Pyopneumothorax with bronchopleural fistula due to pulmonary infection caused by Porphyromonas gingivalis in a patient with periodontitis
Abstract
Pyopneumothorax with bronchopleural fistula is a rare complication of lung infection. We herein report a case of pyopneumothorax with bronchopleural fistula caused by Porphyromonas gingivalis infection, a common pathogenic pathogen of periodontitis, in a 49-year-old man with periodontitis. The patient was admitted with respiratory failure. Pleural puncture yielded a lot of gas continually and foul-smelling light brown pus, which was found to be caused due to infection with P. gingivalis by the metagenomic next generation sequencing (mNGS) and anaerobic culture.
1 INTRODUCTION
Porphyromonas gingivalis is a widely recognized pathogen leading to periodontitis.1 P. gingivalis was reportedly found in more than 80% of subgingival plaque in patients with periodontitis.2 This bacteria produces a various array of virulence factors, including capsule, lipoplysaccharide, proteolytic enzymes, and fimbriae, and rarely causes extraoral infection, but it once causes extraoral infection, which can lead to severe inflammation, tissue destruction, and sometimes abscess formation.3 Pyopneumothorax with bronchopleural fistula is an infrequent complication of pulmonary infection.4 Pyopneumothorax with bronchopleural fistula is characterized by the accumulation of pus and gas in the chest cavity. It is commonly seen in severe lung infections that invades the pleural cavity.5 To the best of our knowledge, we report the first case of P. gingivalis causing pyopneumothorax with bronchopleural fistula.
2 CASE REPORT
A 49-year-old man with a history of tobacco and alcohol consumption was admitted to the hospital due to cough and sputum for a week and dyspnea for a day. Physical examination indicated a fever (38°C), shortness of breath with pus odor, audible moist rales in both lungs, and low breath sounds in the left lung. He had coughed and produced phlegm, which was light brown purulent sputum. Blood tests showed increased white blood cells (14 700 cells/μL with 92.8% neutrophils) and C-reactive protein (285.6 mg/L). A chest computed tomography scan showed infectious lesions in both lungs, the giant cavity of the left lung with gas and fluid levels (Figure 1A–C).

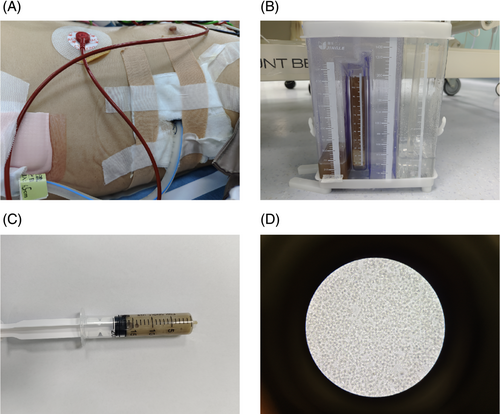
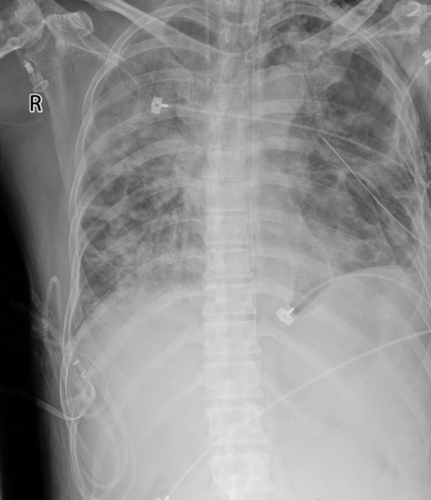
The patient developed respiratory failure and underwent mechanical ventilation with endotracheal intubation and closed thoracic drainage, which produced gas continuously and a large amount of light brown pus with a foul odor (Figure 2A–C). Many pus cells were seen under the microscope after taking pus for smear (Figure 2D). Meanwhile, the pus and peripheral blood were tested for NGS. Based on these findings, a diagnosis of pyopneumothorax was made, Gram-positive suppurative bacterial infection was considered more likely, and intravenous treatment with linezolid was initiated. However, the inflammatory markers continued to rise after 2 days of linezolid anti-infection. Two days later, the NGS results of pus and peripheral blood indicated P. gingivalis positive and P. gingivalis abundance was very high. Then the antibiotic was immediately changed to imipenem (0.5 g q6h) according to the bacterial resistance. Meanwhile, Gram staining of the pus was Gram-negative, and P. gingivalis was cultured in the anaerobic culture of the pus a few days later. The patient had an attack of periodontitis a month ago, which was highly suspected to be the source of the P. gingivalis lung infection. After anti-infective treatment with