Radiofrequency ablation of osteoid osteoma at the base of the coracoid process: Report of two cases
Key Clinical Message
If you encounter an unexplained case of bone marrow edema in a young patient, consider the possibility of osteoid osteoma (OO). Even in the presence of a nidus near vital structures, RFA can safely be used to treat OO.
1 INTRODUCTION
Osteoid osteoma (OO) is a benign osteoblastic lesion that occurs primarily in young men and accounts for approximately 11% of all benign bone tumors.1 Almost 80% of all “OO” cases are detected in patients younger than 30 years old. These lesions are generally seen in the shaft of the long bones, especially the femur or tibia, in the lower limb. They are only rarely detected in the flat bones.2-5 “OO” includes a well-defined osteoblastic mass, known as a nidus, surrounded by the reactive bone sclerosis zone. Following nidus excision, the sclerosis zone gradually disappears, indicating a secondary, reversible alteration.6 Patients with OOs typically report generalized pain at the site of their benign tumors, and their pain can be more severe and frequent at night. Non-steroidal anti-inflammatory drugs (NSAID) and salicylates are commonly used to manage pain.7 Tumor location determines how the disease will progress, which is unpredictable and protracted. A misdiagnosis could result in bone widening, deformation, and even length discrepancy and angle deviation.8
A diagnosis of OO is usually based on plain radiography and a characteristic clinical presentation. It is recommended that plain radiography be performed as the first imaging modality to assess patients with bone pain.9 Computerized tomography (CT) is widely recognized as one of the most valuable imaging techniques for diagnosing and localizing OOs.10 Several authors have reported that CT can detect almost 100% of spinal OOs.11, 12 Furthermore, OO detection in hands and feet is 96.5%.13 In 19 patients with OO that had been pathologically proven before excision of the lesion, CT produced superior diagnostic accuracy in 63% of cases than magnetic resonance imaging (MRI) in diagnosing the OO nidus.14 In terms of detecting and characterizing OOs, MRI is inferior to CT.7 It is estimated that the misdiagnosis risk is 35% when used as the primary imaging modality.9 However, MRI may prove helpful in certain cases when it indicates cortical involvement as well as intramedullary and soft tissue spread. Additionally, it is excellent for demonstrating nidus in intra articular lesions.15 Due to high histopathological variability, the standard biopsy for suspected OO is controversial.16, 17 The need for histopathological confirmation does not always exist for diagnosis. Numerous analyses have failed to confirm the diagnosis.16, 18
It is extremely rare for OO to occur in the scapula, especially in the coracoid process (CP), therefore it is not commonly recognized as a differential diagnosis in young people with shoulder pain.19 Various therapeutic approaches have been proposed for treating these lesions, including complete surgical excision and percutaneous radiofrequency ablation (RFA).20 Nevertheless, it is critical to note that the use of any of these treatment strategies may lead to permanent impairment of the articular cartilage or physics in younger patients.21 Herein, we present the first cases of OO at the CP base, treated successfully with RFA in the literature.
2 CASE DESCRIPTION
2.1 First case
A 13-year-old male without any history of medical illness presented to our department with a complaint of 1-year left shoulder pain. The patient described a constant ambiguous pain on the ventral surface of the shoulder, radiating to the left upper extremity. The ache was more severe at night and during physical activities and responded partially to anti-inflammatory drugs. Approximately a year ago, he reported a history of falling on his left shoulder which was assumed to be the cause of the pain.
2.2 Second case
A 20-year-old man presented to our department with a complaint of chronic right shoulder pain. The pain was more severe at night and the shoulder's range of motion was limited due to pain. He had been treated with physiotherapy and painkillers during this period which were not able to subside the symptoms completely.
