Interventional metabology: A review of bariatric arterial embolization and endovascular denervation for treating metabolic disorders
介入放射学:代谢性疾病治疗手段的新补充
Zhi Wang and Dan-Qi Zhu contributed equally.
Abstract
enThe rising prevalence of metabolic disorders such as obesity and type 2 diabetes mellitus (T2DM) poses a major challenge to global health. Existing therapeutic approaches have limitations, and there is a need for new, safe, and less invasive treatments. Interventional metabolic therapy is a new addition to the treatment arsenal for metabolic disorders. This review focuses on two interventional techniques: bariatric arterial embolization (BAE) and endovascular denervation (EDN). BAE involves embolizing specific arteries feeding ghrelin-producing cells to suppress appetite and promote weight loss. EDN targets nerves that regulate metabolic organs to improve glycemic control in T2DM patients. We describe the current state of these techniques, their mechanisms of action, and the available safety and effectiveness data. We also propose a new territory called “Interventional Metabology” to encompass these and other interventional approaches to treating metabolic disorders.
摘要
zh肥胖和2型糖尿病(T2DM)等代谢性疾病的患病率不断上升给全球健康带来了重大挑战。现有的治疗方法有局限性, 我们需要新的、安全的、创伤较小的治疗方法。代谢性疾病的介入治疗是一种新的治疗手段。本文主要对两种介入技术:减重动脉栓塞术(BAE)和血管内去神经术(EDN)进行综述。BAE通过栓塞特定的动脉造成胃饥饿素下降, 从而抑制食欲和促进体重减轻。EDN靶向调节代谢器官的神经, 改善T2DM患者的血糖控制。我们描述了这些技术的现状、作用机制以及可用的安全性和有效性数据。我们还提出了一个新的领域, 称为“介入性代谢学”, 以涵盖这些和其他介入性治疗代谢性疾病的方法。
1 INTRODUCTION
The prevalence of obesity and type 2 diabetes mellitus (T2DM) is increasing globally,1, 2 with the two conditions sharing essential pathophysiological mechanisms. Obesity is associated with insulin resistance and increased lipid metabolic abnormality, making it one of the major driving factors of the T2DM epidemic.3 T2DM is responsible for 90% of diabetes-related mortality and disability worldwide.2 Although there are various therapeutic strategies for obesity and T2DM, including bariatric surgeries, pharmacotherapies, and lifestyle modification, their efficacy is limited in a number of patients.
Interventional radiology (IR) uses imaging modalities to guide minimally invasive procedures, thus reducing the complications associated with traditional surgery. IR has recently been introduced as a treatment for metabolic disorders, with bariatric arterial embolization (BAE) and endovascular denervation (EDN) emerging as two novel interventional procedures. This review aims to provide the latest evidence for these approaches.
2 BARIATRIC EMBOLIZATION
Behavioral modification, pharmacotherapy, and bariatric surgery are the main therapeutic approaches to obesity, with behavioral modification being the first-line treatment,4 supplemented by pharmacotherapy.5 However, their long-term efficacy is limited.6, 7 Although bariatric surgery is effective for obesity and has a high potentiality in T2DM treatment,8, 9 a number of individuals are ineligible because of their body mass index (BMI).10 Furthermore, its invasiveness may lead to intra- and postoperative problems.11 Other nonpharmaceutical therapies such as endoscopy and interventional bariatric and metabolic therapies offer more options to manage metabolic disorders.
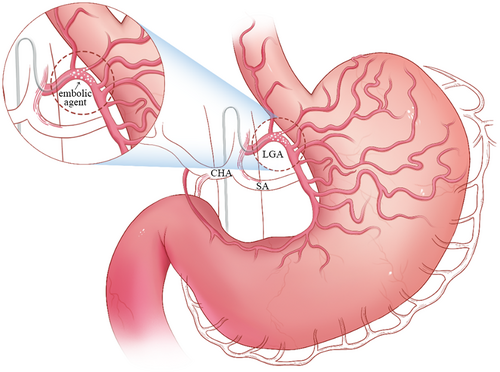
BAE is a novel treatment for obesity with the advantages of less invasiveness, fewer potential complications, and lower costs.12 This procedure includes embolization of the left gastric artery and/or other arteries supplying the fundus using embolic microspheres13, 14 (Figure 1). Currently, various animal experiments and clinical trials have been published to study the safety and efficacy of BAE in treating obesity. The rationale of BAE is to inhibit ghrelin, an orexigenic peptide hormone that increases food intake and promotes positive energy balance,15-19 by embolizing gastric arteries.20-23 The predominance of ghrelin-producing cells in the fundus makes BAE an effective treatment option.24-27 BAE is well tolerated due to the abundant collateral circulation to the stomach, which prevents necrosis and perforation.
