Osteopoikilosis—the incidental finding of a rare bone dysplasia: A case report
Abstract
Key Clinical Message
Osteopoikilosis is an asymptomatic osteosclerotic dysplasia, of autosomal dominant inheritance, which does not cause deformity or alteration in bone development, of incidental diagnosis. The differential diagnosis should be made with osteoblastic metastases, among others, especially if it is asymmetric and in patients over 50 years of age.
Osteopoikilosis is a rare benign bone disease, characterized by the appearance of bone islands in the osseous tissue, which could be confused with bone metastasis. We present the case of a 69-year-old man, in whom the presence of multiple punctate lesions spread throughout the skeleton was discovered after an accidental fall with a fracture of the T11 vertebral body complicated by acute osteomyelitis. The importance of this clinical case lies in the need to rule out neoplastic cause after the vertebral fracture, since osteopoikilosis is usually an incidental finding and the specific characteristics of the radiological image would avoid unnecessary interventions.
1 INTRODUCTION
Sclerotic bone lesions can be the result of multiple etiologies, describing blastic bone metastases, vascular disorders, congenital disorders, infectious and traumatic processes, and endocrinological alterations, with which a differential diagnosis must be made.
Osteopoikilosis is a congenital bone disease of autosomal dominant transmission, which leads to an alteration in the maturation of the endochondral bone, diagnosed incidentally due to its vague symptoms and characteristic radiological findings.1, 3, 4
We present the case of a patient who, after an accidental fall and due to acute back pain, underwent a radiological battery in which bilateral and symmetrical osteosclerotic lesions were evident, characteristics of this disease as an incidental finding. The most important differential diagnosis of these lesions is osteoblastic metastases, especially if they are asymmetric lesions or appear in patients over 50 years of age, more frequently in relation to breast or prostate carcinomas. Consequently, it is essential to take a good history and physical examination and correctly interpret the radiological signs, because osteopoikilosis is a benign disease that only requires analgesic treatment if there is pain, while the rest of the differential diagnosis requires more aggressive measures and can compromise life of the patient. In the literature, some complications of this bone dysplasia have been described, such as the development of osteosarcomas, giant cell tumors or chondrosarcomas, but it is not possible to conclude the causal link due to the small number of cases. However, it has been agreed that control and monitoring of injuries should be carried out.5
The rarity of our clinical case lies in the fact that the patient not only presents bone lesions compatible with osteopoikilosis, but also associates an acute fracture-crush of a dorsal vertebral body after a low-energy trauma, associating spondylodiscitis possibly due to hematogenous transmission and suspected tumor infiltration.
2 CASE HISTORY
2.1 Personal and sociodemographic history and chronic pharmacotherapy
A 69-year-old male, of Belgian origin, who has resided on the island of Tenerife, Spain, for 2 years, with little social support. He lives with a friend in a rental apartment in the south of the island, without first- or second-degree relatives and with a medium-low socioeconomic level. He has no known drug allergies, he is hypertensive, dyslipidaemia and type 2 diabetic for more than 5 years, on treatment with ramipril 10 mg daily, simvastatin 20 mg daily and metformin/dapagliflozin 1000/5 mg every 12 h. He uses night-time CPAP for moderate OSAHS (obstructive sleep apnea–hypopnea syndrome), he is not a smoker, but he recognizes risky alcohol consumption (30–35 g of alcohol/day).
No other relevant medical data or disease history from his country of birth was available, nor was he followed up by primary care medicine since his migration to Spain.
2.2 Current illness and physical examination
The week before his consultation, he had an accidental fall on a public road; since then, back pain that makes mobilization impossible with no response to conventional analgesia, bedridden, abandonment of hygiene due to lack of care. He is brought to the Emergency Department on Basic Life Support with deterioration in level of consciousness, respiratory distress, dehydration, and pressure ulcers in both trochanters and right shoulder.
Poor general condition in the first evaluation, with tachypnea at 28 rpm, tachycardia 110 bpm, BP 115/75 mmHg, without fever. Skin-mucosal pallor, dehydrated with positive fold sign, without IY at 45°. Grade 2 pressure ulcers, without exudate, in the trochanters and right shoulder, hematomas on both thighs and in the lumbar area, superficial and resolving. Glasgow Coma Scale 15/15 with preserved temporal–spatial orientation, without gross neurological focal deficits, except for drowsiness. On cardiopulmonary auscultation, regular heart sounds, without murmurs, with preserved vesicular murmur, with scattered bilateral rhonchi, crackles at the right lung base. The abdominal examination was unremarkable and there was no peripheral edema.
