Rapidly progressing pediatric Lupus with Diffuse Alveolar Hemorrhage and CNS involvement
Abstract
Key Clinical Message
Systemic Lupus Erythematosus (SLE) can have an insidious onset and a fatal prognosis in children. Patients presenting without typical signs of SLE should undergo further evaluation if they are not responding to the initial diagnosis and treatment. This is especially true for patients with rapidly progressing symptoms and deterioration in spite of treatment.
Pediatric Systemic Lupus Erythematosus is a chronic autoimmune disorder with various organ involvement pulmonary involvement in the course of this disorder is a rare yet potentially life-threatening complication. In this case report we highlight the findings of a 16-year-old girl acutely and initially presenting with cough and fever, eventually complicating to diffuse alveolar hemorrhage and gradual loss of consciousness. Although the patient was started on immunosuppressive treatment after the diagnosis of lupus, based on renal and hematological impairment, was made and initially responded, she eventually deteriorated.
1 INTRODUCTION
Pediatric lupus, also known as Systemic Lupus Erythematosus (SLE), is a chronic autoimmune disorder characterized by various clinical manifestations and multisystem involvement. Referred to as Childhood-Onset SLE, typically occurs around the ages of 11 and 12 years, with a higher incidence in females.1, 2 Common clinical manifestations include malar rash, photosensitivity, arthritis, hematologic abnormalities, renal involvement, and vasculitis.1 Despite its lower prevalence in children than in adults, pediatric lupus, especially in those under 5 years old, is associated with significant morbidity and mortality, particularly when vital organs like the brain and lungs are affected.1, 2 Lung involvement in pediatric lupus can present as pleuritis, interstitial lung disease, pulmonary embolism, pulmonary hypertension, acute lupus pneumonitis, and pulmonary hemorrhage.3 Neuropsychiatric involvement, including lupus cerebritis, is observed in up to 75% of pediatric cases, with 30% to 70% presenting with two or more signs or symptoms.4, 5 Although signs of CNS involvement are diverse and can include seizures, chorea, impaired deep tendon reflexes, cranial nerve involvement, and aseptic meningitis, the most prevalent and common initial symptom are headaches.4, 5 This case report outlines the findings of a young girl who, after initially presenting with fever, dyspnea, and cough, rapidly progressed to developing pulmonary hemorrhage. Subsequent testing led to a diagnosis of SLE, along with pulmonary, hematological, neurological, and renal involvement, despite the absence of typical lupus manifestations.
2 CASE HISTORY/EXAMINATION
A 16-year-old female presented at the emergency department with a three-week history of persistent fever, cough, and shortness of breath. She also reported recent weight loss of about 3 kg, weakness, and fatigue during this time. The patient had no significant past medical history, and family history was devoid of any unusual diagnoses. On admission, respiratory rate (RR) was around 22–24, O2 saturation was around 92%, and temperature was 38.3°C, while blood pressure (BP) and heart rate (HR) were within the normal range.
