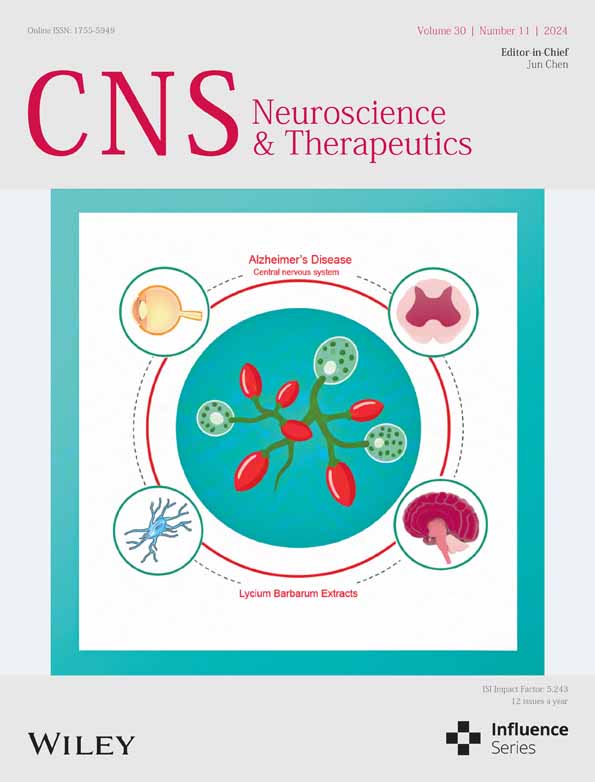
Lycium barbarum Extract Enhanced Neuroplasticity and Functional Recovery in 5xFAD Mice via Modulating Microglial Status of the Central Nervous System
Zhongqing Sun
Department of Neurology, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Innovation Research Institute, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
Department of Orthopaedics and Traumatology, School of Clinical Medicine, Li Kai Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, SAR, China
Search for more papers by this authorJinfeng Liu
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
Search for more papers by this authorZihang Chen
Department of Psychology, The University of Hong Kong, Hong Kong, SAR, China
Department of Sports Medicine, the First Affiliated Hospital, Jinan University, China
Search for more papers by this authorKwok-Fai So
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
State Key Lab of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, SAR, China
Key Laboratory of CNS Regeneration, Guangdong-Hongkong-Macau CNS Regeneration Institute, Ministry of Education, Jinan University, Guangzhou, China
Search for more papers by this authorCorresponding Author
Yong Hu
Department of Orthopaedics and Traumatology, School of Clinical Medicine, Li Kai Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, SAR, China
Orthopedics Center, The University of Hong Kong-Shenzhen Hospital, Shenzhen, China
Correspondence:
Yong Hu ([email protected])
Kin Chiu ([email protected])
Search for more papers by this authorCorresponding Author
Kin Chiu
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
Department of Psychology, The University of Hong Kong, Hong Kong, SAR, China
State Key Lab of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, SAR, China
Correspondence:
Yong Hu ([email protected])
Kin Chiu ([email protected])
Search for more papers by this authorZhongqing Sun
Department of Neurology, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Innovation Research Institute, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
Department of Orthopaedics and Traumatology, School of Clinical Medicine, Li Kai Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, SAR, China
Search for more papers by this authorJinfeng Liu
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
Search for more papers by this authorZihang Chen
Department of Psychology, The University of Hong Kong, Hong Kong, SAR, China
Department of Sports Medicine, the First Affiliated Hospital, Jinan University, China
Search for more papers by this authorKwok-Fai So
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
State Key Lab of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, SAR, China
Key Laboratory of CNS Regeneration, Guangdong-Hongkong-Macau CNS Regeneration Institute, Ministry of Education, Jinan University, Guangzhou, China
Search for more papers by this authorCorresponding Author
Yong Hu
Department of Orthopaedics and Traumatology, School of Clinical Medicine, Li Kai Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, SAR, China
Orthopedics Center, The University of Hong Kong-Shenzhen Hospital, Shenzhen, China
Correspondence:
Yong Hu ([email protected])
Kin Chiu ([email protected])
Search for more papers by this authorCorresponding Author
Kin Chiu
Department of Ophthalmology, School of Clinical Medicine, The University of Hong Kong, Hong Kong, SAR, China
Department of Psychology, The University of Hong Kong, Hong Kong, SAR, China
State Key Lab of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, SAR, China
Correspondence:
Yong Hu ([email protected])
Kin Chiu ([email protected])
Search for more papers by this authorFunding: This work was supported by Joint Founding Project of Innovation Research Institute (LHJJ24JH13). Midstream Research Program for Universities (MRP-092-17X). Health and Medical Research Fund, Hong Kong, China (14151281).