3 METHODS
3.1 First case
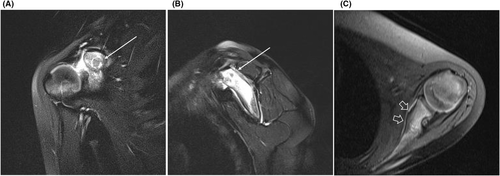
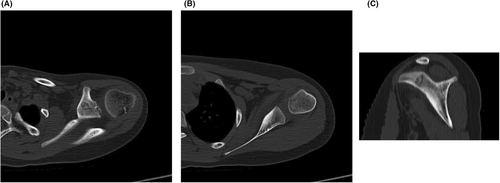
During this period, a non-contrast MRI had been ordered to search for any soft tissue abnormalities since the initial X-rays turned out to be normal. The first MRI revealed the presence of bone marrow edema at the scapula, glenoid, and CP associated with glenohumeral joint effusion. In light of the MRI findings, bone marrow edema was interpreted as traumatic, and further investigations were not conducted. Despite the conservative treatment, the pain continued to exist and increased gradually in severity. After about 1 year, during the physical examination in our department, mild pain sensation was noted around the CP. However, no tenderness or restriction in the range of motion of the shoulder was detected and the muscle strength was normal. Inflammatory markers were also checked and revealed no signs of inflammation. After that, the patient underwent a repeat MRI which revealed extensive bone marrow edema at the scapula, glenoid, and CP together with glenohumeral joint effusion without any changes when compared to the previous MRI (Figure 1). Cortical thickening was noted along the anterior aspect of the scapula. A 7 mm low signal intensity focus with surrounding edema and low signal intensity rim was noticed at the base of the CP which raised the probability of an underlying lesion (Figure 2). Given the gender and age of the patient with the duration and the pattern of symptoms, “OO” was suspected. A spiral CT scan was recommended to identify the nidus. The spiral CT scan nicely demonstrated the nidus of OO as a well-defined lytic lesion with reactive sclerosis around the edges and central calcification at the base of the CP which was responsible for the apparent hypointense focus in MRI images. The solid periosteal reaction was also detectable at CT scan along the anterior margin of the scapula. Considering the clinical status of the patient along with the size and location of OO, after consultations with our interventional radiologists and orthopedic surgeons, RFA was suggested for this case. The patient's parents gave their written informed consent for RFA after they were provided with thorough information on the therapeutic options available along with the medical team's preferred method. After preparation, the patient was placed face down on the CT scan machine table. First, a CT scan was performed to localize the nidus. Caution was made to avoid the brachial plexus during the procedure from the posterolateral approach which passes beneath the CP. After marking the point of insertion on the skin, sterilization was applied. After deep sedation, a small incision was made in the skin, Jamshidi biopsy needle (11 gauge) was introduced to the cortex until it reached the nidus under CT guidance. Afterward, an RF needle (10 mm active RF needle, Cosman RF system) was inserted through the cannula (cannula 101020) into the nidus. The needle was then heated to 60°C for 1 min, followed by heating to 90°C for 7 min to achieve thermal ablation. The RF electrode was removed and sterile dressings were applied. The procedure took about half an hour.
3.2 Second case
Non-contrast MRI was ordered to search for any detectable abnormality. MRI revealed bone marrow edema in the scapula and CP (Figure 3A,B). Reviewing the MRI images results the clinician suspected a primary tumoral process in the scapula. He referred the patient to the radiology interventionist for biopsy utilizing CT guidance. Before any invasive procedure, the interventionist ordered a CT scan. This revealed the nidus of the OO at the base of the CP, the culprit for bone marrow edema (Figure 3C). Provided with thorough information on the therapeutic options available along with the medical team's preferred method the patient opted for RFA and his written informed consent for RFA was obtained. After about half an hour, the procedure was completed. The RFA protocol was similar to the first patient. (Figure 4).


4 CONCLUSION AND RESULTS
Our reports describe two cases with delayed diagnosis of OO at the coracoid base. It is our pleasure to report the first two cases of OO based on the CP that were successfully treated with RFA. After ablation, the patients were discharged on the same day and followed up at 1, 6, and 12 months. Their conditions were symptom-free and they did not experience any complications.