3 METHODS (DIFFERENTIAL DIAGNOSIS, INVESTIGATIONS, AND TREATMENT)
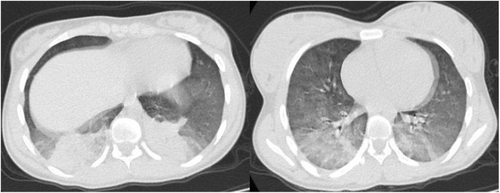
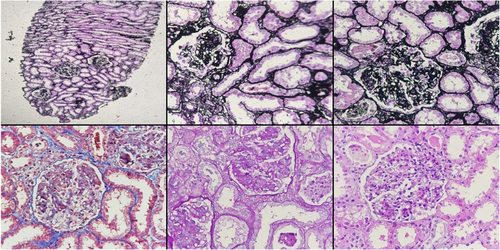
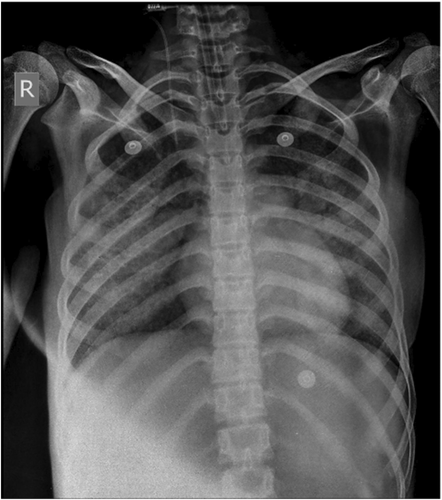
Lung sounds were diminished in bases of both lungs, with chest CT revealed consolidation in the posterior base of both lungs, suggesting bacterial pneumonia, for which antibiotic treatment was initiated (Figure 1). However, her condition did not adequately improve, and subsequent tests for COVID-19, influenza, and tuberculosis were all negative. During this time, she experienced a progressive decline in hemoglobin levels, which was diagnosed as hemolytic anemia when proteinuria and hematuria were detected in urine analysis (UA), and further examinations, including bone marrow biopsy and aspiration, showed no significant abnormalities. Despite the absence of skin lesions or signs of arthritis, along with normal echocardiography and abdominopelvic ultrasound results, the possibility of a rheumatologic disorder was considered due to the multi-organ involvement. Markers, such as ANA, anti-cardiolipin antibodies, and anti-dsDNA, were found to be positive, along with a notable reduction in C3, C4, and CH50 levels. Subsequently, a kidney biopsy revealed Diffuse Proliferative Glomerulonephritis (ISN/RPS class IV-G (A/C)) (Figure 2), confirming the diagnosis of lupus nephritis. The patient received Intravenous Immunoglobulin (IVIg at 2 g/kg), as well as pulses of Methylprednisolone, for 3 days. Treatment with hydroxychloroquine (5 mg/kg/day), mycophenolate mofetil (600 mg/m2 twice a day), Prednisolone (1 mg/kg/day), and aspirin was also initiated. Following the treatment, the patient's respiratory symptoms and fever completely resolved, and she was discharged shortly thereafter. However, she returned 6 days later with hemoptysis and a recurrence of the previous symptoms, with tests showing a further decrease in hemoglobin with an increase in creatinine levels (2.08 mg/dL), and imaging showing diffuse pulmonary infiltration consistent with diffuse alveolar hemorrhage (Figure 3). Similar to the first admission, HR and BP were normal, while O2 saturation and RR were around 90% and 24%, respectively. This time, the patient was treated with pulses of Cyclophosphamide and Methylprednisolone for 2 days until creatinine levels normalized and respiratory symptoms resolved. Upon discharge, the patient continued to receive hydroxychloroquine, mycophenolate mofetil, and high-dose prednisolone. She returned a month later, this time with new onset tremor and lower extremity weakness, hinting at CNS involvement. Unlike the past two admission, the patient had normal O2 saturation and RR, while BP fell below 90 mmHg and HR was elevated to around 120 bpm. Physical examination showed gross tremor in both hands, slightly reduced deep tendon reflexes, normal plantar reflexes, and muscle force was graded 4/5. No cranial neuropathy and sensory deficits were noted, and pupils were mid-sized and reactive to light. Labs showed only pancytopenia (Table 1) and elevated Ferritin levels (1500 ng/mL), with a normal peripheral blood smear (PBS).