ABSTRACT
Objective
Alzheimer's disease (AD) is the most prevalent neurodegenerative disease with limited treatment options. This study aimed to investigate the effects of Lycium barbarum extract (LBE), a Chinese herb, on the central nervous system (CNS)—including the retina, brain, and spinal cord—in 5xFAD transgenic mice after the onset of AD.
Methods
Starting at 6 months of age, 5xFAD mice received daily intragastric gavage of LBE (2 g/kg) for 2 months. At 8 months, behavioral tests were conducted to assess cognition, motor function, and visual function. These included the Morris water maze, novel object recognition, and Y-maze tests for cognition; the beam walking balance and clasping tests for motor function; and electroretinogram (ERG) for visual function. Immunohistochemistry, western blotting, and ELISA were used to evaluate Aβ deposition, microglial morphology, neuroinflammation, and neuroprotective signaling pathways. Primary microglia and the IMG cell line were used to study LBE's effects on Aβ uptake and degradation in vitro.
Results
After 2 months of LBE treatment, the decline in cognition, motor, and visual functions in 5xFAD mice was significantly slowed. Microglia in the brain, spinal cord, and retina exhibited a neuroprotective state, with reduced Aβ deposition, decreased inflammatory cytokine levels (e.g., TNF-α, IL-1β, IL-6), increased Arg-1/iNOS ratio, and enhanced phagocytic capacity. LBE also promoted Aβ uptake and degradation in primary microglia and the IMG cell line. Neuroprotective signals such as p-Akt, p-Erk1/2, and p-CREB were elevated. Additionally, LBE treatment restored synaptic protein expression and enhanced neuroplasticity.
Conclusion
The findings suggest that LBE treatment can enhance neuroplasticity, reduce systemic inflammation, and improve phagocyte clearance of Aβ deposition via inducing a neuroprotective microglial phenotype throughout CNS. As an upper-class Chinese medicine, appropriate intake of LBE may serve as a beneficial antiaging strategy for AD.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Supporting Information
| Filename | Description |
|---|---|
| cns70123-sup-0001-Figures.docxWord 2007 document , 4.9 MB |
Figure S1. LBE oral feeding restores cognitive memory in 5xFAD mice. (A) The latency for the mice to reach the platform during the first 5 days of trials (n = 25 WT, n = 19 water treatment, n = 21 LBE treatment, **p < 0.01, two-way ANOVA with Tukey's multiple comparison test). (B)Total distance of day 6 in the swimming pool. (C) Mean speed of day 6 in the swimming pool (n = 25 WT group, n = 19 5xFAD group, n = 21 5xFAD + LBE group, one-way ANOVA with Tukey's multiple comparison test). (D) Illustration of the open-field test that measured the exploratory and spontaneous locomotor activity. (E) Time spent in the center of the square box (n = 25 WT group, n = 19 5xFAD group, n = 20 5xFAD + LBE group, Kruskal–Wallis test with Dunn's multiple comparison test). (F) Total distance in the center of the square box (n = 25 WT group, n = 19 5xFAD group, n = 20 5xFAD + LBE group, one-way ANOVA with Tukey's multiple comparison test). (G) Mean traveling speed in the square box (n = 25 WT group, n = 19 5xFAD group, n = 20 5xFAD + LBE group, one-way ANOVA with Tukey's multiple comparison test). (H) Illustration of the NOR test that measured the recognition memory. (I) Time spent on two objectives of the NOR test. (J) Recognition index in the NOR test. Figure S2. LBE oral feeding restores motor movement and retina responses in 5xFAD mice. (A) Representative picture of 5xFAD and WT mice in clasping test. The limbs exhibit clasping with curled toes in the 5xFAD mice at the position of white arrow. The limb clasping test was used to quantify deficits in corticospinal function. (B) Qualify the score of clasping tests. (C) Representative ERG waveform to a scotopic 0.01 cd.s/m2 flash under light adaptation of WT group (dark), 