Cost saving analysis of prediabetes intervention modalities in comparison with inaction using Markov state transition model—A multiregional case study
Abstract
Background
Prediabetes management is a priority for policymakers globally, to avoid/delay type 2 diabetes (T2D) and reduce severe, costly health consequences. Countries moving from low to middle income are most at risk from the T2D “epidemic” and may find implementing preventative measures challenging; yet prevention has largely been evaluated in developed countries.
Methods
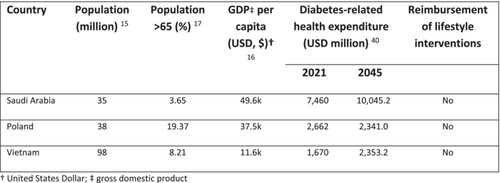
Markov cohort simulations explored costs and benefits of various prediabetes management approaches, expressed as “savings” to the public health care system, for three countries with high prediabetes prevalence and contrasting economic status (Poland, Saudi Arabia, Vietnam). Two scenarios were compared up to 15 y: “inaction” (no prediabetes intervention) and “intervention” with metformin extended release (ER), intensive lifestyle change (ILC), ILC with metformin (ER), or ILC with metformin (ER) “titration.”
Results
T2D was the highest-cost health state at all time horizons due to resource use, and inaction produced the highest T2D costs, ranging from 9% to 34% of total health care resource costs. All interventions reduced T2D versus inaction, the most effective being ILC + metformin (ER) “titration” (39% reduction at 5 y). Metformin (ER) was the only strategy that produced net saving across the time horizon; however, relative total health care system costs of other interventions vs inaction declined over time up to 15 y. Viet Nam was most sensitive to cost and parameter changes via a one-way sensitivity analysis.
Conclusions
Metformin (ER) and lifestyle interventions for prediabetes offer promise for reducing T2D incidence. Metformin (ER) could reduce T2D patient numbers and health care costs, given concerns regarding adherence in the context of funding/reimbursement challenges for lifestyle interventions.
CONFLICT OF INTEREST STATEMENT
Ulrike Gottwald-Hostalek and Nikola Vesic are employees of Merck. The views expressed in this article are the authors' own and do not necessarily reflect the views of the company.