| Labs | Admission | Reference range | ||
|---|---|---|---|---|
| First | Second | Third | ||
|
WBC (×109/L) Hb (g/dL) Plt (/mcL) Retic (%) |
5.35 6.5 228 8 |
11.3 7.8 302 1.2 |
2.4 6.1 42 - |
4.5–11 11.5–15 150–400 <1% |
|
ESR (mm/h) CRP (mg/dL) Uric acid (mg/dL) |
93 5.4 5.4 |
90 5.8 4.5 |
82 41 3.5 |
<10 <1 2.5–6 |
|
AST (U/L) ALT (U/L) LDH (U/L) |
40 38 1417 |
46 16 4002 |
257 99 2140 |
<40 <45 140–280 |
|
Alb (g/dL) Ferritin (ng/mL) Creatinine (mg/dL) |
3.2 - 0.8 |
3.4 470 2.08 |
2.5 1500 1.2 |
3.5–5.5 12–150 0.5–1.1 |
|
U/A blood U/A protein U/A WBC U/A RBC |
3+ 4+ Many Many |
3+ 3+ Many 4–6 |
1+ 1+ 3–4 1–2 |
- - - - |
|
Anti-nuclear antibody (ANA) Anti-dsDNA antibody Anti-cardiolipin IgM Anti-cardiolipin IgG |
Pos (>250) Pos (>100) Pos (16.1) Pos (14) |
- - - - |
- - - - |
Positive >55 Positive >40 Positive >12 Positive >12 |
|
Anti-phospholipid IgM Anti-phospholipid IgG C3 (mg/dL) C4 (mg/dL) |
Neg (3.5) Neg (2.6) 23 5 |
- - - - |
- - - - |
Positive >10 Positive >10 89–187 10–40 |
|
p-ANCA c-ANCA |
2.5 6.3 |
- - |
- - |
Positive >20 Positive >20 |
- Abbreviations: Neg, negative; Pos, positive.
4 CONCLUSION AND RESULTS (OUTCOME AND FOLLOW-UP)
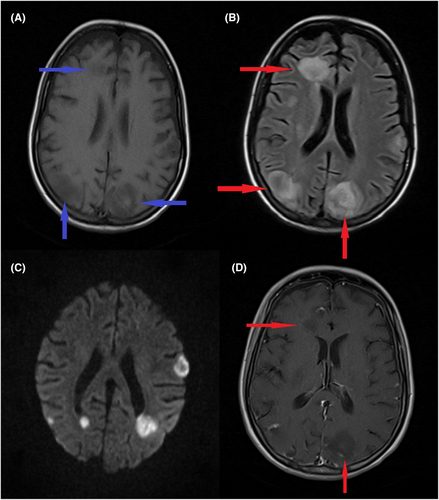
The possibility of macrophage activation syndrome (MAS), CNS vasculitis, and thrombotic thrombocytopenic purpura (TTP) was considered, for which she received cyclosporine, dexamethasone, cyclophosphamide (IV at a dose of 0.5 g/m2) and Methylprednisolone, this time in addition to IVIg for 5 days. Unfortunately, her condition gradually worsened during her hospital stay and she eventually lost consciousness, for which a brain MRI was performed (Figure 4), which showed multiple white matter lesions with extension into the gray matter. Due to a lack of improvement plasmapheresis was considered, however the patient went into cardiac arrest before treatment could be commenced. CPR was initiated, unfortunately all attempts at resuscitation were unsuccessful and the patient eventually expired, potentially due to disseminated intravascular coagulation. This was potentially a result of a cytokine storm and subsequent macrophage activating syndrome, and not due to any infections.
5 DISCUSSION
Childhood-Onset SLE, also known as pediatric lupus, is a chronic connective tissue disease that can affect multiple organs. Although the patient in this report did not display the standard hallmarks of SLE; including a malar rash and arthritis, she did have pulmonary, neurological, and renal involvement in the form of diffuse proliferative glomerulonephritis alongside diffuse alveolar hemorrhage. Despite having a lower prevalence in children than adults, lupus is associated with significant morbidity and mortality, especially when it affects vital organs like the brain and lungs.4, 6 Headaches, seizures, tremors, muscle weakness, cognitive decline, and aseptic meningitis are a few neurological symptoms that can appear when the CNS is involved in pediatric lupus.7 Involvement of the CNS can also cause a gradual loss of consciousness, especially if other organ dysfunction is present.1, 4, 7 Although the pathogenesis of CNS lupus is not fully understood, autoantibodies and immune complex deposition are thought to play a crucial role in the emergence of neurologic manifestations.4, 5, 7 Since the initial symptoms and signs of CNS lupus can be subtle and easily confused with those of other neurological dysfunctional causes, concurrent manifestation of other lupus related signs and symptoms is generally necessary for the diagnosis. Although headaches are the most prevalent initial symptom of CNS involvement in SLE cases, only new onset tremor and muscular weakness were noted in the patient prior to losing consciousness. A potentially fatal side effect of pediatric lupus is diffuse alveolar hemorrhage (DAH), which is characterized with dyspnea, hemoptysis, and a drop in hemoglobin levels.8 In cases of lupus DAH, radiographic evidence of bilateral infiltrates on chest X-ray or computed tomography (CT) scan is frequently present, and although the etiology is not well understood, it is thought to be similar to that of lupus nephritis being mainly immune complex-driven.8 In order to effectively treat DAH, immunosuppressive therapy and respiratory support must be started right away to address underlying inflammation and vasculitis.3, 8, 9 In this patient, bilateral base opacities in the lungs were initially treated as pneumonia, on account of the fever, dyspnea, and cough. Even though her symptoms alleviated with treatment, they recurred after less than a week, this time with hemoptysis and low hemoglobin levels, indicating DAH. Immunosuppressive treatment temporarily halted the progression of her disorder, but was ultimately unsuccessful.