2.3 Supplementary tests
Basic blood tests were performed, which showed elevated muscle enzymes (CPK 17,522 U/L, myoglobin 12,415 U/L), glomerular filtration rate 59 mL/min, creatinine 0.98 mg/dL, with normal liver function tests, sodium 160 mmol/L, rest of ions normal, with plasma osmolarity 337 mOsm/L and elevated acute phase reactants (leucocytosis 14,500/mm3 at the expense of neutrophilia, CRP 17.53 mg/dL), hemoglobin 11.9 g/dL with VCM normal and D-Dimer 2500 ng/mL. The analysis suggested rhabdomyolysis in the context of the fall and prostration, with hypernatremic dehydration and signs of secondary infection/inflammation.
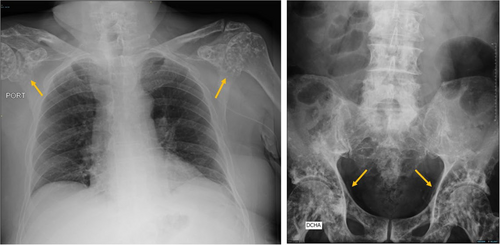
The arterial blood gas analysis showed respiratory alkalosis, sinus tachycardia at 110 bpm with S1Q3 pattern on the electrocardiogram, and the simple chest x-ray showed consolidation with air bronchogram in the right lower lobe. A CT scan of the pulmonary arteries was performed, given the tachypnea, sinus tachycardia, respiratory alkalosis, and elevated D-Dimer in a patient who was bedridden for more than 3 days, which confirmed pulmonary thromboembolism of the lobar and segmental branches of LSD, LID, and LII, and signs of hypertension. secondary pulmonary disease, without evidence of overload of the right heart chambers. Internal twin DVT was evident in both lower extremities on limb Doppler ultrasound. The dorso-lumbar spine x-ray showed a crush fracture of the T11 vertebral body, as well as patchy sclerotic bone lesions in the pelvis, humeri and femurs, predominantly proximal.
3 EVOLUTION
The patient is admitted to the Internal Medicine Service. Peripheral blood cultures were taken due to fever peaks and antibiotic therapy was started with amoxicillin-clavulanic acid 1 g/8 h and bronchodilators as treatment for community-acquired pneumonia. Low molecular weight heparin was also prescribed at an anticoagulant dose adjusted to weight given the thromboembolic disease, hydration with serum therapy with glucose at 125 mL/h due to hypernatremic dehydration, first and second step analgesia, vitamin complex, and other support measures.
He continued to be febrile during the first 48 h of admission with a fluctuating level of consciousness, with no other neurological symptoms. A CT scan of the head was performed, showing cortico-subcortical atrophy and punctate and nodular blast lesions in C1, and occipital condyles. A lumbar puncture was performed, which showed proteinorrachia, with normal glucorrhachia, without cell count and with a negative microbiological analysis. The study was expanded with MRI of the spine in which a traumatic lesion in the T11 vertebral body was described, with atypical evolution, possible osteomyelitis with anterior paraspinal extension on vertebral osteonecrosis. Positive blood culture was received for Staphylococcus hominis (2 series) and Candida glabrata, escalating antibiotic coverage to piperacillin-tazobactam, daptomycin, and anidulafungin as directed treatment, which was maintained for 14 days, with improvement in symptoms, disappearance of fever and decrease in acute phase reactants. Transthoracic echocardiography, ophthalmological examination, serial control blood cultures, and chest-abdomen CT did not yield other relevant findings.
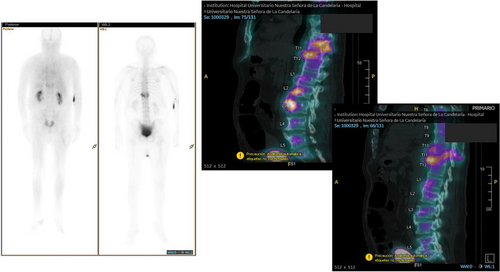
Regarding the bone lesions, the patient did not give consent to perform a spinal biopsy. It showed a slight elevation of bone alkaline phosphatase (155 IU/L) with normal phosphocalcium metabolism, ESR, free PSA and proteinogram. No evidence of neoplasia was found in the imaging studies performed. The bone lesions were sclerotic, patchy, nodular or oval, well defined, and affected the metaphysis and epiphyses of long bones, pelvis, calvaria, and vertebral column. A study was completed with bone SPECT/CT scintigraphy in which no tracer deposit was evident, with a more probable diagnosis of osteopoikilosis or spotted bone disease (Figures 1-3).

