Neutrophilic eccrine hidradenitis from granulocyte-stimulating factor in a patient with ANCA vasculitis
Key Clinical Message
Neutrophilic eccrine hidradenitis (NEH) is one of the cutaneous manifestations of chemotherapy side effects. However, it can arise from other non-chemotherapy medications. The granulocyte-colony-stimulating factor is a medication reported to trigger NEH.
1 CASE
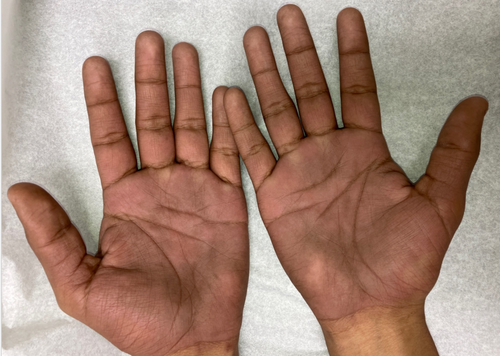
(A) A young adult Hispanic male with end-stage renal disease secondary to IgA nephropathy, hypertension, and p-antineutrophilic cytoplasmic antibody (ANCA) vasculitis presented to the clinic with skin discoloration on bilateral palms and soles for 2 weeks. (Figures 1 and 2) The itchiness and painful discoloration started 3–4 weeks ago on his left sole. A week later, it progressed to the other sole and both palms. The pain was reproducible with pressure to the affected area. He denies fever, malaise, or joint pain.

Three weeks before the development of the discoloration, he developed neutropenia secondary to mycophenolate mofetil (MMF) for the treatment of ANCA vasculitis requiring the administration of filgrastim 300 mcg subcutaneously daily for 10 days and MMF discontinuation. The last filgrastim dose was 10 days before the onset of discoloration.
Physical examination showed tender well-defined mild swelling erythematous-violaceous plaques on bilateral palms and soles. The complete blood count, ESR, and CRP levels were unremarkable. The differential diagnosis includes toxic acral erythema and contact dermatitis.
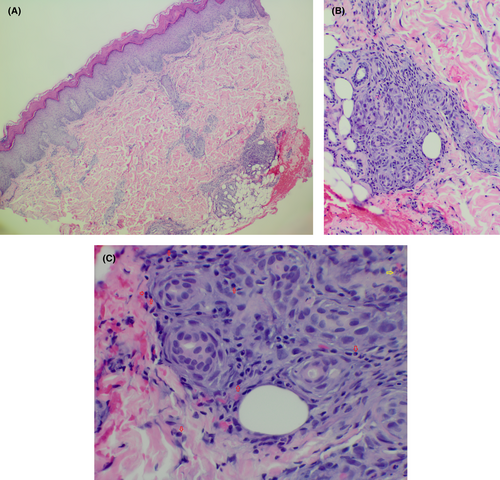
A skin biopsy of the left palm demonstrates squamous metaplasia of the eccrine ducts and a few neutrophils and eosinophils around the eccrine ducts consistent with neutrophilic eccrine hidradenitis. (Figure 3A–C).
The patient was treated with clobetasol ointment 0.05% twice daily for itchiness. He was advised that the discoloration would resolve on its own without treatment. At 10-week follow-up, the lesions have resolved.
2 DISCUSSION
NEH is a non-vasculitis neutrophilic dermatosis that develops 7–14 days after initiation of culprit agent.1 It has been reported to be associated with post-chemotherapy for lymphoma and solid tumors and granulocyte-colony-stimulating factor (GCS-F) administration.2 In patients receiving chemotherapy, the excretion of toxic components into eccrine sweat glands is thought to be the underlying pathogenesis of NEH.1, 2 They may exhibit fever, or neutropenia, especially in the setting of receiving chemotherapy.2 Typical presentations include tender erythematous papules macules and plaques on the trunk face or extremities.2
The definitive diagnosis requires a biopsy which typically reveals neutrophilic peri-eccrine infiltrates, neutrophilic infiltrates within eccrine apparatus, necrosis of eccrine, epithelium, and a squamous syringometaplasia.1, 2 However, it is important to note that NEH is more commonly seen during neutropenia compared to other neutrophilic dermatoses, thus neutrophilic infiltrates may be sparse or absent on histopathology.3 Dermatopathology in a young patient who received chemotherapy concomitantly with GCS-F and developed NEH showed sparse neutrophilic infiltrate despite normal to high white blood cell count.3
In our case, filgrastim, a GCS-F, could be the trigger within the suspected timeframe. Additional laboratory investigations including complete blood count are still crucial to exclude the presence of leukemia.
There is no specific and standard treatment for NEH as it is self-limited and resolves within several days to weeks. Corticosteroids are applicable to shorten the duration of the lesions and relieve the pain in some patients.1 Colchicine has been used successfully for treatment, and dapsone has been used for treating and preventing recurrences.1, 2 Administration of empiric antimicrobial therapy is appropriate in post-chemotherapy patients who present with NEH, fever, and neutropenia until infection is excluded.1
AUTHOR CONTRIBUTIONS
Nattanicha Chaisrimaneepan: Conceptualization; formal analysis; validation; visualization; writing – original draft. Sakditad Saowapa: Conceptualization; visualization; writing – review and editing. Watsachon Pangkanon: Conceptualization; writing – review and editing. Jerapas Thongpiya: Formal analysis; writing – review and editing. Pitchaporn Yingchoncharoen: Resources; writing – review and editing. Natchaya Polpichai: Validation; writing – review and editing. Pharit Siladech: Project administration; resources; validation.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
No funding was received.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
The data is available for sharing.




