An unusual presentation of craniopharyngioma in an adult with nasal bloackade
Key Clinical Message
Early biopsy and multidisciplinary collaboration with imaging and physical examination are crucial for the diagnosis of such rare tumor presenations. Highlighting the importance of maintaining a broad differential for intra-nasal lesions given the rare presentation of craniopharyngioma as nasal mass.
1 INTRODUCTION
Craniopharyngiomas are classified as WHO grade 1 tumors of dysodontogenic origin that demonstrate distinct, circumscribed growth patterns and histological characteristics reflecting benignity despite exhibiting malignant behavior.1
2 CLINICAL PRESENTATION
We present a case of a 31-year-old man, who presented to the ENT outpatient department with complaints of nasal blockade and thick B/L nasal discharge since 3 months. The patient had concomitant headaches alleviated with analgesics. The patient had no history of epistaxis or any allergies, no complaints of any associated visual disturbances nor any features indicative of pituitary dysfunction. Patient has no relevant family history or contributing occupation history. General physical examination and systemic examination were normal and unrevealing.
Examination of the nasal cavity revealed a friable, polypoidal mass toward the end of the posterior nasal septum. There was some amount of discharge present around the mass as well.
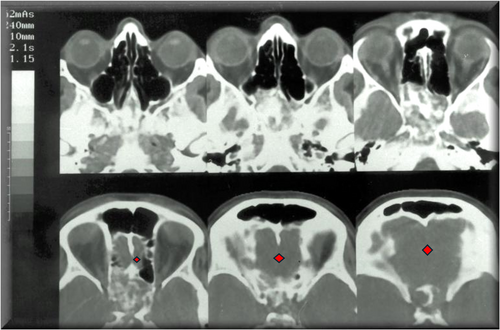
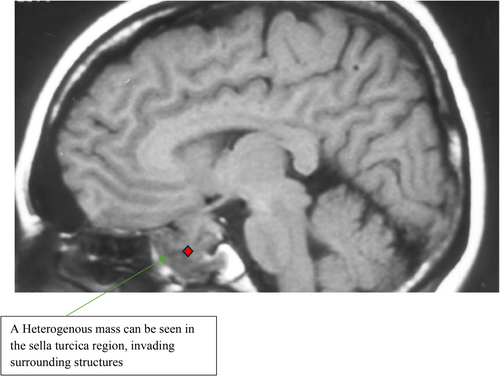
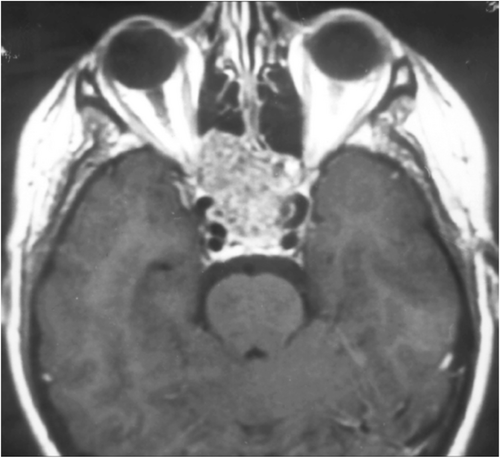
The patient underwent routine labs, revealing a normal blood count, no presence of inflammatory markers. Patient had a normal fundoscopy. CT scan of paranasal sinuses revealed an ill-defined, heterogeneously enhancing mass in the posterior nasal cavity invading into the sinuses, choanal, sellar, and parasellar regions (Figure 1). The patient initially denied pre-op MRI due to concerns for claustrophobia but eventually ended up getting it (Figures 2,3).
Given the nature of local spread of the mass, presence of thick, slightly bloody discharge, and associated friable appearance; the possible differentials were;
Clivus chordoma (the mass wasn't hard), esthesioneuroblastoma (patient had no decreased sense of olfaction), Basaloid type of squamous cell carcinoma, and craniopharyngioma were the two debatable provisional diagnosis which demanded the need for a pathological diagnosis.
