mitosis is noted. A background of foamy macrophages is seen | NA |
| Punia et al.37 | A 34-year-old female presented with 2.5 × 2.5 irregular slow growing swelling on the left arm for 18 years accompanied by discharge in the last 2 years | NA | NA |
| Rekhi et al.26 | A 28-year-old female presented with multiple swellings in her left shoulder, associated with intermittent pain for 1 year and a half. Radiologic imaging revealed multiple, well-defined, subcutaneous lesions in the left supraclavicular region | Initially diagnosed as Ewing sarcoma. Smears showed cohesive clusters of round to oval cells with scant cytoplasm, focally arranged in an acinar-rosetting pattern around hyaline ‘droplets/bodies’, along with few scattered lymphocytes against a background of red blood cells | NA |
| Panigrahi et al.38 | A 35-year-old male presented with a slow growing painless cutaneous nodule of 1.5 cm size of 6-month duration. On local examination, a single well-defined, freely mobile, non-tender skin nodule was found over the dorsum of the right hand | Fine needle aspiration (FNA) of the swelling yielded particulate material. The cytosmears were highly cellular and showed three populations of cells comprising cohesive clusters of larger cells, discreetly lying larger cells and smaller lymphocyte-like cells. The cohesive cells were larger with round nuclei, pale chromatin and moderate amounts of cytoplasm. Focal rosette-like arrangements were noted. The larger scattered cells were in the form of naked nuclei with fragile cytoplasm giving a glycogenated appearance to the background. The third population of cells was comprised of smaller cells with coarsely clumped clock face-appearing chromatin resembling lymphocytes. There was no mitosis, nuclear atypia or necrosis | NA |
| Satturwar et al.39 |
Case 1: A 68-year-old male with a painless soft tissue mass, clinically recurrent on the arm Case 2: 54-year-old male with slow growing painless, soft tissue mass on the lower leg near the knee for years Case 3: A 62-year-old female presented with slow growing painless soft tissue mass on the ankle for 20 years |
A highly cellular specimen of tightly cohesive loose clusters composed of three cell types of basaloid cells, spindle cells and lymphocytes. Cells were small, round to oval and spindle with scant (pale to eosinophilic) with indistinct cytoplasmic border. Focal rosette-like architecture is noted in all cases. Basement membrane material was noted in two cases. No cytologic atypia, necrosis or mitotic figures were noted in any of the cases | IHC cell block of two cases highlighted dual epithelial cell population. Myoepithelial markers (p63, smooth muscle Actin, calponin and S100) highlighted the abluminal cells and keratins (AE1/3, CAM 5.2, epithelial membrane antigen, CK5 and CK7) highlighted the luminal cells. Desmin, CD34 and ERG (ETS [erythroblast transformation specific]-related gene) stains were negative |
| Our case | A 75-year-old male presented with a new firm, round and smooth nodule on the scalp | Cytologic smears and cell block evaluation revealed a cohesive multilayered cluster of biphasic cellular composition, consisting of a round to oval epithelioid cell population with relatively vesicular nuclei and eosinophilic cytoplasm, and few myoepithelial cells with hyperchromatic nuclei and scant cytoplasm. Prominent deposition of thick basement membrane-like material and focal duct formation were noted. No definitive lymphocytes were present. No necrosis or increased mitotic figures activity were noted | Positive staining for p40, P63 and SOX-10 was observed, while CK7 showed patchy staining within the tumour cells and ER highlighted scattered cells. CK20, PR, Synaptophysin and mCEA showed negative staining |
The differential diagnosis of ES include several benign and malignant entities with overlapping cytologic features with ES. Basaloid carcinomas, such as basal cell carcinoma (BCC) or adenoid cystic carcinoma (AdCC), resemble ES cytologically. 7 However, the presence of clusters of small, oval cells with hyperchromatic nuclei, nuclear atypia and high nuclear-to-cytoplasm ratio and increased mitotic figures in BCC compared to the relatively bland cytology of ES aids in differentiating these two entities.8
Although, rarely encountered on the scalp,9 AdCC, a malignant tumour may resemble ES.10-12 However, AdCC typically displays a cribriform or glandular pattern, with small, uniform cells forming glandular structures when compared to the cohesive clusters of cells with variable cell sizes and shapes in ES. In addition, ES exhibits a combination of basaloid, spindle and epithelioid morphology with bland to mildly pleomorphic nuclei when compared to the small, uniform nuclei with hyperchromasia and nuclear moulding in AdCC. In addition, the presence of numerous hyaline globules and bare nuclei in AdCC aids in differentiating these two entities.13, 14
In the other hand, immunohistochemical staining is valuable in distinguishing between ES and ACC. ES typically shows positive staining for epithelial membrane antigen (EMA), cytokeratin (CK), S100 protein and p63.15 Whereas AdCC commonly expresses CK7, CK14, CK19 and S100 protein, with a characteristic dual positivity for myoepithelial markers such as p63, smooth muscle actin and luminal markers such as CK7 and CK19.