5xFAD (red), and 5xFAD + LBE (blue). (D, E) Scattered plots of the amplitude of a-wave and b-wave in the ERG of different groups under dark adaptation and flash in 0.01 cd.s/m2. (F) Representative ERG waveform to a scotopic 3.0 cd.s/m2 flash under light adaptation of WT group (dark), 5xFAD (red), and 5xFAD + LBE (blue). (G, H) Scattered plots of the amplitude of a-wave and b-wave in the ERG of different groups under dark adaptation and flash in 3.0 cd.s/m2. Figure S3. LBE treatment reduced Aβ load in the brain and spinal cord of 5xFAD mice. (A) Images of brain slices stained for Thio-S (green) labeling Aβ plaques from WT mice. Regions including DG and CA1 of the hippocampus, and cortex are shown in the different rows for WT mice. (B) Images of spinal cord slices stained for Thio-S (green) labeling Aβ plaques from WT mice. Scale bar: 50 μm. Figure S4. LBE treatment reduced Aβ load in the brain 5xFAD mice. (A) Representative image of 4G8 antibody for amyloid plaques in the hippocampus. Qualification of 4G8 protein level in the hippocampus. (B) Representative image of Aβ1-42 antibody for amyloid plaques in the hippocampus. Qualification of Aβ1-42 protein level in the hippocampus. (C) Representative image of 4G8 antibody for amyloid plaques in the cortex. Qualification of 4G8 protein level in the cortex (n = 4 WT group, n = 4 5xFAD group, n = 4 5xFAD + LBE group, one-way ANOVA with Tukey's multiple comparison test). (D) Representative image of 4G8 antibody for amyloid plaques in the spinal cord. Qualification of 4G8 protein level in the spinal cord. (E) Representative image of Aβ1-42 antibody for amyloid plaques in the spinal cord. Qualification of Aβ1-42 protein level in the spinal cord. (F) Representative image of 4G8 antibody for amyloid plaques in the retina. Qualification of 4G8 protein level in the retina (n = 4 WT group, n = 4 5xFAD group, n = 6 5xFAD + LBE group, one-way ANOVA test with Tukey's post hoc test.) ns, not significant. *, p < 0.05; **, p < 0.01. Figure S5. LBE treatment preserved presynaptic density in the CNS of 5xFAD mice. (A) Representative images of antibodies for SYP (presynapse) in brain after LBE treatment. (B) Qualification protein level of SYP in the hippocampus and cortex. Data are shown as mean ± SEM. *p < 0.05; **p < 0.01; ***p < 0.001 by one-way ANOVA test with Dunn's multiple comparison test. Figure S6. LBE treatment preserved postsynaptic density in the CNS of 5xFAD mice. (A) Images of brain slices stained PSD95 (red) labeling presynaptic density from WT, 5xFAD, and 5xFAD + LBE mice. (B) Quantification of the relative density and counts of PSD95-positive dot points in the DG region. (C) Quantification of the relative density and counts of PSD95-positive dot points in the CA1 region. Scale bar: 20 μm. (D) Images of brain slices stained PSD95 (red) labeling presynaptic density from WT, 5xFAD, and 5xFAD + LBE mice. (E) Quantification of the relative density and counts of PSD95-positive dot points in the cortex region. (F) Images of spinal cord slices stained PSD95 (red) labeling presynaptic density from WT, 5xFAD, and 5xFAD + LBE mice. Scale bar: 20 μm. (G) Quantification of the relative density, and counts of PSD95-positive dot points in the spinal cord. (H) Images of retina slices stained for PSD95 (red) labeling presynaptic density merged with DAPI from WT, 5xFAD, and 5xFAD + LBE mice. (I) Quantification of the fluorescence intensity of PSD95-positive in the retina. Scale bar: 20 μm. Data are shown as mean ± SEM. *p < 0.05; **p < 0.01; ***p < 0.001 by one-way ANOVA test with Tukey's multiple comparison test. |
| cns70123-sup-0002-DataS1.pdfPDF document, 1.5 MB |
Data S1. Supporting Information. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
References
- 1F. Leng and P. Edison, “Neuroinflammation and Microglial Activation in Alzheimer Disease: Where Do We Go From Here?,” Nature Reviews. Neurology 17, no. 3 (2021): 157–172.