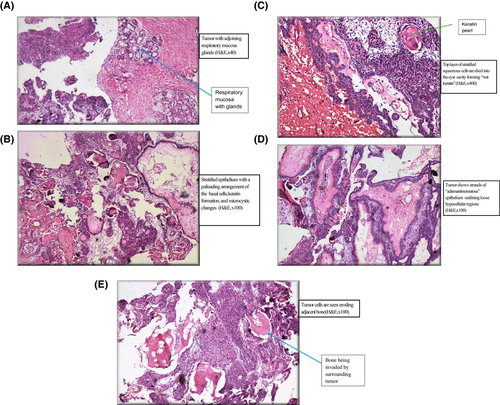
Patient was subsequently admitted and underwent endoscopy-guided punch-biopsy of the lesion and surrounding area, which after pathological assessment, was found to be a craniopharyngioma (Figure 4 A–E). Following the diagnosis, the patient was taken up for endoscopic sinus surgery for removal of the tumor from the posterior ethmoid and trans-sphenoidal resection of the tumor from the sphenoid sinus. The post-op status of the patient was uneventful with eventual loss of follow up.
3 DISCUSSION
This case brings forth a rather rare presentation of a craniopharyngioma, as a nasal mass presenting with nasal discharge and nasal blockade.
The rarity of craniopharyngiomas presenting as nasal masses stems from their embryological origin and typical patterns of growth. Craniopharyngiomas arise from remnants of the craniopharyngeal duct. As such, these tumors most commonly develop within the sella turcica and suprasellar region of the skull base. Their growth patterns tend to be primarily intra-cranial, with local invasion into surrounding structures like the optic chiasm, hypothalamus, and third ventricle. Extension inferiorly into the nasal cavity and paranasal sinuses is decidedly uncommon, as the tumor must traverse through the sphenoid sinus and break through the skull base to reach these areas. This unusual route of spread likely accounts for the paucity of reported cases presenting as nasal masses, making our case particularly noteworthy and educational. Due to it is high propensity to recur, pathologists must demonstrate high degree of suspicion for early diagnosis.2
Certain similar differentials that could be mimicked by a primary CNS tumor with secondary downward extension and associated local destruction (like craniopharyngioma) could include clivus chordomas and esthesioneuroblastomas, both of which were ruled out clinically due to the absence of a hard mass or altered sense of smell, respectively. A potential differential of basaloid type of squamous cell carcinoma was ruled out after craniopharyngioma was further confirmed on biopsy.
Though imaging and physical findings do aid provide crucial insights into the anatomy, location, extent and presentation craniopharyngiomas, reliance on imaging alone would lead to misdiagnosis of the condition due to overlapping radiological features among different lesions. Therefore, we emphasize on a tissue/pathological diagnosis which can easily confirm the diagnosis of such an entity and can be followed directly by the required management.3
With only around 50 or so cases of craniopharyngioma reported with known infrasellar extension; our case brings out the rarity and the clinical duplicity of such a lesion, especially it presenting as a friable, nasal polyp, putting into consideration how a strong clinical acumen even with paucity of literature can aid in the diagnosis of this condition.
4 CONCLUSION
Despite the rarity of brain tumors invading the nasal cavity, this report underscores the crucial clinical lesson of maintaining a broad differential diagnosis for nasal masses, including the possibility of extension from intracranial lesions. Heightened clinical suspicion and a multidisciplinary approach involving otolaryngologists, neurosurgeons, and pathologists are paramount in such unusual cases.
AUTHOR CONTRIBUTIONS
Jay Gohri: Conceptualization; data curation; formal analysis; project administration; resources; supervision; visualization; writing – original draft; writing – review and editing. Mayuri Chaurasia: Conceptualization; resources; visualization; writing – original draft. Varun Sheoran: Validation; visualization; writing – original draft; writing – review and editing. Vishal Kanwrani: Visualization; writing – original draft; writing – review and editing.
FUNDING INFORMATION
No external funds given.
CONFLICT OF INTEREST STATEMENT
No conflict of interest reported.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.