The evolution was favorable. He was referred to a mid-stay center for continuity of care, functional motor rehabilitation and continuation of oral antibiotic therapy with cotrimoxazole 160/800 mg every 12 hours and rifampicin 600 mg daily for a minimum of 6 weeks, as empirical treatment of spondylodiscitis, although guided by microbiology in peripheral blood cultures, persisting without fever, with negative acute phase reactants and without axial pain to date.
4 DIAGNOSIS
- Acute osteomyelitis with anterior paraspinal extension on vertebral osteonecrosis at T11 in a patient with disseminated sclerotic bone lesions compatible with osteopoikilosis.
- Bacteremia due to S. hominis and candidemia due to C. glabrata.
- Community-acquired right lower lobe pneumonia, FINE IV. Possible bronchoaspiration component due to impaired level of consciousness.
- Bilateral pulmonary thromboembolism of lobar and segmental branches in LSD, LID, and LII, low-risk/PESI I, without signs of overload of the right heart chambers.
- Deep vein thrombosis in the internal calves of both lower extremities.
- Moderate, hyperosmolar hypernatremia, with decreased ECV, in relation to volume depletion due to low intake.
- Rhabdomyolysis secondary to trauma since discharge, and grade 2 pressure ulcers in relation to falls and prolonged bed rest.
5 DISCUSSION
Osteopoikilosis, also known as disseminated condensing osteopathy or spotted bone disease, is a rare bone disorder classified as an autosomal dominant osteosclerotic dysplasia associated with heterogeneous mutations in the LEMD3 gene, which involves alterations in the bone maturation process. Three forms of the disease have been described: mottled type, striated type, and mixed type.1, 3, 2
It is a benign disease, asymptomatic in most cases, of incidental diagnosis. It presents with sclerotic, oval, multiple, well-defined and symmetrical lesions. Characteristically, the lesions remain for life, with a periarticular distribution, affecting, according to case series, in order of frequency from highest to lowest, the phalanges, carpal and metacarpal bones, pelvis, femur, radius, sacrum, humerus, tibia, and ball joint. Involvement of the epiphysis and metaphysis of long bones is common.1, 3, 4
An association has been described with other disorders such as scleroderma, endocrinological diseases, rheumatoid arthritis, syndactyly and cleft palate, and with syndromes such as Buscke–Ollendorf and Klippel–Feil. The differential diagnosis of this disease includes osteoblastic metastases, primary bone tumor, mastocytosis, tuberous sclerosis, synovial chondromatosis, striated osteopathy, and melorheostosis.1, 6
Complementary tests are usually normal, including bone scintigraphy with Tc99m6, although cases of osteopoikilosis with pathological findings by bone scintigraphy have been reported and, if there are symptoms, joint pain is the most common and generally responds to treatment with non-steroidal anti-inflammatory drugs.1, 3
The patient in our clinical case did not know the diagnosis nor did he have a history of bone diseases in his family, and except for diabetes mellitus, no other associated disorders were found. The complexity of this clinical case lies in the concurrence of osteoblastic lesions characteristic of osteopoikilia with an acute fracture crush of a dorsal vertebra and an infectious process on it, which requires exhaustively ruling out the presence of bone metastasis; therefore, the main differential diagnosis of this disease.
AUTHOR CONTRIBUTIONS
Tejera-Pérez Rosa Juana: Conceptualization; formal analysis; investigation; supervision; writing – original draft. Aguilar-López Ana: Conceptualization; formal analysis; investigation. Marfil-Daza Julia: Conceptualization; formal analysis; investigation. Castaño-Pérez Sara: Conceptualization; formal analysis; investigation.
ACKNOWLEDGMENTS
The authors have nothing to report.
FUNDING INFORMATION
This article did not receive any grants.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
ETHICS STATEMENT
None.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