2.1 Preclinical and clinical evidence of BAE
BAE is effective in reducing weight and subcutaneous fat, inhibiting ghrelin production, and regulating various metabolic hormones in animal14, 21, 23, 28-31 and human studies.32-39 Preclinical studies using animal models have provided evidence of the feasibility and effectiveness of BAE (Table 1). In 2007, Arepally et al reported early experience using morrhuate sodium as an embolic agent in a swine model and showed that low and high doses can increase or decrease systemic ghrelin levels, respectively.21 Their further investigation demonstrated a short-term persistence of ghrelin and weight gain reduction, with ulcers and gastritis verified by endoscopy.20, 22 Another study by Bawudun and colleagues using a canine model showed a substantial reduction in ghrelin, weight loss, and subcutaneous fat following chemical and polyvinyl alcohol particle embolization.23
| Author (year) | Embolic | Animal model | Weight reduction | Ghrelin suppression | Ulceration rate | Other |
|---|---|---|---|---|---|---|
| Arepally et al (2007)21 | Sodium morrhuate | Swine | Yes | a. Yes | NA | Ghrelin decreased with high dose and increased in low-dose group |
| b. No | ||||||
| a. high dose | ||||||
| b. low dose | ||||||
| Arepally et al (2008)22 | Sodium morrhuate | Swine | Yes | Yes | NA | NA |
| Bawudun et al (2012)23 | a. bleomycin A5 hydrochloride-lipiodol mixture | Canine | Yes | Yes | 0/10 | Subcutaneous fat size measured by computed tomography was significantly reduced |
| b. microspheres (500–700 μm) | ||||||
| Paxton et al (2013)20 | Microspheres (40 μm) | swine | Yes | Yes | 2/5 | All ulcers occurred in nontarget locations. |
| Paxton et al (2014)28 | Microspheres (40 μm) | swine | NA | NA | 2/6 | All treated animals showed minimal to mild sequelae of ischemia in the gastric fundus |
| Pasciak et al (2016)30 | Yttrium-90 microspheres | Swine | Yes | Yes | 5/6 | Three of five had healed superficial mucosal ulcers whereas the other two were predominantly healed with small central crater |
| Kim et al (2017)29 | Microspheres | Swine | No | Yes | 3/5 | Recanalization was noted in three of five animals |
| a. 150–250 μm (n = 3) | ||||||
| b. 50–150 μm (n = 2) | ||||||
| Fu et al (2018)31 | Microspheres | Swine | s | Plasma ghrelin was unchanged in both groups | ||
| a. 100–300 μm | a. Yes | a. Yes | a. 5/5 | |||
| b. 300–500 μm | b. No | b. No | b. 3/5 | |||
| Weiss et al (2020)14 | Radiopaque microspheres (50 μm) | Swine | Yes | Yes | 1/6 | Calibrated Radiopaque microspheres and an antireflux catheter were used. Gastritis was absent in all animals |
Several clinical trials have assessed the safety and effectiveness of BAE in humans (Table 2).21, 33-44 The first-in-human BAE study was described by Kipshidze et al,37 which demonstrated that five patients had reduced appetite and weight after the procedure. Our team also reported 9-month data in five patients and indicated that BAE is a safe and promising strategy for weight loss and abdominal fat reduction.38 Recently, the first randomized, sham-controlled study of BAE demonstrated sustainable weight loss over a 12-month follow-up43 with substantial absolute and percentage total weight reduction as shown in the intention-to-treat and per-protocol analyses. These results provided substantial evidence and support the clinical application of BAE to treat obesity.