- 2J. M. Long and D. M. Holtzman, “Alzheimer Disease: An Update on Pathobiology and Treatment Strategies,” Cell 179, no. 2 (2019): 312–339.
- 3L. Jia, M. Quan, Y. Fu, et al., “Dementia in China: Epidemiology, Clinical Management, and Research Advances,” Lancet Neurology 19, no. 1 (2020): 81–92.
- 4C. H. van Dyck, C. J. Swanson, P. Aisen, et al., “Lecanemab in Early Alzheimer's Disease,” New England Journal of Medicine 388, no. 1 (2023): 9–21.
- 5Y. Tang and W. Le, “Differential Roles of M1 and M2 Microglia in Neurodegenerative Diseases,” Molecular Neurobiology 53, no. 2 (2016): 1181–1194.
- 6G. Zhang, Z. Wang, H. Hu, M. Zhao, and L. Sun, “Microglia in Alzheimer's Disease: A Target for Therapeutic Intervention,” Frontiers in Cellular Neuroscience 15 (2021): 749587.
- 7H. Sarlus and M. T. Heneka, “Microglia in Alzheimer's Disease,” Journal of Clinical Investigation 127, no. 9 (2017): 3240–3249.
- 8O. Wirths, H. Breyhan, A. Marcello, M. C. Cotel, W. Bruck, and T. A. Bayer, “Inflammatory Changes Are Tightly Associated With Neurodegeneration in the Brain and Spinal Cord of the APP/PS1KI Mouse Model of Alzheimer's Disease,” Neurobiology of Aging 31, no. 5 (2010): 747–757.
- 9S. Jawhar, A. Trawicka, C. Jenneckens, T. A. Bayer, and O. Wirths, “Motor Deficits, Neuron Loss, and Reduced Anxiety Coinciding With Axonal Degeneration and Intraneuronal Aβ Aggregation in the 5XFAD Mouse Model of Alzheimer's Disease,” Neurobiology of Aging 33, no. 1 (2012): 196.e129–196.e140.
- 10S. Chiquita, A. C. Rodrigues-Neves, F. I. Baptista, et al., “The Retina as a Window or Mirror of the Brain Changes Detected in Alzheimer's Disease: Critical Aspects to Unravel,” Molecular Neurobiology 56, no. 8 (2019): 5416–5435.
- 11F. Liu, J. Zhang, Z. Xiang, et al., “Lycium barbarum Polysaccharides Protect Retina in rd1 Mice During Photoreceptor Degeneration,” Investigative Ophthalmology & Visual Science 59, no. 1 (2018): 597–611.
- 12S. E. Perez, S. Lumayag, B. Kovacs, E. J. Mufson, and S. Xu, “Beta-Amyloid Deposition and Functional Impairment in the Retina of the APPswe/PS1DeltaE9 Transgenic Mouse Model of Alzheimer's Disease,” Investigative Ophthalmology & Visual Science 50, no. 2 (2009): 793–800.
- 13A. L. Manthey, K. Chiu, and K. F. So, “Effects of Lycium barbarum on the Visual System,” International Review of Neurobiology 135 (2017): 1–27.
- 14Y. S. Ho, M. S. Yu, X. F. Yang, K. F. So, W. H. Yuen, and R. C. Chang, “Neuroprotective Effects of Polysaccharides From Wolfberry, the Fruits of Lycium barbarum, Against Homocysteine-Induced Toxicity in Rat Cortical Neurons,” Journal of Alzheimer's Disease 19, no. 3 (2010): 813–827.