imipenem, the inflammatory index C-reactive protein and procalcitonin decreased significantly. At the same time, the ventilator support parameters of the patient were reduced, and the blood gas condition improved. The patient's improvement was also evident on the reexamined chest X-ray (Figure 3). However, a large amount of gas continued to escape from the chest closed drainage bottle, and the bronchopleural fistula was considered according to the chest CT upon admission. Unfortunately, the fistula was not located by chest CT. After the patient's condition improved, the tracheal cannula was successfully removed and replaced with the nasal catheter for oxygen inhalation. After a period of conservative treatment, a review of the chest CT revealed a 1.41 mm diameter fistula in the left superior lobe of the lung connecting to the chest cavity (Figure 4A,B). After nearly 3 months of long-term life with the tube, no gas escaped from the chest drainage bottle, and the chest tube was successfully removed.

3 DISCUSSION
P. gingivalis is a kind of Gram-negative anaerobic bacteria, which is widely regarded as the main pathogenic bacteria causing periodontitis. P. gingivalis can enter the lungs by aspiration and cause lung infection. In recent years, more and more studies have found that P. gingivalis is closely related not only to periodontitis and oral squamous cell carcinoma6 but also to inflammatory bowel disease,7 cancer,8 cardiovascular disease,9 Alzheimer's disease,10 rheumatoid arthritis,11 diabetes,12 and other non-oral diseases. An external oral abscess caused by P. gingivalis is rare, but multiple cases of brain abscess13 and one case of lung abscess have been reported. Pyopneumothorax with bronchopleural fistula from P. gingivalis is very rare. A case of empyema and subcutaneous abscess caused by P. gingivalis infection was reported.14 To the best of our knowledge, this case report is the first case of pyopneumothorax with bronchopleural fistula caused by P. gingivalis.
Empyema is the accumulation of pus in the pleural cavity caused by a suppurative infection of the pleural cavity. Pathogenic bacteria can spread to the pleural cavity to cause empyema through pulmonary infection, blood flow, lymphatic vessels, thoracic puncture, and other ways, among which pulmonary infection is more common.15 For the already formed empyema, treatment with antibiotics alone is easy to cause the relapse of empyema. Effective anti-infective treatment should be accompanied by adequate drainage of the abscess, which will have a better prognosis.16 Pus and peripheral blood should be submitted for bacterial culture or genetic testing before antibiotic application and preferably obtained bacterial culture or genetic test results as soon as possible. However, when patients develop large-diameter bronchopleural fistula, conservative treatment is usually ineffective and surgical intervention is required.4
In conclusion, this case report suggests that P. gingivalis can cause severe pulmonary infection and pyopneumothorax with bronchopleural fistula. A recent history of periodontitis is crucial information for clinical treatment.
AUTHOR CONTRIBUTIONS
Jun Sha: Write the article. Jie Shao, Sheng Lu, Wei Yao, Yimai Deng, Jie Chen, and Jianfeng Zhang: Case data collation. Yufeng Feng: Review and revise the article.
ACKNOWLEDGEMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflict of interests. We do not have any possible conflicts of interest.
ETHICS STATEMENT
The case report had been reviewed by the Ethics Committee of Changshu No.2 People's Hospital.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