| Author (year) | Study design | Patients (n) | Body weight change | Body mass index change | Ghrelin suppression | Dietary consideration | Improvements in Glycemic control | AEs |
|---|---|---|---|---|---|---|---|---|
| Takahashi et al (2019)40 | Retrospective | 16 | −6.4% | −6.3% | NA | NA | NA | NA |
| Kim et al (2018)39 | Retrospective | 21 | −17.5% | −9.4% | NA | NA | NA | NA |
| Gunn and Oklu (2014)41 | Retrospective | 19 vs. 28 | −7.3% vs. −2% (early) | NA | NA | NA | NA | NA |
| −3.5% vs. −0.3% (late) | ||||||||
| Weiss et al (2017)32 | Prospective, single-arm | 5 | −12.8% (3 months) | NA | Yes | Yes | NA | 2 minor AEs |
| Weiss et al (2019)35 | Prospective, single-arm | 20 | −8.2% | NA | NA | No | Yes | 11 minor AEs |
| Zaitoun et al (2019)33 | Prospective, single-arm | 10 | −8.9% | −8.8% | NA | No | Yes | 7 mild epigastric pain |
| Elens et al. (2019)36 | Prospective, single-arm | 16 | −10.0% | −11.8% | NA | No | NA | 1 minor and 1 major AEs |
| Pirlet et al (2019)42 | Prospective, single-arm | 7 | −3.8% | NA | NA | No | NA | 6 mild transient epigastric discomfort |
| Bai et al (2018)38 | Prospective, single-arm | 5 | −7.6% | NA | Yes | Yes | NA | No severe AE |
| Syed et al (2016)34 | Prospective, single-arm | 4 | −7.8% | NA | No | Yes | Yes | No major |
| AE | ||||||||
| Kipshidze et al (2015)37 | Prospective, single-arm | 5 | −17.2% | NA | Yes | NA | NA | NA |
| Reddy et al (2020)43 | Randomized sham-controlled | 22 vs. 22 | −6.4% vs. −2.8% | −6.7% vs. −2.7% | Yes | Yes | NA | 1 serious AE unrelated to the procedure |
2.2 Other metabolic effects of BAE
Weight loss improves glycemic control,45, 46 and several studies explored the metabolic effect of BAE. In a prospective study, BAE improved glycated hemoglobin (HbA1c) from 6% to 4.7% at 6 months post procedure in prediabetic patients.33 Meanwhile, Weiss et al35 reported a decrease in HbA1c at 12 months after BAE, although the improvements in glycemic control were independent of weight reduction. These findings revealed that BAE has the potential for glycemic control and that there may be other mechanisms apart from weight loss contributing to the improvements.
However, several concerns require resolution. First, although minor ulceration is a confirmed adverse event of BAE, whether it will cause functional changes such as gastric emptying and gastric acid secretion requires clarification. Second, although the underlying mechanism of BAE is currently considered to be ghrelin inhibition, the degree of weight reduction is not always correlated with ghrelin reduction. Finally, the potential role of BAE in glycemic control and its underlying mechanism requires further exploration. Recently, our team conducted a canine model experiment and found that, in addition to weight loss, which is one of the hypoglycemic mechanisms, BAE may contribute to delayed gastric emptying and therefore improve postprandial glucose excursion (unpublished). Despite this, further animal experiments and clinical trials are necessary before BAE becomes a widely used approach to treating morbid obesity and related metabolic disorders.
3 ENDOVASCULAR DENERVATION
The primary goal of treating T2DM is to control glycemia. Modulating the sympathetic nervous system (SNS), whose overactivation contributes to metabolic disorders, is a potential therapeutic strategy. Catheter-based renal denervation (RDN) is a novel procedure that directly targets the SNS, but its efficacy in treating T2DM is inconsistent and not reproducible across studies. To target hepatic and islet innervation instead of renal nerves, we introduced denervation at the celiac and hepatic arteries, known as EDN, and explored the safety and efficacy in treating T2DM.47
3.1 The rationale for EDN
T2DM is often accompanied by SNS overactivation, exacerbating hyperglycemia and increasing the risk of complications.48, 49 The central nervous system regulates glucose metabolism through the direct innervation of organs by autonomic nerves. These nerves release neurotransmitters and neuropeptides to control hormone secretion, glucose synthesis, and metabolism.
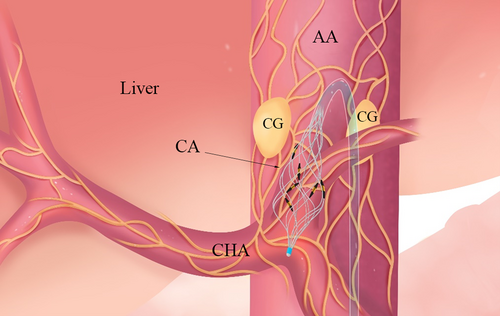
Islets are densely innervated by sympathetic fibers that rapidly increase blood glucose levels by inhibiting glucose-stimulated insulin secretion and stimulating glucagon secretion.50, 51 Meanwhile, the liver receives sympathetic innervation via the celiac and superior mesenteric ganglia52 (Figure 2). Hepatic sympathetic activity increases circulating glucose by promoting glycogenolysis and inhibiting glycogen synthesis.53 Consequently, the crosstalk between nerves and metabolic organs opens up an area for detailed studies on nerve modulation to regulate glucose metabolism and treat metabolic dysfunction.