- 15Y. Zhou, Y. Duan, S. Huang, et al., “Polysaccharides From Lycium barbarum Ameliorate Amyloid Pathology and Cognitive Functions in APP/PS1 Transgenic Mice,” International Journal of Biological Macromolecules 144 (2020): 1004–1012.
- 16M. Ye, J. Moon, J. Yang, et al., “The Standardized Lycium chinense Fruit Extract Protects Against Alzheimer's Disease in 3xTg-AD Mice,” Journal of Ethnopharmacology 172 (2015): 85–90.
- 17S. Y. Liu, S. Lu, X. L. Yu, et al., “Fruitless Wolfberry-Sprout Extract Rescued Cognitive Deficits and Attenuated Neuropathology in Alzheimer's Disease Transgenic Mice,” Current Alzheimer Research 15, no. 9 (2018): 856–868.
- 18K. Wang, J. Xiao, B. Peng, et al., “Retinal Structure and Function Preservation by Polysaccharides of Wolfberry in a Mouse Model of Retinal Degeneration,” Scientific Reports 4 (2014): 7601.
- 19P. Teng, Y. Li, W. Cheng, L. Zhou, Y. Shen, and Y. Wang, “Neuroprotective Effects of Lycium barbarum Polysaccharides in Lipopolysaccharide-Induced BV2 Microglial Cells,” Molecular Medicine Reports 7, no. 6 (2013): 1977–1981.
- 20J. Xiao, E. C. Liong, Y. P. Ching, et al., “Lycium barbarum Polysaccharides Protect Mice Liver From Carbon Tetrachloride-Induced Oxidative Stress and Necroinflammation,” Journal of Ethnopharmacology 139, no. 2 (2012): 462–470.
- 21Y. K. Zhang, J. Wang, L. Liu, R. C. Chang, K. F. So, and G. Ju, “The Effect of Lycium barbarum on Spinal Cord Injury, Particularly Its Relationship With M1 and M2 Macrophage in Rats,” BMC Complementary and Alternative Medicine 13 (2013): 67.
- 22Z. Q. Sun, J. F. Liu, W. Luo, et al., “Lycium barbarum Extract Promotes M2 Polarization and Reduces Oligomeric Amyloid-β-Induced Inflammatory Reactions in Microglial Cells,” Neural Regeneration Research 17, no. 1 (2022): 203–209.
- 23J. Liu, L. Baum, S. Yu, et al., “Preservation of Retinal Function Through Synaptic Stabilization in Alzheimer's Disease Model Mouse Retina by Lycium Barbarum Extracts,” Frontiers in Aging Neuroscience 13 (2021): 788798.
- 24H. Lian, E. Roy, and H. Zheng, “Protocol for Primary Microglial Culture Preparation,” Bio-Protocol 6, no. 21 (2016): e1989.
- 25R. C. McCarthy, D. Y. Lu, A. Alkhateeb, A. M. Gardeck, C. H. Lee, and M. Wessling-Resnick, “Characterization of a Novel Adult Murine Immortalized Microglial Cell Line and Its Activation by Amyloid-Beta,” Journal of Neuroinflammation 13 (2016): 21.
- 26F. Kosel, J. M. S. Pelley, and T. B. Franklin, “Behavioural and Psychological Symptoms of Dementia in Mouse Models of Alzheimer's Disease-Related Pathology,” Neuroscience and Biobehavioral Reviews 112 (2020): 634–647.
- 27K. Tanaka, S. Nogawa, E. Nagata, et al., “Persistent CREB Phosphorylation With Protection of Hippocampal CA1 Pyramidal Neurons Following Temporary Occlusion of the Middle Cerebral Artery in the Rat,” Experimental Neurology 161, no. 2 (2000): 462–471.
- 28M. R. Walton and I. Dragunow, “Is CREB a Key to Neuronal Survival?,” Trends in Neurosciences 23, no. 2 (2000): 48–53.
- 29M. Amidfar, J. de Oliveira, E. Kucharska, J. Budni, and Y. K. Kim, “The Role of CREB and BDNF in Neurobiology and Treatment of Alzheimer's Disease,” Life Sciences 257 (2020): 118020.