Hidradenoma, another benign cutaneous adnexal tumour that originates from eccrine sweat glands and imitates ES.16 Cytology specimens exhibit cell clusters with tubular formations, globoid or cylindrical clear cells. Necrotic debris, anaplasia and squamous differentiation may be seen in malignant cases.17, 18
Pilomatricoma is characterized by the presence of clusters of basaloid cells exhibiting round to ovoid nuclei, along with nucleated squamous cells.19, 20 Additionally, the characteristic cytoplasmic basophilic granules inclusion of shadow cells (a remnant of shadow cell degeneration) aligns with the typical features of pilomatricoma. Foreign body giant cells may also be observed.
Cylindroma, another benign adnexal tumour may mimic ES on cytology specimens and share similar immunohistochemical staining pattern.21 While ES may exhibit metachromatic-stained hyaline globules or stromal material in the background with prominent lymphocytes,22 cytology of cylindroma is characterized by the presence of clusters of small round to oval basaloid cells with hyperchromatic nuclei attached to abundant magenta coloured acellular hyaline material and lack of T lymphocytes.23 Cell clusters of cylindromas often display nested pattern with jigsaw puzzle arrangement.
Glomus tumours, a benign vascular neoplasm may mimic ES.24 However, the presence of endothelial cells and the lack of dual cell population aid in distinguishing glomus tumours from ES. In addition, the expression of vascular markers such as smooth muscle actin (SMA) and the lack of expression of keratin markers in glomus tumours aids in separating these two entities.24
Metastatic carcinomas or malignant melanoma involving the skin may occasionally mimic ES cytologically.25 However, a thorough evaluation of clinical history, radiological findings and additional ancillary studies may help differentiate between these entities.
Other entities described in the literature that might mimic ES include malignant nerve sheath tumours,26, 27 malignant round cell tumour (Ewing sarcoma reported by Rekhi et al)26 and neuroma.28
Molecular studies aid in differentiating ES from other adnexal tumours that may share certain cytomorphologic features and immunohistochemical staining patterns such as cylindromas and ACCs.21, 29 While ES acquire ALPK1 (alpha kinase 1) gene mutations in 43% of cases and occasional CYLD gene inactivation in approximately 29% of cases; cylindromas tend to acquire CYLD gene inactivation in nearly 100% of cases.29, 30 In the other hand, ACC acquires MYB::NFIB fusion in 73–83% of cases and MYBL1::NFIB fusion in 20–23% of cases.29 Glomus tumors have characteristic NOTCH gene fusion that aid in differentiating this entity from ES.24
Complete local excision is usually curative for ES. However, local recurrence and malignant transformation were reported in some cases.31 The malignant transformation of spiradenoma has been associated with an increase in Ki67 proliferation index rates32 and loss of MYB expression.29, 33
4 CONCLUSION
Eccrine spiradenoma is a rarely encountered entity in FNA cytopathology and there is limited literature on its cytomorphologic features. Due to its resemblance to other benign and malignant dermal basaloid neoplasms, clinicopathologic correlation and immunohistochemical staining play a pivotal role in establishing an accurate diagnosis.
AUTHOR CONTRIBUTIONS
Nada Shaker: Conceptualization; Data curation; Writing—original draft; Writing—review & editing; Poonam Vohra: Conceptualization; Writing—review & editing; Zaibo Li: Conceptualization; Writing—review & editing; Omar P. Sangueza: Conceptualization; Writing—review & editing. Abdul Abid: Conceptualization; Data curation; Writing—original draft; Writing—review & editing.
ACKNOWLEDGEMENTS
Authors acknowledged manuscript submission to the journal.
CONFLICT OF INTEREST STATEMENT
Authors have no conflict of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
Data is available upon request from the corresponding author.