RDN was first introduced to treat resistant hypertension and now enables selective denervation of the kidney. Although additional potential benefits such as metabolic improvements have been described in some small-scale studies,54, 55 the outcomes vary across studies and are not always reproducible. For instance, the Denervation of the Renal Arteries in Metabolic Syndrome (DREAMS) study showed that RDN did not lead to a significant improvement in insulin sensitivity.56 A systematic review including 19 relevant studies suggested that although blood lipids were slightly improved, RDN appeared to have a negligible impact on metabolic parameters.57 Due to the lack of robust evidence that RDN could improve glycemic control, our team sought a new denervation site that could directly control metabolic organs such as the islet and liver.47 Neuromodulation of the sympathetic nerves of the islet and liver has demonstrated metabolic benefits, making denervation along the celiac and hepatic arteries a more reasonable option.
3.2 The preclinical evidence of hepatic denervation
Early research demonstrated that celiac ganglionectomy improved glucose tolerance in rats,58 and surgical or chemical sympathetic denervation of the common hepatic artery improves glucose tolerance and postprandial glucose clearance.59 Hurr et al60 showed that liver sympathetic nerve activity increased in the obese mice, and hepatic steatosis was alleviated by sympathetic denervation. Kraft et al59 established that surgical sympathetic denervation of the common hepatic artery in a canine model decreased both the hepatic and β-cell defects caused by a high-fat, high-fructose diet, thereby increasing glucose tolerance. Kiuchi et al61 investigated the feasibility, safety, and efficacy of EDN of both hepatic and renal arteries in a swine model, achieving significant and sustained denervation without major safety events. Tzafriri et al62 analyzed the nerves and adjacent anatomies surrounding the human common hepatic artery to guide the clinical translation of catheter-based denervation. They found that the hepatic artery is a rich and accessible target for sympathetic denervation. Recently, we used the high-fat, high-fructose canine model to study how EDN affects glucose metabolism. We found that EDN resulted in significant periarterial nerve injury and decreased tissue norepinephrine. Similar to hepatic surgical denervation, EDN led to a prominent increase of glucose tolerance by enhancing insulin secretion and improving insulin sensitivity of glucose disposal (unpublished). These results may provide further rationale for the clinical application of EDN.
3.3 The preliminary clinical evidence of EDN
Based on the preclinical evidence, we applied a minimally invasive, catheter-based EDN procedure at the celiac artery and aorta around the celiac artery to treat T2DM.47 We registered the first-in-human study on ClinicalTrials.gov (NCT04086043) and reported the feasibility and safety of EDN in 11 patients with T2DM, as well as its initial efficacy. In our study, both HbA1c levels and homeostatic model assessment of insulin resistance were significantly reduced at 6 months (9.9% vs. 8.0%, p = .005; 13.3 vs. 6.0, p = .016). Additionally, we observed decreases in fasting plasma glucose and 2-hour-postprandial glucose levels (227.2 vs. 181.8 mg/dL, p < .001; 322.2 vs. 205.2 mg/dL, p = .001). Furthermore, EDN improved β-cell function and led to a reduced insulin dosage. Surprisingly, we also observed an improvement in liver function (alanine transaminase, 31.0 vs. 24.0 U/L, p = .014; gamma-glutamyl transferase, 47.0 vs. 27.0 U/L, p = .021). We did not find significant changes in blood lipids (triglyceride, 4.4 vs. 3.6 mmol/L, p = .244; total cholesterol, 5.1 vs. 4.6 mmol/L, p = .157). However, the metabolic benefits were not associated with changes in body weight, body mass index, or waist circumference (p > .05). Our study provides the first evidence of the clinical efficacy of EDN in treating T2DM. As a pilot study with a relatively simple design, we further initiated well-designed studies to validate the efficacy and elucidate the clinical mechanism (NCT05631561, NCT05673668).
Before more applications of EDN, it is important to address several issues. First, the dose–response relationship requires clarification. Research has been conducted to study the optimal ablation parameters in RDN, and similar extensive data are needed for radiofrequency ablation in the celiac and hepatic arteries. Second, due to the comprehensive innervation of celiac sympathetic nerves, the effects on different organs need to be clearly understood to optimize ablation sites and reduce complications. Last, the long-term effects of EDN have not yet been evaluated. Therefore, further preclinical experiments and clinical trials are still required to fully understand the potential risks and benefits of EDN.
4 CONCLUSION
IR offers a series of treatment options for metabolic disorders, leading us to propose a new territory named “interventional metabology.” The effect of BAE and EDN in combination with lifestyle intervention, pharmaceutical, and other treatments, as well as the comparison with standard care for obesity and T2DM are also arousing interest. Although reasonably safe, BAE and EDN require further investigation for unresolved issues and high-class evidences.
ACKNOWLEDGEMENTS
This work was supported by grants from the National Natural Science Foundation of China (61821002 to Gao-Jun Teng, 82170845 to Ling Li, 82200929 to Xiang-Yun Zhu, and 82000740 to De-Chen Liu)
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interest.