- 30A. Griciuc and R. E. Tanzi, “The Role of Innate Immune Genes in Alzheimer's Disease,” Current Opinion in Neurology 34, no. 2 (2021): 228–236.
- 31W. Cao and H. Zheng, “Peripheral Immune System in Aging and Alzheimer's Disease,” Molecular Neurodegeneration 13, no. 1 (2018): 51.
- 32J. D. Cherry, J. A. Olschowka, and M. K. O'Banion, “Arginase 1+ Microglia Reduce Aβ Plaque Deposition During IL-1β-Dependent Neuroinflammation,” Journal of Neuroinflammation 12 (2015): 203.
- 33C. H. Latta, T. L. Sudduth, E. M. Weekman, et al., “Determining the Role of IL-4 Induced Neuroinflammation in Microglial Activity and Amyloid-β Using BV2 Microglial Cells and APP/PS1 Transgenic Mice,” Journal of Neuroinflammation 12 (2015): 41.
- 34A. Lyons, R. J. Griffin, C. E. Costelloe, R. M. Clarke, and M. A. Lynch, “IL-4 Attenuates the Neuroinflammation Induced by Amyloid-Beta In Vivo and In Vitro,” Journal of Neurochemistry 101, no. 3 (2007): 771–781.
- 35H. Tian, N. Ding, M. Guo, et al., “Analysis of Learning and Memory Ability in an Alzheimer's Disease Mouse Model Using the Morris Water Maze,” Journal of Visualized Experiments 152 (2019).
- 36C. V. Vorhees and M. T. Williams, “Morris Water Maze: Procedures for Assessing Spatial and Related Forms of Learning and Memory,” Nature Protocols 1, no. 2 (2006): 848–858.
- 37N. Curdt, F. W. Schmitt, C. Bouter, et al., “Search Strategy Analysis of Tg4-42 Alzheimer Mice in the Morris Water Maze Reveals Early Spatial Navigation Deficits,” Scientific Reports 12, no. 1 (2022): 5451.
- 38L. Zhong, K. Chiu, G.-S. He, and Y. Xu, “Wolfberry Extract Enhances the Retinal Light Responses of a Mouse Model of Alzheimer's Disease,” Journal of Pharmaceutical and Biomedical Sciences 11, no. 2 (2021).
- 39E. R. Roy, B. Wang, Y. W. Wan, et al., “Type I Interferon Response Drives Neuroinflammation and Synapse Loss in Alzheimer Disease,” Journal of Clinical Investigation 130, no. 4 (2020): 1912–1930.
- 40S. Cohen and M. E. Greenberg, “Communication Between the Synapse and the Nucleus in Neuronal Development, Plasticity, and Disease,” Annual Review of Cell and Developmental Biology 24 (2008): 183–209.
- 41Y. Gao, Y. Wei, Y. Wang, F. Gao, and Z. Chen, “Lycium barbarum: A Traditional Chinese Herb and a Promising Anti-Aging Agent,” Aging and Disease 8, no. 6 (2017): 778–791.
- 42L. Zhou, W. Liao, H. Zeng, Y. Yao, X. Chen, and K. Ding, “A Pectin From Fruits of Lycium barbarum L. Decreases β-Amyloid Peptide Production Through Modulating APP Processing,” Carbohydrate Polymers 201 (2018): 65–74.
- 43J. Meng, Z. Lv, M. Guo, et al., “A Lycium barbarum Extract Inhibits β-Amyloid Toxicity by Activating the Antioxidant System and mtUPR in a Caenorhabditis elegans Model of Alzheimer's Disease,” FASEB Journal 36, no. 2 (2022): e22156.
- 44Y. Dai, J. Guo, B. Zhang, et al., “Lycium barbarum (Wolfberry) Glycopeptide Prevents Stress-Induced Anxiety Disorders by Regulating Oxidative Stress and Ferroptosis in the Medial Prefrontal Cortex,” Phytomedicine 116 (2023): 154864.
- 45L. Xu, L. Yang, H. Xu, et al., “Lycium barbarum Glycopeptide Ameliorates Motor and Visual Deficits in Autoimmune Inflammatory Diseases,” Phytomedicine 129 (2024): 155610.