Our case is similar to that of Asseri et al., in which a 13-year-old girl developed diffuse alveolar hemorrhage (DAH) as a complication of SLE and COVID-19 infection.10 Similar to our case, she was treated with Methylprednisolone and broad-spectrum antibiotics, and discharged with prednisolone, hydroxychloroquine, and azathioprine. Unlike our patient, she received 6 sessions of Plasmapheresis resulting in significant clinical improvement. Another case by Kimura et al., reported a 14-year-old girl who was placed in extracorporeal membrane oxygenation (ECMO), and later treated with pulmonary lobectomy in addition to methylprednisolone, cyclophosphamide, IVIg, and plasmapheresis, again with significant clinical improvement.11 Studies have shown the efficacy of methylprednisolone and cyclophosphamide as initial therapies in DAH; however, both plasmapheresis and rituximab are potentially beneficial adjuvants.8, 12 Plasmapheresis has been initiated in patients with persistent and resistant DAH.8 However, some studies have failed to show that plasmapheresis improved overall survival rates. In our case, plasmapheresis was not initiated, however no conclusions can be made regarding its efficacy and potential survival of the patient had she received it.8, 12
This case report provides a thorough account of a 16-year-old female patient with pediatric lupus, exhibiting concurrent renal, brain, and lung involvement. The patient initially presented with a mild fever and cough, and developed hemolytic anemia and hematuria during her first admission with her symptoms alleviated with immunosuppressive therapy. Unfortunately, she eventually developed DAH and loss of consciousness. Despite early and high-dose treatment with immunosuppressants, the patient gradually deteriorated and eventually expired. This case report sheds light on the complex clinical presentation and management of pediatric lupus with simultaneous CNS and lung involvement, emphasizing the importance of a multidisciplinary approach in the care of these patients. Additionally, it underscores the rapid progression and potentially fatal characteristic of pediatric SLE.
AUTHOR CONTRIBUTIONS
Mahdieh Vahedi: Conceptualization; methodology; validation. Reza Nejad Shahrokh Abadi: Investigation; writing – original draft; writing – review and editing. Abdolreza Malek: Data curation; investigation; supervision; validation. Farrokh Seilanian Toosi: Conceptualization; formal analysis; project administration; resources; writing – review and editing. Maryam Naseri: Investigation; supervision. Narges Hashemi: Conceptualization; data curation; investigation; methodology; supervision; validation; writing – review and editing.
ACKNOWNLEDGMENTS
The authors would like to appreciate the Clinical Research Development Unit, Ghaem Hospital, Mashhad University of Medical Sciences, for their assistance.
FUNDING INFORMATION
The authors declare that there are no funding/financial sources or conflicts of interest relevant to this work.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest regarding the publication of this paper.
CONSENT
Written informed consent for the publication of this report was obtained from the patients by the corresponding author.
Open Research
DATA AVAILABILITY STATEMENT
Data supporting the conclusions of the study is all available free of cost through open access journals and websites.