5 DISCUSSION
The CP is an exceptional and remarkably uncommon site for OOs.3 OO is typically characterized by a nonspecific pain sensation that worsens at night and responds favorably to NSAIDs.22 When OO is located in the scapula, pain severity and distribution may vary, leading to the suspicion of numerous shoulder diseases, whereas this benign osteogenic tumor is infrequently taken into consideration.4 Therefore, misdiagnoses and delays in diagnosis are common in OO cases of CP. In one of our cases, the shoulder pain was assumed to be traumatic, as the patient's history and MRI findings demonstrated. The other patient had received unsuccessful conservative treatment long before the diagnosis of OO was made. The diagnosis of OO of the base of CP was made after about 1 year from the onset of symptoms with further investigations. CP bone tumors may be challenging to detect on plain radiographs. To exclude the likelihood of a bone lesion in a patient with persistent shoulder pain that is not relieved by the chosen treatment, additional imaging examinations may be undertaken.23 A radiograph taken from the axilla can help visualize the CP and spot any lesions at its base. Owing to their superior sensitivity, CT and MRI are preferred for CP lesions. CT scans may require thin sections to detect the nidus. MRI is generally considered less useful for identifying nidus than CT scans. However, it is useful for distinguishing OO from malignant tumors and osteomyelitis.24 A Technetium-99 bone scan is also sensitive but not specific.25 Various strategies have been employed in the treatment of OO, ranging from open surgical procedures to scarcely applied conservative management using anti-inflammatory drugs and minimally invasive percutaneous therapies.19 The selection of a therapeutic method is influenced by various aspects, with anatomical localization being a crucial consideration in the decision-making process. Hence, it is imperative to carefully evaluate and choose the most suitable therapy technique for each patient on an individual basis.19 In surgical approaches, the total removal of the core part is the most preferred method. Both of the two excision techniques proposed by Campanacci involved wide removal of the entire area or gradual removal of the overlying extra bone followed by scraping.26 It is recommended to unroof and curettage a lesion that is located in a critical area.26 In 2002, Kelly27 presented the initial report of applying arthroscopy as a therapeutic approach to resolving an OO affecting the shoulder. It has been demonstrated that arthroscopic treatment of OO lesions in joints of the upper extremities is highly successful with minimal complications. Nevertheless, there exists a potential for inadequate removal in regions that are more challenging to reach using arthroscopic procedures.28 At present, RFA is regarded as the preferred mode of treatment due to its safety and efficacy. It exhibits a high initial success rate of approximately 92%, and the rates of recurrence (ranging from 0% to 35%) and complications (3%) are low. The most prevalent complications of this method include thermal injuries to sensitive neurovascular structures close to the probe and skin burns.19 A minimal amount of bone is removed during RFA, allowing the patient to regain normal function quickly.29 Due to the medial passage of neurovascular structures to the CP and the penetration of the musculocutaneous nerve underneath the coracobrachial muscle,19 RFA application has been considered with substantial risk of causing damage to important anatomical structures in this area. In our cases, after consulting with our interventional radiologists and orthopedic surgeons, RFA was decided to be performed on these patients. Patients underwent RFA of their OO after obtaining informed consent. Thankful to the unique expertise of our interventional radiologist team, the operations went smoothly, and the patients were discharged the same day. They were soon back to their routine daily activities and were symptom-free without any restrictions during the 1-year follow-up.
AUTHOR CONTRIBUTIONS
Mohammad Reza Babaei: Conceptualization; methodology; validation; visualization. Esmaeil Gharepapagh: Supervision; writing – review and editing. Amir Honarmand Alamdari: Conceptualization; investigation. Javad Jalili: Writing – review and editing. Amin Mohammadi: Conceptualization; investigation. Mahsa Karbasi: Conceptualization; data curation; methodology; project administration; supervision; writing – original draft. Sahar Rezaei: Conceptualization; supervision; validation; visualization; writing – review and editing.
ACKNOWLEDGMENTS
None.
FUNDING INFORMATION
There is no funding or support for our article.
CONFLICT OF INTEREST STATEMENT
No author states to have any conflicts of interest.
CONSENT
Written informed consent was obtained from the patients to publish this report in accordance with the journal's patient consent policy.
Open Research
DATA AVAILABILITY STATEMENT
Detailed information is included in this article and if further explanation is required, please contact the corresponding author.




